Paramedic perceptions of conveying patients to an emergency department who were suitable for primary care: a cross-sectional survey
Belinda Delardes A B * , Meg Powell A , Kelly-Ann Bowles A , Samantha Chakraborty
A B * , Meg Powell A , Kelly-Ann Bowles A , Samantha Chakraborty  C D , Karen Smith A E and Alexander Olaussen A
C D , Karen Smith A E and Alexander Olaussen A
A
B
C
D
E
Abstract
Ambulance callouts and conveyances continue to increase disproportionately to population growth. This is largely driven by low- and medium-acuity patients who do not require ambulance management. We aimed to estimate the proportion of patients paramedics have conveyed to an emergency department (ED) via ambulance whom they considered suitable for primary care, and understand the barriers that contributed to these decisions.
A cross-sectional survey of registered paramedics in Victoria, Australia, was undertaken using an online questionnaire during 2022. Responses are presented using descriptive statistics, and logistic regression was used to identify associations between paramedic characteristics and barriers influencing primary care pathway referral.
A total of 367 responses were received. Of these, 70% of paramedics reported that at least half of the patients they conveyed to an ED were suitable for a primary care pathway. Paramedics reported high levels of confidence and support for primary care pathways in lieu of transport, however this had no correlation with their self-reported practice. The most common barrier to primary care pathway referral was limited access to a suitable primary care pathway (68%) followed by fear of an internal complaint, litigation or organisational pressure to convey patients to an ED (66%). Paramedics regarded themselves as more supportive of primary care pathway referral than those around them, including their peers, mentors, employers and university. They also reported that the COVID-19 pandemic had increased their personal support for primary care pathways, as well as organisational support from their employer, without corresponding increase in the broader medical and public communities. In fact, paramedics reported the COVID-19 pandemic had decreased support from the public and patients to refer patients to primary care pathways, and 57% of paramedics reported conveying a patient that had declined their primary care referral in the past week.
Paramedics frequently convey to an ED patients who they believe are appropriate for a primary care pathway. Paramedics face practical barriers such as a lack of available primary care providers and perceived lack of cultural support that contribute to this practice.
Keywords: ambulance, attitude to health, emergency medical services, general practice, health services accessibility, low-acuity, medical overuse, primary health care.
Introduction
Paramedics are increasingly attending patients with low- and medium-acuity conditions who do not require emergency management, which is disproportionate to population growth (Lowthian et al. 2011; Andrew et al. 2020). While use of an ambulance for non-emergent conditions has historically been labelled as ‘inappropriate’ (Richards and Ferrall 1999), contemporary research recognises that non-emergent patients contact ambulance services for advice and reassurance to restore their coping abilities following an unplanned deterioration in their health status (King et al. 2023; Lederman et al. 2023). The scope and education of paramedics has also changed over time, with a shift from paramedics as emergency service workers facilitating timely transport to definitive care, to paramedics being expert clinicians who are integrated within the broader healthcare system (Eaton et al. 2020). Despite this, there remains a trend of increasing ambulance conveyance of non-emergent patients to hospital emergency departments (EDs) suggesting there may be a mismatch between patient and paramedic perspectives of the role of the ambulance in non-emergent conditions.
Many patients requiring the reassurance and advice of paramedics will require follow-up in the community for further investigations and management, best provided by their general practitioner (GP). Most patients who are not conveyed to hospital following emergency ambulance response describe high levels of satisfaction (King et al. 2021), and in the Australian context, only 0.3% of patients had an adverse event occur within 48 h (Delardes et al. 2024). Ideally, this patient cohort would be referred to, and seen by, their GP within a timely manner, however limited GP availability is a known contributor to demand for ambulance services (Oosterwold et al. 2018). Paramedics describe knowing a patient is suitable for non-conveyance, however being unable to arrange primary care follow-up as aggravating and problematic (Lederman et al. 2023). This situation likely contributes to moral distress for paramedics, which is known to impact staff wellbeing and retention (Borhani et al. 2014; Campbell et al. 2018).
Non-conveyance rates in ambulance services are partially determined by the paramedic perception of risk aversion of senior management, and it is recognised that a ‘blame culture’, including the impact of complaints and defensive practices influences paramedics’ clinical practice (Kirk et al. 2018; Knowles et al. 2018). This further contributes to paramedics knowingly conveying patients who do not require ambulance services due to fear of reprisal (Oosterwold et al. 2018). Unnecessary ambulance conveyance to an ED to avoid complaints is an example of defensive practice, which has repercussions for both paramedic job satisfaction and patient care (Newton et al. 2020).
There is a growing body of qualitative evidence that discusses paramedic decision making regarding conveyance, however no research could be found that quantified the proportion of patients that would be suitable for alternate care. We aimed to estimate the proportion of patients paramedics have conveyed to an ED via ambulance whom they considered suitable for primary care and further understand the barriers that contributed to these decisions.
Methods
Study design
A cross-sectional survey of registered paramedics was undertaken using an online questionnaire. The questionnaire was developed by the authors who have expertise in paramedicine, general practice and emergency medicine. The questionnaire was piloted on a convenience sample of four paramedics for both readability and face validity, however no further validation occurred. The questionnaire included sections relating to the proportion of patients appropriate for primary care management, the barriers to primary care management and information to assist in decision-making. Data was collected through Qualtrics, an online survey platform enabling anonymous responses. The questionnaire was accessible from 29 August 2022 until 1 November 2022.
Once participants had consented to the survey, they were instructed to recall or review relevant electronic patient care records from their own cases in the past week where they were the treating paramedic and they transported the patient via emergency ambulance (i.e. excluding patients who were referred to a primary care provider).
The questionnaire asked participants to estimate the proportion of patients they transported that they believed to be appropriate for primary care management, as well as their confidence in recommending this management to patients in lieu of ambulance conveyance to an ED on a scale of 0 (no confidence) to 100 (complete confidence). Participants were then asked to indicate any barriers from a ‘select all that apply’ list with a free text ‘other’ option that they had faced in the past week when recommending a primary care service in lieu of conveyance to an ED.
