Efficacy of a structured audio-visual asthma care session during GP visit in Australia: a single GP centre intervention trial
Md Imrose Hasan A , K. M. Shahunja B C * and Abdullah Mamun B C
B C * and Abdullah Mamun B C
A
B
C
Abstract
This study aims to assess the effectiveness of a structured audio-visual educational session for people on asthma symptoms management during a general practitioner visit.
We conducted this single-centre intervention study in a general practice clinic in Queensland, Australia. There were 78 intervention and 78 control participants in this study. We followed 1:1 randomisation to allocate study intervention between two groups of participants with asthma. The intervention group received an audio-visual demonstration of asthma, its symptoms, triggers, and how to use inhalers correctly, along with the standard asthma management by a physician on enrolment. The control group received only the standard asthma management by a physician. We assessed the ‘Asthma Control Test’ score on enrolment and after 90 days and compared the changes across the groups.
Participants were, on average, 28 years old (range: 6–60, 60% women). The intervention group showed a 1.9-unit increment, and the control group showed a −0.5-unit increment in ‘Asthma Control Test’ score from baseline to endline. The difference of differences between the intervention and control groups was 2.4 units (P = 0.016) after adjusting for potential confounders. In age-stratified analysis, the children (6–17 years) showed a significant difference (mean difference of 2.5 between intervention and control groups) in their asthma control score.
Structured educational sessions involving audio-visual media along with standard management for people with asthma during general practice visits would be effective for better asthma control. However, a further multi-centre study with a larger sample is needed to see its efficacy.
Keywords: asthma, asthma control, asthma education, audio-visual, Australia, efficacy, GP, intervention.
Introduction
Asthma is one of the most common chronic, non-communicable diseases in children and adults that causes variable respiratory symptoms (Papi et al. 2018). It also impacts the psychological and social well-being of people living with the condition (Stanescu et al. 2019). The global prevalence of self-reported, doctor-diagnosed asthma in adults is ~4%. However, the prevalence varies across countries, and Australia is one of the high prevalent countries for asthma in the world (To et al. 2012). According to the National Health Survey in 2017–2018, one in every nine Australians had asthma diagnosed by a doctor or nurse (AIHW 2020). Although Australia has made substantial progress in reducing hospital attendance and mortality, asthma remains a major public health problem (National Asthma Council Australia 2022a), and it incurs a substantial financial burden on the Australian health system (AIHW 2020).
Asthma is the most frequently managed chronic health problem in general practice settings in Australia (Barton et al. 2009). The National Asthma Council Australia (NAC) has provided a comprehensive, evidence-based guideline for asthma management and invaluable resources for patients, carers, and health professionals (National Asthma Council Australia 2015). Despite the excellent access to effective pharmacological treatments and valuable resources for asthma prevention, it could not achieve a satisfactory outcome for asthma management. The NAC has identified several key challenges facing asthma management in Australia (National Asthma Council Australia 2018). There are several issues in people with asthma or their caregivers that undermine the prevention strategy and effectiveness of the therapeutic treatment. The authors mentioned that most people with asthma do not use their inhalers correctly, resulting in suboptimal medication administration, poor asthma control, increased risk of flare-ups, and lack of perceived benefit by the people. Up to 90% of people demonstrate the incorrect technique with either standard pressurised metered-dose inhalers or dry-powder inhalers (National Asthma Council Australia 2018). Lack of awareness, education, and skills have been identified as the main factors behind these low levels of compliance with the standard management practice by the people (National Asthma Council Australia 2018).
Educational awareness is considered an effective problem-solving approach to the delivery of health care that standardises the management of patients’ preferences and values in making the best clinical decisions about asthma (Urek et al. 2005; Clark et al. 2009; Carvalho Coelho et al. 2016). As a part of the educational awareness to prevent asthma, the NAC introduced the ‘Asthma Action Plan’ (National Asthma Council Australia 2022a) for all people with asthma. However, many people with asthma do not have a current written asthma action plan. In 2017–2018, it was identified that only 31% of people with asthma across all ages had a written asthma action plan (AIHW 2020) despite the recommendations that every person with asthma have an asthma action plan. The percentage is even lower among people above 15 years of age (AIHW 2020). Adherence to this type of asthma action plan or self-management strategies is also not adequate. Global studies reported that poor adherence to asthma self-management is very common and a significant contributor to inadequately controlled asthma (Dunbar-Jacob et al. 2000). However, patient education is the foundation for increasing adherence and effective self-management (Eakin and Rand 2012). Evidence from multiple studies reported the value of educational interventions for improving people adherence to asthma self-management practices (Gibson et al. 2000). Several modalities of educational interventions were found in earlier studies. Family-focused education was delivered at the bedside during an acute asthma hospitalisation (Mosnaim et al. 2017), through individual telephone calls (Baptist et al. 2020), and through demonstration in a school setting for children with asthma (Mosnaim et al. 2016) to increase the compliance to the asthma action plan and better manage symptoms. However, data are limited regarding the effectiveness of this type of educational intervention in general practice settings, especially in Australia.