Participants were asked to rank how important the information or training they received from various sources was to shaping their clinical decision-making for low-acuity patients. Sources of information that were investigated included university training, senior managers within their service, local managers/mentors, their peers and other information found via self-directed learning. Participants were asked to rate how supportive they felt each of these sources were in regard to diverting low-acuity cases to primary care in lieu of conveying a patient to an ED. This involved a 5-point Likert scale from 1 (extremely unsupportive) to 5 (extremely supportive). Finally, participants were asked to indicate how they believed the COVID-19 pandemic impacted their own support for referrals to primary care for low-acuity presentations, as well as their perception of change in support from senior managers within their service, the wider public and media, patients and their family members and the wider medical community. This was recorded on a 5-point Likert scale from 1 (significantly less supportive) to 5 (significantly more supportive).
Setting
Ambulance Victoria employs approximately 4500 full time equivalent operational clinical staff (Ambulance Victoria 2021) as the sole provider of emergency medical services for a total land area of approximately 227,500 km2 and population of 6.7 million residents. Paramedics are required to maintain registration with the Australian Healthcare Practitioner Regulation Agency, and practice within the scope of the publicly accessible Ambulance Victoria Clinical Practice Guidelines (Ambulance Victoria 2022). The clinical practice guidelines contain a short list of conditions and deranged vital signs (‘red flags’) that mandates the patient should be advised to attend an ED via ambulance, however outside of these conditions paramedics are able to autonomously decide to convey a patient to an ED or refer the patient to an alternative service. Paramedics also have the option of consulting the Victorian Virtual Emergency Department, which is a statewide service offering remote audiovisual consultations with ED physicians for medium-acuity patients, as previously described (Sher et al. 2022).
Participants
Participants were registered paramedics working within Victoria, Australia. Paramedics were required to have at least 6 months operational experience and have regular operational duties. ‘Regular’ operational duties were defined as at least 10 operational hours per week in the last 2-week period. All staff at the jurisdictional ambulance service were invited to participate in the questionnaire via an internal staff email with an online link, and it was not possible to derive the exact number of eligible paramedics given the ‘regular operational duties’ inclusion criteria.
Statistical methods
Responses were presented using descriptive statistics including frequencies, proportions, medians and interquartile ranges (IQRs). Information was presented visually using histograms, scatter plots and stacked bar charts.
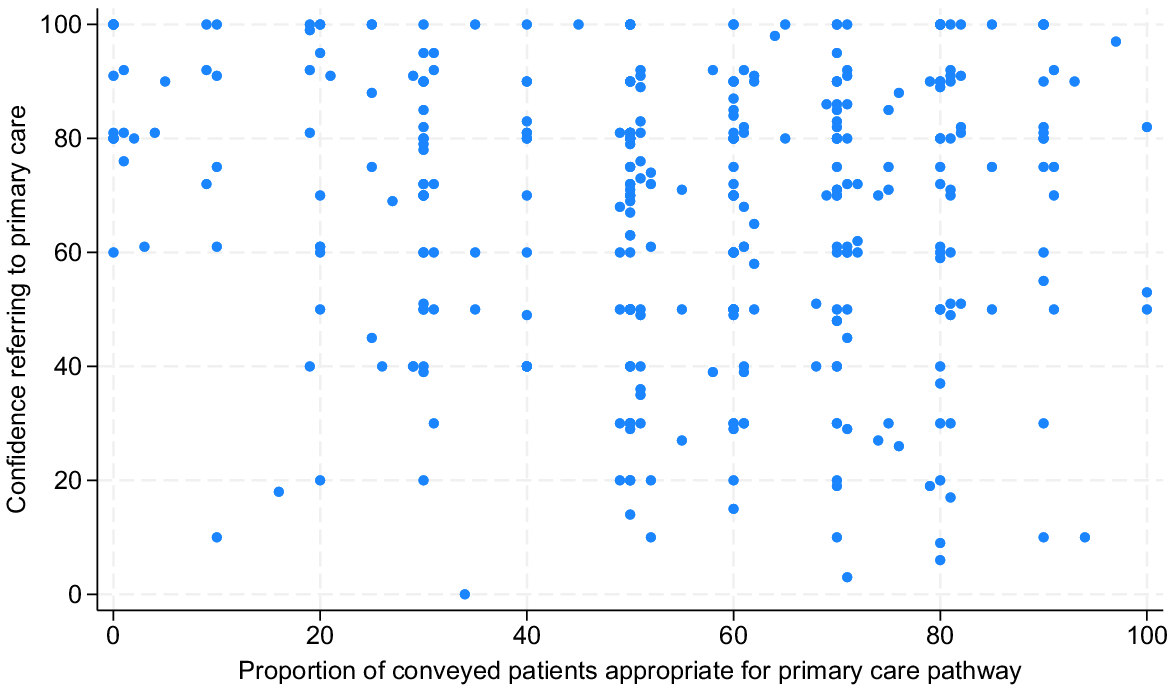
Correlation between paramedic confidence referring a patient to primary care and the proportion of primary care appropriate patients conveyed to an ED was shown visually using a scatter plot and further evaluated using Spearman’s Rho. Univariate logistic regression between participant reported barriers to referring low-acuity patients to primary care pathways and basic paramedic demographics such as age and gender were presented as odds ratio (OR) and 95% confidence intervals (CIs).
Results
In total, there were 367 complete responses. Participants had a median of 7 years experience as a paramedic (IQR 4–12 years), and the majority of participants (82%) practiced as Advanced Life Support (ALS) paramedics, as per Table 1. A total of 13% of participants reported not having access to an ED facility within 30 min drive of their usual work location.
| Characteristic | N (%) | |
|---|---|---|
| Gender | ||
| Man | 214 (58.3) | |
| Woman | 147 (40.1) | |
| Non-binary | 6 (1.6) | |
| Age (years) | ||
| 18–24 | 23 (6.3) | |
| 25–34 | 197 (53.7) | |
| 35–44 | 84 (22.9) | |
| 45–54 | 43 (11.7) | |
| ≥ 55 | 20 (5.5) | |
| Education | ||
| Vocational training | 28 (7.6) | |
| Undergraduate degree | 254 (69.2) | |
| Postgraduate degree | 85 (23.2) | |
| Role | ||
| Graduate paramedic | 17 (4.6) | |
| ALS paramedic | 301 (82.0) | |
| Intensive care paramedic | 46 (12.5) | |
| Extended scope paramedic | 3 (0.8) | |
| Additional experience | ||
| Secondary phone triage services | 30 (8.2) | |
| ALS single responder | 63 (17.2) | |
| Clinical educator | 200 (54.5) | |
| Communication and control centre | 3 (0.8) | |
| Patient frequency | ||
| 1–10 patients in the past week | 136 (37.1) | |
| 11–20 patients in the past week | 178 (48.5) | |
| 21–30 patients in the past week | 42 (11.4) | |
| ≥31 patients in the past week | 11 (3.0) | |
| Operational hours | ||
| 10–19 h in the past week | 14 (3.8) | |
| 20–29 h in the past week | 30 (8.2) | |
| 30–39 h in the past week | 63 (17.2) | |
| ≥ 40 h in the past week | 260 (70.8) | |
| Highest level of care within 30 min | ||
| None | 2 (0.5) | |
| Primary care only | 46 (12.5) | |
| Emergency department | 159 (43.3) | |
| Tertiary care facility | 160 (43.6) | |
Proportion suitable for primary care referral
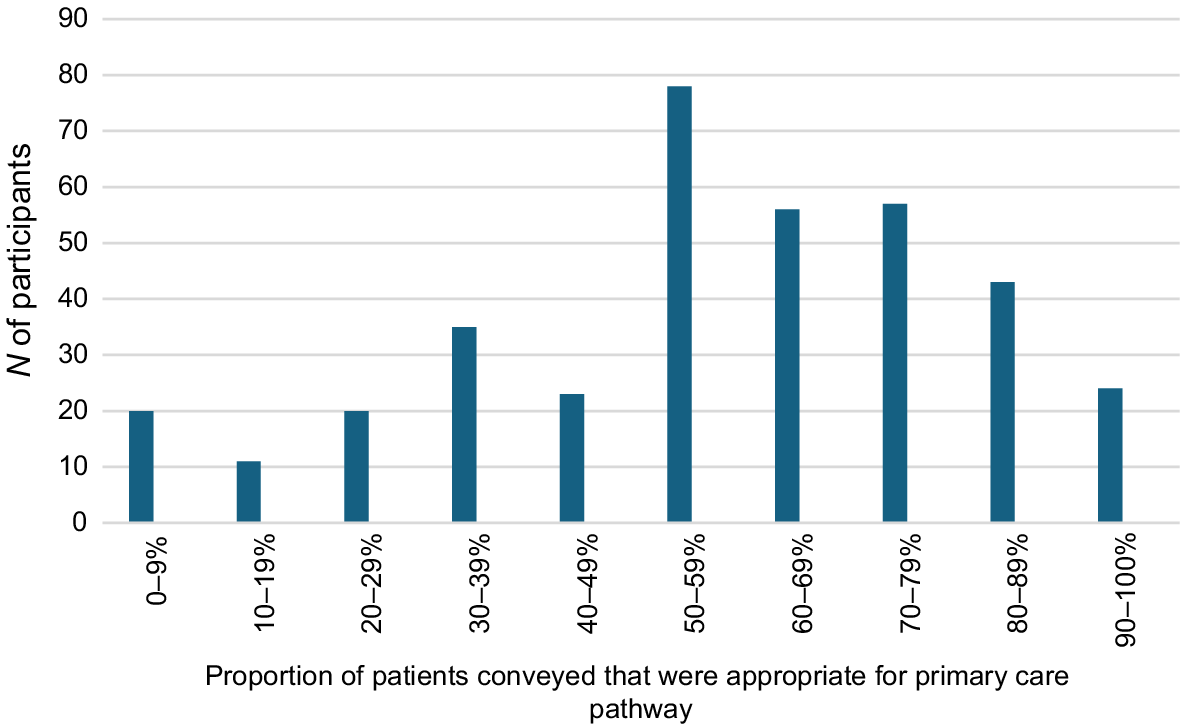
A total of 70% of participants reported that at least half of the patients they conveyed in the week prior to completing the questionnaire were suitable for a primary care pathway, as shown in Fig. 1. While intensive care paramedics reported lower rates of perceived primary care suitable conveyances, 57% of intensive care paramedics still reported at least half of their patients to be suitable for a primary care pathway. Only 3% (n = 10) of participants reported that all of their conveyed patients required paramedic services and were not suitable for primary care referral. In addition, 78% of participants reported discussing alternatives to ambulance conveyance with at least one of their patients that they ultimately conveyed.
Graph demonstrating proportion of patients participants conveyed to an ED via ambulance that were appropriate for a primary care pathway.
Participants rated their confidence in recommending primary care pathways to patients highly, with a median score of 72 (IQR 50–87). Using Spearman’s rank correlation, there was no relationship found between self-reported confidence in recommending primary care pathways and actual conveyance of perceived primary care suitable patients (r(367) = 0.05, P = 0.297) as shown in Fig. 2.
Barriers to primary care referral
Participants reported the most common barriers faced when attempting to refer a perceived primary care suitable patient was limited access to a primary care pathway (68%), the patient declining primary care referral (57%) and concern over the patients’ intention to follow-up with a primary care provider (54%), as shown in Fig. 3. Overall, 66% of participants reported that fear of an internal complaint, litigation or organisational pressure to convey patients to an ED was a barrier to referring patients to primary care pathways despite believing this was the most appropriate place of care for the patient.