The role of the general practitioner (GP) is an influential factor that significantly impacts asthma outcomes. The general practice setting can enable patients to access essential educational resources during a GP consultation. Visual, audio-visual, printed, and online resources can be used for the patient at the centre before consultation when patients are more receptive to the information due to the high relevance (Riera et al. 2017; Shah and Gupta 2017). In particular, video demonstration was found to be more effective than written instruction in improving compliance with self-administered treatment (Shah and Gupta 2017). However, GPs are often under a time constraint due to multiple competing demands, and they hardly have any protected time for patient education (National Asthma Council Australia 2015). Not all general practices are well equipped with nursing support available to educate people with asthma. Moreover, patients’ reluctance to explore educational resources and their attitude toward asthma (being a non-fatal condition) has been preventing them from accessing the resources to improve their knowledge and attitude towards asthma and its self-management (National Asthma Council Australia 2018). Thus, it is important to include a structured educational session involving audio-visual asthma care resources during general practice visits.
This study aims to assess the effectiveness of a structured audio-visual educational session for asthma during a general practice visit on asthma symptoms management. The findings of this study may provide further evidence of the effectiveness of awareness and education on asthma management by the people.
Methods
Study setting
We conducted this study at Coomera Town Medical Centre, Queensland, Australia. This primary healthcare clinic provides bulk bill services to the community and treats approximately 1000 patients of all ages per month. They provide comprehensive health care to all individuals and their families in the community and specialised care for specific age groups such as children, women, and the elderly.
Study participants
We included participants aged 6–60 years, of either sex, confirmed as having asthma for the first time by an attending physician while visiting the clinic, English speaking, and who gave consent to participate in this study (Table 1). Asthma was diagnosed by a physician based on history, clinical examinations, and spirometry following NAC guidelines (National Asthma Council Australia 2022a). We chose this age group for our study participants as confirming the diagnosis of asthma below 6 years is difficult due to difficulty performing lung function testing (e.g. spirometry) below 6 years (Ducharme et al. 2015). In Australia, ~80% of older people (aged 65 years and above) have at least one chronic health condition (AIHW 2021). We limited our participants’ ages to 60 years to avoid possible chronic health conditions, including a window period of 5 years. We also had some exclusion criteria for selecting the participants, including having a known co-morbidity and other physiological or pathological condition that may have different pathophysiology of asthma and may hinder the intervention (Table 1). We purposefully excluded people with co-morbidity and pregnancy or lactation as these pathological and physiological conditions may interfere with our study intervention. A person with an unstable mental condition might not follow our intervention as it consisted of educational materials. We excluded tourists or people who were not residents of the area near the study site, as we had a follow-up visit on/after 90 days of the enrolment, and these people had a high chance of being lost to follow-up. We also purposefully excluded Aboriginal and Torres Strait Islander peoples as they have a significantly higher prevalence of asthma than the non-Indigenous population in Australia (AIHW 2020). They often presented with co-morbidities (Jenkins et al. 2009). Moreover, our proposed intervention is for the overall population. Aboriginal or Torres Strait Islander people need culturally tailored intervention because they respect cultural differences, build trust, and improve engagement with health services (Bainbridge et al. 2015).
| Inclusion criteria | Exclusion criteria | |
|---|---|---|
Sample size
For sample size calculation, we considered a prior study by Reddel et al. (2015) where they calculated the average asthma score from a nationwide representative sample in Australia. The average asthma score was 19.20 [standard deviation (s.d.) 5.28] in that study. We assume, in our population, the baseline mean asthma score to be the same (but due to the small sample size, the s.d. would be double), and our proposed intervention may increase the asthma score by 20% from the baseline. To determine the appropriate sample size for our study, we aimed to detect a medium effect size with a power of 80% at a 5% significance level. Based on prior literature and theoretical considerations, we estimated an effect size (Cohen’s d) of 0.5. Therefore, the required sample size per group is approximately 78 participants in each group (156 in total).