Paramedic reported barriers to referring perceived primary care suitable patients to a primary care provider.
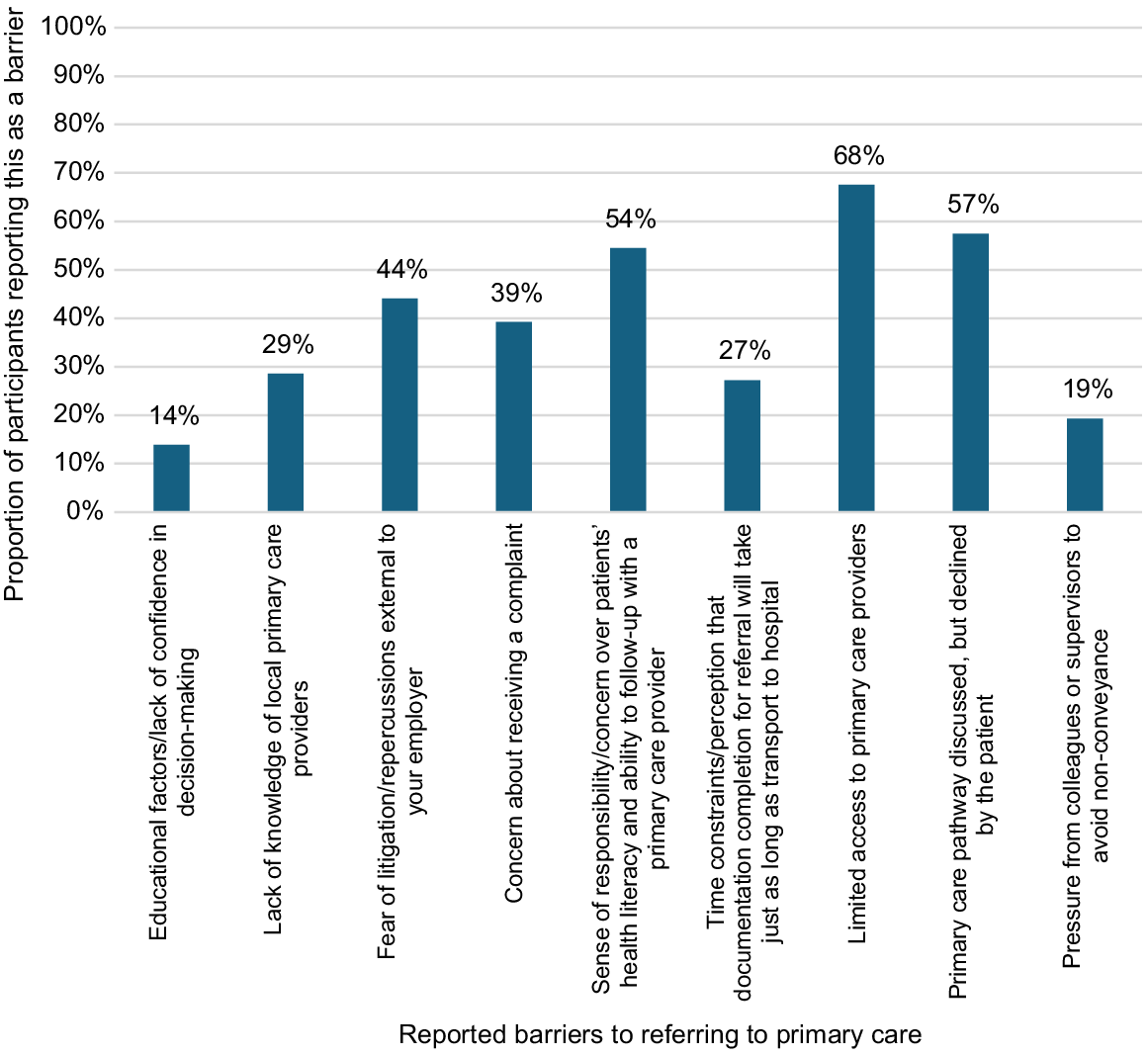
Paramedics reported different barriers to referring patients to primary care pathways based on their own gender. Men were almost twice as likely to report a lack of knowledge of suitable local primary care pathways compared to women colleagues (OR 1.68, 95%CI 1.04–2.72), whereas women were 75% more likely to report patients declining their recommendation to seek primary care in lieu of ambulance conveyance to an ED compared to men (OR 1.75, 95%CI 1.13–2.69).
Likewise, paramedics reported different barriers to referring patients to primary care based on their own age. Each increased decade of paramedic age was associated with a 32% decreased likelihood of educational factors or a lack of confidence in decision-making as a barrier to primary care referral (OR 0.68, 95%CI 0.48–0.97). Similarly, increasing paramedic age was associated with decreased fear of litigation (OR 0.65, 95%CI 0.51–0.82) and pressure from colleagues or supervisors to avoid non-conveyance (OR 0.58, 95%CI 0.42–0.81).
Primary care pathway education and support
Participants were asked to rank how important the information or training they received from various sources had been in shaping clinical decision-making for low-acuity patients, as shown in Fig. 4. Over a third of participants indicated that self-directed learning was the most important source of information for low-acuity patients, compared to only 3% of participants who found university to be the most important source of education and training for low-acuity patients.
Ranked importance of information sources on clinical decision making for low-acuity patients.
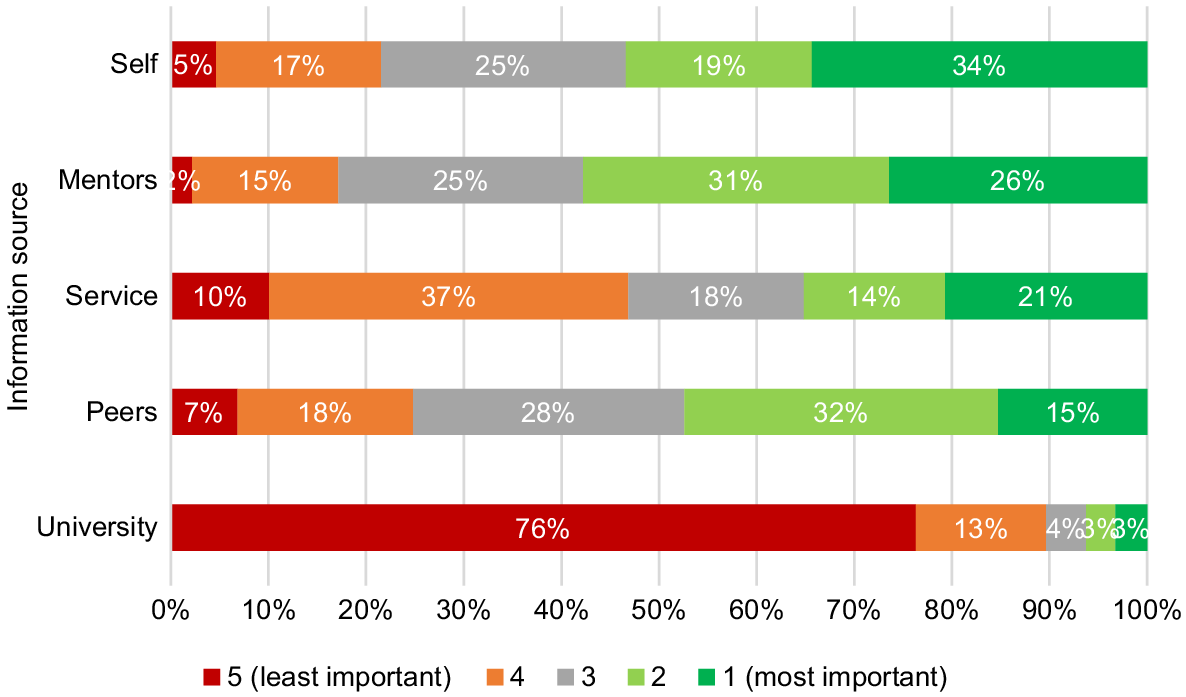
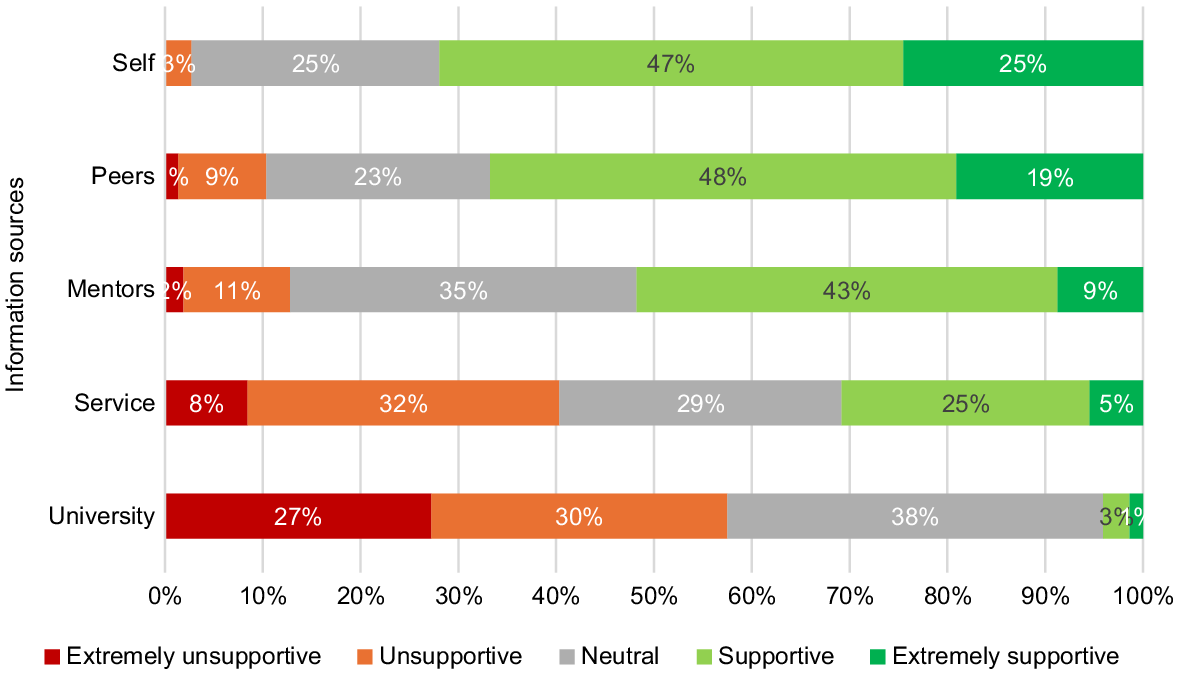
When assessing the perception of support for their decision to divert low-acuity patients from an ED, over 50% of participants stated they found university education to be extremely unsupportive (27%) or unsupportive (30%) towards diverting low-acuity cases to primary care pathways rather than an ED, as shown in Fig. 5. Only 1% of participants found their university education to be extremely supportive of diversion to primary care pathways. In comparison, no participants indicated they themselves were extremely unsupportive of diverting these patients to primary care pathways, and only 3% stated they were unsupportive. Similarly, two thirds of participants stated their peers were supportive (48%) or extremely supportive (19%) of diversion to primary care pathways.