Randomisation
After enrolment of the study, we randomised the participants in a 1:1 ratio to the intervention arm and control arm. We followed the permuted block (size of 4) technique (Broglio 2018) for randomisation to make the allocation equal at any time point of the study. The researchers of this study had no role in the randomisation and allocation process. Dedicated study nurses of the general practice clinic performed this task.
Study interventions
After randomisation and allocation of the study arms, the control group received the standard management for asthma by a GP. The standard intervention consisted of medical treatment as per their need, advice as to the use of a metered-dosed inhaler (no powder, for children with spacer), and general asthma education by the attending GP. The intervention group received one additional educational session by a trained study nurse in addition to the standard management for asthma by the attending GP. The education materials consisted of an audio-described video display in English adopted from the NAC (National Asthma Council Australia 2022b) and Nucleus Medical Media (Nucleus Medical Media 2022). The Nucleus Medical Media’s video described what asthma is, its symptoms, and its triggering factors. The NAC’s video demonstrated the standard procedure for using a metered-dose inhaler with and without a spacer. The graphical presentation of these videos showed how the children should use inhalers with a spacer, and how an adult can use an inhaler properly without a spacer. However, the NAC’s graphical presentation videos that we used in our trial have now been updated by human demonstration as role play videos. The total length of these two (Nucleus Medical Media and any of the two NAC videos) videos was ~5 minutes. We demonstrated the video in a dedicated room at the clinic to avoid cross-intervention with the control group participants. Other than these videos, no other health education related to asthma control was provided. However, all participants received general asthma education from the attending GPs as their standard practice during the GP consultations. In the case of child participants, the attending parents/carers received the study intervention on behalf of their children.
Data collection
We used a pre-tested case record form to collect all socio-demographic and clinical data of the participants. On enrolment, we collected several sociodemographic and clinical data from the participants. We considered the Asthma Control Test (ACT) (see Supplementary Table S1) as our outcome variable. We adopted this scoring system from the Australian Asthma Handbook which was originally developed by Asthma Australia, in association with the NAC and GlaxoSmithKline (Asthma Australia 2021). This scoring system has five asthma questions, five responses, and an overall score ranging from five to 25 points. Fewer points indicate the worst control of asthma. We assessed asthma scores for all participants on day zero (just after enrolment, before receiving any intervention) as our baseline score and on day 90 as our endline score. We set a 90-day follow-up to assess our endline measurements as it is recommended to have follow-up visits every 3–6 months for participants with asthma according to their severity/symptoms (Horak et al. 2016). Attentiveness to the intervention media was measured by direct observation by a dedicated study nurse.
Statistical analysis
Statistical analysis was performed on data from all randomised participants in the study on an intention-to-treat (Tripepi et al. 2020) basis. Descriptive statistics of the baseline characteristics are presented in percentage, mean, and standard deviations as appropriate. We compared baseline characteristics of both treatment and control arms and presented their P values. To assess the treatment effect, we conducted a ‘longitudinal analysis of covariates’ (Twisk et al. 2018) after adjusting for potential confounders (see Results section) to assess the independent effect of the intervention on asthma. In our study, we considered confounding factors that may alter the effect of the association between the intervention and outcome such as paticipant’s age, sex, carpet use at home or bedroom, exposure to smoking, furry pet at home, gas stove, and adverse neighbourhood characteristics (such as neighbourhood cleanliness; having adequate parks, playgrounds, and play spaces; neighbourhood traffic load). Several studies have reported significant associations of these factors with asthma (Shahunja et al. 2021). We also adjusted the baseline characteristics. Results are presented with mean changes (difference between endline score and baseline score) of outcome variables across the groups and the difference between their differences. A P-value less than 0.05 was considered to have statistical significance. All statistical analyses were done using a personal computer and statistical software STATA (StataCorp, USA, ver. 17.0).