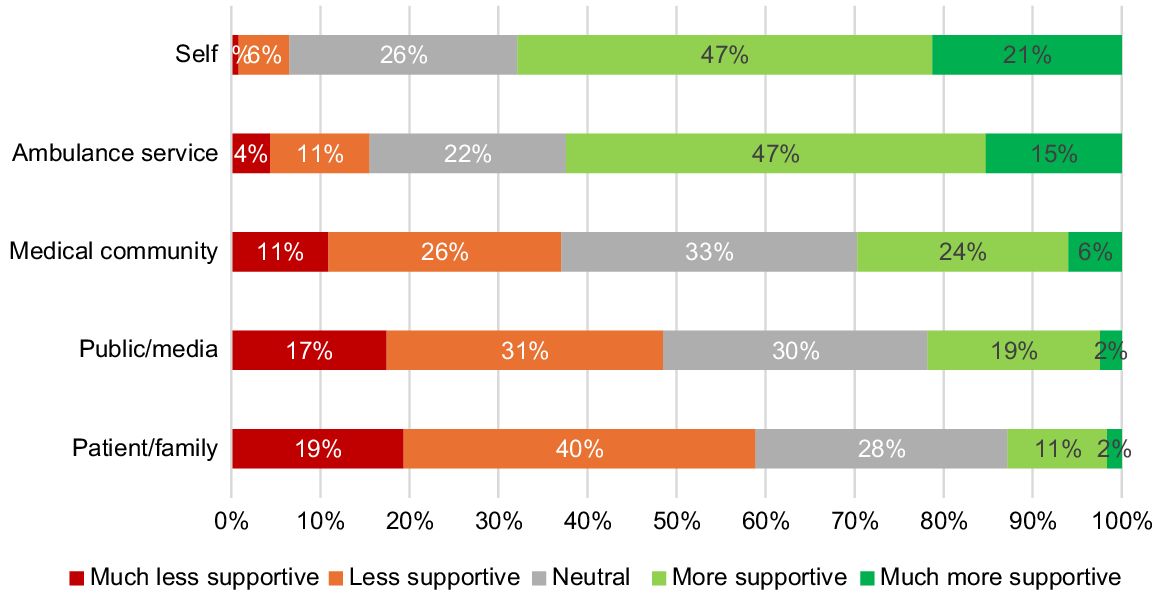
Changes in perception during the COVID-19 pandemic
Finally, participants were asked to indicate how they felt the COVID-19 pandemic had impacted referral to primary care providers for low-acuity patients as shown in Fig. 6. Participants reported their own personal support to have the largest shift in increased support for primary care pathway utilisation, with 68% reporting an increase in their support of the practice. Conversely, 59% of participants reported a perception that patients and their families showed decreased support for primary care pathways during the COVID-19 pandemic.
Discussion
Our study found that 70% of participants reported they perceived at least half of the patients they conveyed to an ED in the week prior to completing the questionnaire to be suitable for a primary care pathway. Participants reported high levels of confidence in referring patients to a primary care pathway, however this had no correlation with their actual practice. They reported a range of barriers, the most common of which was having limited access to suitable primary care pathways for patients. Paramedics reported themselves to be supportive of referring patients to primary care pathways, and that exposure to the COVID-19 pandemic increased this support. Despite this, they also reported that their colleagues, the broader ambulance service and universities were less supportive or not supportive of referral to primary care pathways.
These outcomes suggest that paramedics feel they are conveying a large proportion of patients to an ED who do not require their skills or expertise, and that there is limited practical and cultural support to correct this. The most commonly reported barrier to referring these patients to alternative places of care was a lack of access to suitable options. These deficits in primary care access have been highlighted in recent data where 39% of Australians who saw a GP for urgent medical care waited for 24 h or more, and 23% of patients felt they waited longer than acceptable for a GP appointment (Australian Bureau of Statistics 2021–2022). It is forecast that by the end of the decade there will be a 25% shortfall between the demand for GP services and supply in Australia (Deloitte Access Economics 2019). When a patient cannot access a GP, an ED often becomes the default place of care, and the responsibility for correcting this has complex political implications in the Australian setting given they have different sources of funding. In Australia, GPs are federally funded utilising the Medicare rebate scheme, with an option to have an additional fee paid by the service user, compared to hospitals (including EDs) which are substantially state-funded (Australian Institute of Health Welfare 2020). In Victoria, a range of state-funded services such as the Victorian Virtual Emergency Department and GP-led Priority Primary Care Centres have been introduced to offer care for patients who have non-emergent conditions. These services offer timely care when, and where, traditional GPs may not be available, although these services were in their infancy and not yet widely available to Victorian paramedics at the time of this survey. Since our data collection, the Australian federal government has also established 58 Medicare Urgent Care Centres which are available in all Australian states and territories (Department of Health and Aged Care 2024). Data regarding the frequency, safety and satisfaction associated with ambulance usage of these Urgent Care Centres are not yet available.
Globally, there is also an increasing usage of paramedic practitioners who can offer medication prescribing, wound care including suturing and referral for medical investigations to facilitate a patient remaining at home (Adibhatla et al. 2024). In the United Kingdom, paramedic practitioners are often integrated into primary care settings such as general practice and Urgent Care Clinics, which has been broadly perceived as positive by healthcare providers and patients alike (Eaton et al. 2021). Additionally, there is opportunity to incorporate a physician into an ambulance service, such as the Alternative Pre-hospital Pathway team in Cork, Ireland which demonstrated a non-conveyance rate of 68% (Patton et al. 2021). Many paramedic services utilise physicians to support paramedics in delivering intensive care for high-acuity patients, however it is a relatively new concept to incorporate physicians with the aim of reducing ED conveyance. In the Australian context, ambulance physicians are reserved for high-acuity patients, however paramedic practitioner models with varying scope to manage primary care presentations have existed for several decades (Blacker et al. 2009). Paramedic practitioner models have predominantly been utilised in rural and remote settings to fulfil workforce shortage gaps although the roles vary considerably between states (Shannon et al. 2022). Paramedic Community Support Coordinators have long been employed in Victoria, however their role is to support coordination and training of existing health services in rural Victoria rather than respond to, and divert, acute ambulance calls. The Victorian government has announced that paramedic practitioners are expected to commence working in Victoria in 2026, following completion of a specialist postgraduate degree that affords an extended skill set to respond to acute ambulance calls which may contribute to reduced ED conveyances (State Government of Victoria 2023). It is important to recognise that while paramedic practitioner models may be suitable for managing acute, low-acuity conditions or interim management while awaiting follow-up care, paramedics ultimately have reduced capacity to provide appropriate long-term follow-up for chronic conditions and do not replace the role that GPs play in providing holistic, relationship-based care (Royal Australian College of General Practitioners 2020).
The second most encountered barrier was a patient declining the referral to a primary care pathway. As per the Shared Code of Conduct that governs paramedic registration with the Australian Health Practitioner Regulation Agency, paramedics have a responsibility to ‘investigate and treat patients based on clinical need and the effectiveness of the proposed investigations or treatment, and not provide unnecessary services or encourage the indiscriminate or unnecessary use of health services’ (Australian Health Practitioner Regulation Agency 2022). Despite this, our results indicate that paramedics are frequently conveying patients to an ED based on patient preference rather than clinical need, which was particularly evident for women paramedics. Previous research has indicated that ambulance personnel feeling disrespected or undervalued leads to moral distress (Viele 2018), and this experience of having their recommendations declined by patients may contribute to this moral distress. It is unsurprising that this phenomenon is experienced more often by women paramedics, given previous research indicates that women physicians were almost twice as likely to have a patient refuse to allow them to provide care on the basis of their gender (Dyrbye et al. 2022). A lack of organisational support is also known to contribute to both moral injury in emergency service workers (Smith-MacDonald et al. 2021) and increased conveyance rates to an ED (O’Cathain et al. 2018). Given that two-thirds of participants in our questionnaire reported feeling that fear of an internal complaint, litigation or organisational pressure was a barrier to referring patients to primary care pathways, increased organisational support may be integral to reducing the number of perceived primary care suitable patients who are conveyed to an ED via ambulance.
A lack of paramedic education about primary care suitability was the least reported barrier to referring patients to primary care pathways, although only 24% of participants reported that formal sources such as university or service-led education were the most important sources of information for them. Conversely, the most informal source of information (self-directed learning) was rated as the most relied upon source of information. Additionally, older paramedics were less likely to consider a lack of education about primary care suitability on their behalf as a barrier to primary care pathway referral. This further supports the notion that paramedics are acquiring knowledge about primary care suitability from self-directed learning throughout their career. While non-conveyance is generally associated with low-levels of adverse patient outcomes (Ebben et al. 2017), it is concerning that there may be considerable variation in paramedic referral practices based on their own self-education. Participants consistently reported themselves to be more supportive of diversion to primary care pathways than those around them. This was particularly evident when comparing how the COVID-19 pandemic influenced perceived support for non-conveyance, where paramedics believed patients and families to be less supportive of primary care pathways. This is surprising, given presentations to hospitals dramatically decreased as a result of the COVID-19 pandemic, with patients delaying and avoiding hospitals even for life-threatening conditions (Cummins et al. 2022). As low-acuity patient presentations continue to increase it is important to investigate how supportive education for paramedics regarding primary care referrals impacts on patient willingness, and how communication between paramedics and this patient cohort can be improved.
Limitations
We were unable to determine the number of paramedics that met the inclusion criteria for this survey, and thus could not determine an exact response rate. Despite this, with a workforce of approximately 4500 FTE paramedics and 367 responses, the response rate is likely around 10%. This participation bias may have unduly influenced the study results.
Conclusion
Paramedics believe that at least half of the patients they convey to an ED are appropriate for referral to primary care pathways, however there are multiple barriers complicating this. Predominantly, paramedics face limited available primary care services and patients often refuse these services when recommended. While paramedics were predominantly supportive of referring patients to primary care pathways, most expressed concern over internal complaints, litigation or organisational pressure. Given the conflicting nature of paramedics conveying a significant proportion of patients to hospital whom they believe do not require this service, further research should examine if this contributes to moral injury and burnout for paramedics. The impact on broader health services, from both an economic and systems capacity perspective, should also be investigated.
Data availability
The data that support this study cannot be publicly shared due to ethical or privacy reasons and may be shared upon reasonable request to the corresponding author if appropriate.
References
Adibhatla S, Lurie T, Betz G, Palmer J, Raffman A, Andhavarapu S, Harris A, Tran QK, Gingold DB (2024) A systematic review of methodologies and outcome measures of mobile integrated health-community paramedicine programs. Prehospital Emergency Care 28, 168-178.
| Crossref | Google Scholar | PubMed |
Ambulance Victoria (2022) Clinical practice guidelines. Available at https://www.ambulance.vic.gov.au/paramedics/clinical-practice-guidelines/ [accessed 12 March 2022]
Andrew E, Nehme Z, Cameron P, Smith K (2020) Drivers of increasing emergency ambulance demand. Prehospital Emergency Care 24, 385-393.
| Crossref | Google Scholar | PubMed |
Australian Bureau of Statistics (2021–2022) Patient experiences. Available at https://www.abs.gov.au/statistics/health/health-services/patient-experiences/latest-release
Australian Health Practitioner Regulation Agency (2022) Code of conduct. Available at https://www.ahpra.gov.au/Resources/Code-of-conduct/Shared-Code-of-conduct.aspx
Borhani F, Abbaszadeh A, Nakhaee N, Roshanzadeh M (2014) The relationship between moral distress, professional stress, and intent to stay in the nursing profession. Journal of Medical Ethics and History of Medicine 7, 3.
| Google Scholar | PubMed |
Cummins NM, Garavan C, Barry LA, Devlin C, Corey G, Cummins F, Ryan D, Mccarthy G, Galvin R (2022) The impact of COVID-19 on an Irish Emergency Department (ED): a cross-sectional study exploring the factors influencing ED utilisation prior to and during the pandemic from the patient perspective. BMC Emergency Medicine 22, 176.