Ethics
Participation in this study was voluntary. We only enrolled a participant in this study after having written informed consent. However, the participants had the full right to withdraw from the study at any time until the completion of this study. Participants received standard management for asthma by a GP from the centre if anyone denied taking part in this study. This study was approved by the Human Research Ethics Committee of the University of Queensland (Approval number: 2019002311).
Results
Participants
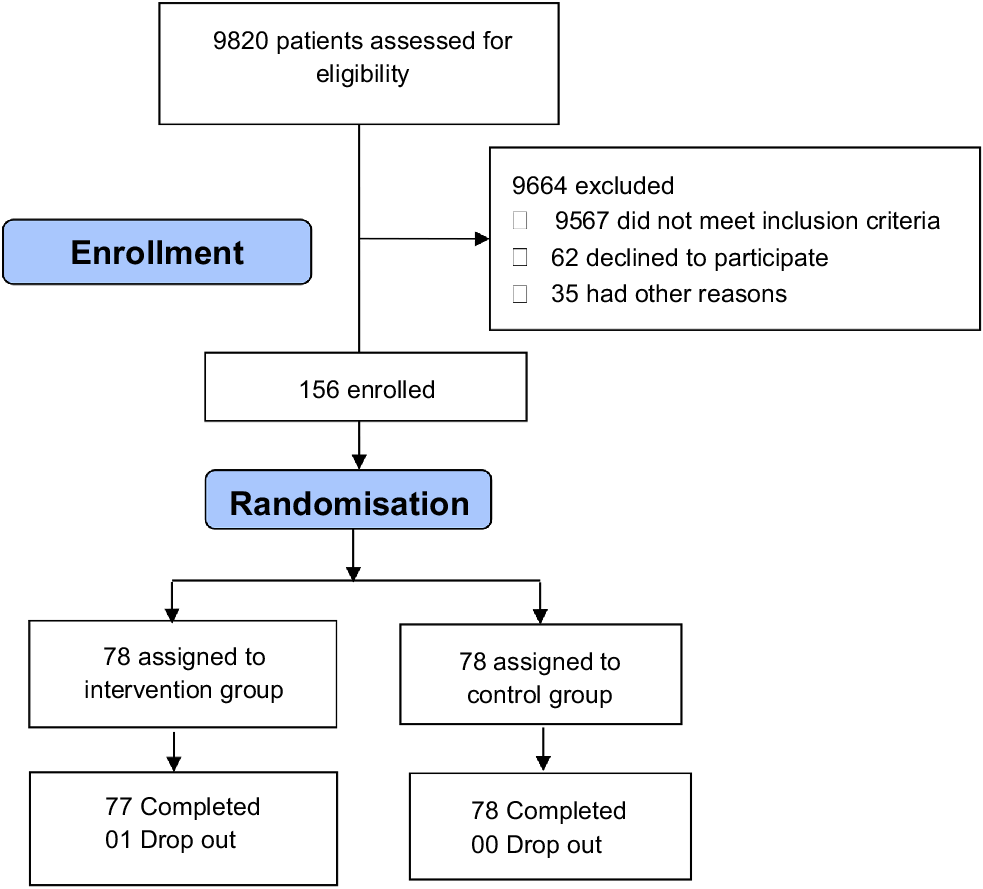
From February 2020 to August 2021, we screened 9820 people for the eligibility criteria of this study and identified 595 (6%) potential participants with asthma, 156 were enrolled in this study and the other 439 were excluded due to one or more exclusion criteria as mentioned earlier. The regular pace of enrolment of the participants was hampered in April and May 2020 due to the outbreak of COVID-19. After randomisation, we assigned 78 participants to the intervention group and another 78 participants to the control group (Fig. 1). We had only one participant drop-out who was in the intervention group. We could limit the dropout to almost nil as we had strong inclusion and exclusion criteria, participants came from the usual catchment area, and there were regular patients of this general practice centre. A consort flow chart has described the enrolment process of our study (Fig. 1).