| Crossref | Google Scholar | PubMed |
Delardes B, Nehme E, Bowles K-A, Chakraborty S, Cox S, Smith K (2024) Characteristics and outcomes of patients referred to a general practitioner by Victorian paramedics. Prehospital Emergency Care 1-10.
| Crossref | Google Scholar |
Department of Health and Aged Care (2024) About medicare urgent care clinics. Available at https://www.health.gov.au/our-work/medicare-urgent-care-clinics/about-medicare-urgent-care-clinics [accessed 27 June 2024]
Dyrbye LN, West CP, Sinsky CA, Trockel M, Tutty M, Satele D, Carlasare L, Shanafelt T (2022) Physicians’ experiences with mistreatment and discrimination by patients, families, and visitors and association with burnout. JAMA Network Open 5, e2213080.
| Crossref | Google Scholar | PubMed |
Eaton G, Wong G, Williams V, Roberts N, Mahtani KR (2020) Contribution of paramedics in primary and urgent care: a systematic review. British Journal of General Practice 70, e421-e426.
| Crossref | Google Scholar |
Eaton G, Wong G, Tierney S, Roberts N, Williams V, Mahtani KR (2021) Understanding the role of the paramedic in primary care: a realist review. BMC Medicine 19, 145.
| Crossref | Google Scholar | PubMed |
Ebben RHA, Vloet LCM, Speijers RF, Tönjes NW, Loef J, Pelgrim T, Hoogeveen M, Berben SAA (2017) A patient-safety and professional perspective on non-conveyance in ambulance care: a systematic review. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine 25, 71.
| Crossref | Google Scholar | PubMed |
King R, Oprescu F, Lord B, Flanagan B (2021) Patient experience of non-conveyance following emergency ambulance service response: a scoping review of the literature. Australasian Emergency Care 24, 210-223.
| Crossref | Google Scholar | PubMed |
King R, Oprescu FI, Lord B, Flanagan B, Downer T (2023) Patients’ experiences of non-conveyance following an Australian ambulance service paramedic response: a constructivist grounded theory exploration. Paramedicine 20, 63-78.
| Crossref | Google Scholar |
Kirk A, Armstrong K, Nurkka N, Jinks A (2018) The impact of blame culture on paramedic practice: a qualitative study exploring English and Finnish paramedic perceptions. International Journal of Emergency Services 7, 214-227.
| Crossref | Google Scholar |
Knowles E, Bishop-Edwards L, O’Cathain A (2018) Exploring variation in how ambulance services address non-conveyance: a qualitative interview study. BMJ Open 8, e024228.
| Crossref | Google Scholar | PubMed |
Lederman J, Löfvenmark C, Djärv T, Lindström V, Elmqvist C (2023) A phenomenological interview study with patients being non-conveyed in the ambulance service. BMC Emergency Medicine 23, 30.
| Crossref | Google Scholar | PubMed |
Lowthian JA, Jolley DJ, Curtis AJ, Currell A, Cameron PA, Stoelwinder JU, Mcneil JJ (2011) The challenges of population ageing: accelerating demand for emergency ambulance services by older patients, 1995–2015. Medical Journal of Australia 194, 574-578.
| Crossref | Google Scholar | PubMed |
Newton A, Hunt B, Williams J (2020) Disruptive innovation: barriers, opportunities and differences internationally. International Paramedic Practice 10, 63-77.
| Crossref | Google Scholar |
O’Cathain A, Jacques R, Stone T, Turner J (2018) Why do ambulance services have different non-transport rates? A national cross sectional study. PLoS ONE 13, e0204508.
| Crossref | Google Scholar | PubMed |
Oosterwold J, Sagel D, Berben S, Roodbol P, Broekhuis M (2018) Factors influencing the decision to convey or not to convey elderly people to the emergency department after emergency ambulance attendance: a systematic mixed studies review. BMJ Open 8, e021732.
| Crossref | Google Scholar | PubMed |
Patton A, O’Donnell C, Keane O, Henry K, Crowley D, Collins A, Redmond E, Glynn N, Dunne M, Deasy C (2021) The Alternative Pre-hospital Pathway team: reducing conveyances to the emergency department through patient centered Community Emergency Medicine. BMC Emergency Medicine 21, 138.
| Crossref | Google Scholar | PubMed |
Richards JR, Ferrall SJ (1999) Inappropriate use of emergency medical services transport: comparison of provider and patient perspectives. Academic Emergency Medicine 6, 14-20.
| Crossref | Google Scholar | PubMed |
Royal Australian College of General Practitioners (2020) The role of specialist GPs. Available at https://www.racgp.org.au/advocacy/position-statements/view-all-position-statements/health-systems-and-environmental/the-role-of-specialist-gps [accessed 13 March 2022]
Shannon B, Eaton G, Lanos C, Leyenaar M, Nolan M, Bowles K-A, Williams B, O’Meara P, Wingrove G, Heffern JD, Batt A (2022) The development of community paramedicine; a restricted review. Health & Social Care in the Community 30, e3547-e3561.
| Crossref | Google Scholar | PubMed |
Sher L, Semciw A, Jessup RL, Carrodus A, Boyd J (2022) Structured evaluation of a virtual emergency department triage model of care: a study protocol. Emergency Medicine Australasia 34, 907-912.
| Crossref | Google Scholar | PubMed |
Smith-Macdonald L, Lentz L, Malloy D, Brémault-Phillips S, Carleton RN (2021) Meat in a seat: a grounded theory study exploring moral injury in canadian public safety communicators, firefighters, and paramedics. International Journal of Environmental Research and Public Health 18, 12145.
| Crossref | Google Scholar |
State Government of Victoria (2023) Delivering Australian-first paramedic practitioners. Available at https://www.premier.vic.gov.au/delivering-australian-first-paramedic-practitioners [accessed 27 June 2024]