Baseline characteristics
Although age-stratified randomisation was not performed, 21% of our study participants were children (6–17 years). Overall, 60% of the participants were female. Half of the participants were overweight/obese (body mass index ≥25), and half of the overall participants had a furry pet at home (Table 2). Some of these characteristics were comparable across the groups (intervention vs control). However, the percentage of participants who did not have a spacious and clean neighbourhood, furry pet, carpet, or gas heater in the house and were exposed to active and passive tobacco smoking were not comparable across the groups that may occur by chance. Details about baseline characteristics are described in Table 2. The baseline asthma score was approximately 19.6 (±4.8) for overall participants (Table 2). Although our target was to measure the endline asthma score on day 90 of the enrolment, the mean days for endline measurement for the intervention group were 96.1 days and 98.2 days for the control group, which was statistically not significant (Supplementary Table S2).
| Characteristics | Total | Intervention group | Control group | P-value | |
|---|---|---|---|---|---|
| N = 156, n (%) | N = 78, n (%) | N = 78, n (%) | |||
| Age (mean, s.d.) | 28.3 (13.1) | 27.2 (13.2) | 29.3 (13.0) | 0.156 | |
| Age groups | |||||
| Children (6–17 years) | 33 (21.1) | 21 (26.9) | 12 (15.3) | 0.078 | |
| Adults (18–60 years) | 123 (78.8) | 57 (73.1) | 66 (84.6) | ||
| Female sex | 93 (59.6) | 51 (65.3) | 42 (53.8) | 0.093 | |
| Body mass index (BMI) | |||||
| Overweight/obese | 79 (50.9) | 38 (49.0) | 41 (53.2) | 0.573 | |
| Neighbourhood characteristic: spacious and clean–Disagree | 21 (13.4) | 14 (17.9) | 7 (8.9) | 0.020 | |
| Poorly ventilated house (yes) | 9 (5.7) | 5 (6.4) | 4 (5.1) | 0.731 | |
| Furry pet at home (yes) | 75 (48.0) | 42 (53.8) | 33 (42.3) | 0.041 | |
| Carpet in house (yes) | 137 (87.8) | 73 (93.5) | 64 (82.0) | 0.002 | |
| Gas stove in the house (yes) | 62 (39.7) | 36 (46.1) | 26 (33.3) | 0.021 | |
| Cigarette smoking (yes) | 28 (17.9) | 6 (7.6) | 22 (28.2) | <0.001 | |
| Passive smoking at home (yes) | 22 (14.2) | 6 (7.6) | 16 (21.0) | 0.001 | |
| Asthma score (baseline) (mean, s.d.) | |||||
| All participants (N = 156) | 19.6 (4.8) | 19.1 (5.0) | 19.60 (4.6) | 0.552 | |
| Children (N = 33) | 19.9 (4.2) | 19.8 (4.2) | 20.08 (4.4) | 0.861 | |
| Adults (N = 123) | 19.2 (4.9) | 18.8 (5.3) | 19.51 (4.6) | 0.492 | |
Comparison done between intervention and control groups. A P-value <0.05 (bold text) was considered as a statistically significant difference.
Seasonality of the enrolment
June and July seemed the peak season for maximum enrolment of participants with asthma. Forty-five percent of the total participants were enrolled during these 2 months of the year (Supplementary Fig. S1). The highest enrolment in these months was possibily due to winter and the outbreak of COVID-19 as people visited the general practice centres more often due to respiratory symptoms at this time. On the other hand, we had fewer enrolments in April and May 2020, perhaps due to repeated lockdowns, quarantine, and relatively less movement of people outside the home.
Compliance with the intervention
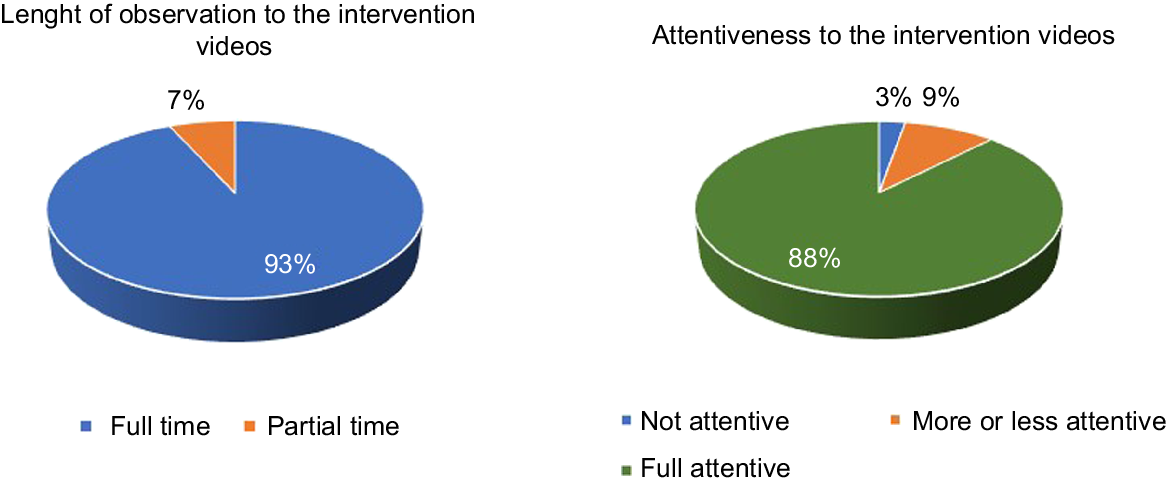
In our study, most of the participants in the intervention arm showed good compliance with our intervention materials. More than 90% of participants watched the educational videos (intervention materials) at full length. Eighty-eight percent of participants watched the videos with full attention (Fig. 2).
Intervention effects
Irrespective of age, intervention group participants had an increment of 1.9 units in their ACT score at the endline compared to the baseline. However, the control group had a decline in this score by ~0.5 units. Thus, the intervention group achieved a ~2.5-unit better increment in asthma score compared to the control arm, which was statistically significant. Children also showed a remarkable increment in ACT score in comparison to the control group in the age-stratified analysis. However, it did not show statistical significance due to a lack of sample (Table 3).
| Age group | Unadjusted | Adjusted | P-value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention group | Control group | DiD | P-value | Intervention group | Control group | DiD | |||
| Mean (s.e.) | Mean (s.e.) | Mean (s.e.) | |||||||
| Mean (s.e.) | Mean (s.e.) | Mean (s.e.) | |||||||
| All participants (N = 156) | 1.9 (0.7) | −0.5 (0.7) | 2.4 (1.0) | 0.010 | 1.9 (0.7) | −0.5 (0.7) | 2.4 (1.0) | 0.011 | |
| Children (N = 33) | 2.0 (1.2) | −0.5 (1.6) | 2.5 (2.1) | 0.230 | 2.0 (1.2) | −0.5 (1.5) | 2.5 (1.9) | 0.219 | |
| Adults (N = 122) | 1.9 (0.8) | −0.5 (0.8) | 2.4 (1.1) | 0.040 | 1.9 (0.8) | −0.5 (0.8) | 2.4 (1.1) | 0.030 | |
Adjusted for age (in all participants group), sex, carpet, smoking (active), smoking (passive), neighbourhood characteristic, furry pet at home, gas stove at home, and time (in days) to endline measurement. A P-value <0.05 (bold text) was considered as a statistically significant difference.
s.e., standard error; DiD, difference in differences.
Discussions
Our intervention consisted of an audio-visual demonstration focusing on asthma, including its definition, symptoms of an asthma attack, and common triggering factors. Additionally, we provided guidance on the correct usage of a metered-dose inhaler, both with and without a spacer. Our study revealed that a simple educational video on asthma significantly improved asthma control scores for a 2.5-unit increment in a general practice setting. However, the significance of an improvement of a clinical score due to an intervention should be based on the Minimal Clinically Important Difference (MCID), which is the smallest change or difference in an outcome measure that is perceived as beneficial and would lead to a change in the patient’s medical management (Bonini et al. 2020). Several previous studies, including a recent review article, (Schatz et al. 2009; Bonini et al. 2020) have shown that an MCID for an ACT score is 3 points for adults and 2 points for children aged 12–18 years, indicating significant clinical improvement. Moreover, Asthma Australia interprets a change of 3 points in the ACT score as clinically important (Asthma Australia 2021). Therefore, the improvement in the ACT score of 2.5 out of a total of 25 in the overall population (both children and adults) seems significant considering the MCID of the ACT score. The actual cause of asthma symptoms is still unknown (Mims 2015), but many cross-sectional and longitudinal studies have found its association with a range of multifactorial risks (Dick et al. 2014a). Interactions among a range of genetic and environmental risk factors are thought to play an important role in triggering asthma-like symptoms (Yang et al. 2017). It is impossible to alter the genetic factors, so controlling the environmental risk factors would be the best strategy to manage this condition. Studies across the globe reported several environmental triggers for asthma (Apelberg et al. 2001; Ahluwalia and Matsui 2011; Dick et al. 2014b; Bowatte et al. 2015; Hollenbach and Cloutier 2015; Lau et al. 2018). Optimal management of asthma depends on the accurate identification of asthma triggers and their prevention. Many potential asthma triggers, such as pollen, house dust mites, mould, small particulate matter, or respiratory viruses, do not have a phenomenal appearance that is easy to perceive. Thus, people have a variable degree of knowledge about these triggering factors (Janssens and Ritz 2013). Adequate knowledge about common asthma triggers may help people to identify and prevent this factor to control asthma. Our intervention materials described some common triggering factors for asthma. Perhaps it boosted the participants’ perception of asthma triggers and implied further importance in preventing these. Eventually, it might improve asthma control.
Management of asthma and allergies consists of pharmacological management and avoidance of triggers that cause symptom exacerbations (Reddel et al. 2014). Another important component of our intervention materials was how to use inhalers properly. Metered-dose inhalers are the most common and vital pharmacological intervention for people with asthma. The preferred methods of medication delivery in asthma are through metered-dose inhalers, which deliver medication straight to the lungs. Studies consistently report that inhalation techniques in both adults and children might be poor (Cochrane et al. 2000; Sleath et al. 2011) and the proper technique of using metered-dose inhalers is important for asthma control (Price et al. 2011). A systematic review found that the inhaler technique significantly improves after educational interventions, regardless of whether provided by a nurse, pharmacist, or physician or whether that education occurred online, in a clinic, or as part of a school-based program (Gillette et al. 2016). The National Heart, Lung, and Blood Institute guidelines recommend that healthcare providers check inhaler techniques at every opportunity and correct any deficiencies if they are seen (Mensah et al. 2018). However, compliance with this instruction sometimes would be difficult, especially in general practice settings. Not all general practices are well equipped with nursing support to demonstrate and observe the patients’ techniques. It would also be difficult to implement when patients’ load to a general practice clinic is overwhelming. Thus, a structured educational session involving audio-visual media with the patients to provide a direct demonstration would be an alternative to checking the inhaler technique. This is the first study that demonstrated inhaler technique by an audio-visual presentation at a general clinic and we have demonstrated the efficacy of this technique.
Our study showed that a structured educational session involving audio-visual media for patients with asthma had a high acceptance by the participants. Most of the patients found it interesting and observed the video at full length with full attention. As such, this method could be replicated in a broader context. Our study results show that the intervention may also be effective in children as asthma scores remarkably increased in the intervention group than in the control. In this study, we have found a relatively higher effect of the intervention on asthma scores in children than in adults. However, we did not obtain a statistically significant difference in the treatment effect in children, perhaps a result of a relatively low sample size undermining the study results. A future study with an adequate sample in this population may refute our result.
Strength and limitations
The main strength of our study is that it was a randomised intervention trial. Due to randomisation, we could avoid selection bias and control most of the baseline characteristics of the participants. Although asthma diagnosis and participants’ selection were made by the attending GP, there were dedicated nursing staff to deliver the intervention. The intervention video was short, simple, and in the participants’ native language, which could keep the participants’ attention while playing the video. The nursing staff communicated with the participants and gave reminders before 90 days to take the endline measurement. Attrition was limited to only one participant, which helped to retain our expected sample size and the power of the analysis. Asthma diagnosis by a physician also gives our study a precise technique to identify the study participants.
However, there are a few limitations as well. The study could not assess the participants’ compliance with the intervention while they were at home. The study was conducted during the COVID-19 pandemic. As such, repeated restrictions, including restricted movement and using face masks, might also influence the outcome of asthma. However, due to randomisation, we assume both groups were influenced equally so it did not affect the study outcome. We excluded several potential participants with asthma from participating in this study due to the presence of other co-morbidities, as outlined in our exclusion criteria. This exclusion may limit the generalisability of our findings. This study was conducted in a single general practice centre. Our sample population may represent only those people who regularly attend that clinic.
Conclusion
A structured audio-visual educational session for asthma during a general practice visit effectively improves the asthma status in the overall population irrespective of age. The participants well accepted the educational materials and techniques. Further study with scaling the intervention in different settings may strengthen the findings of our research.
Data availability
The data that support this study cannot be publicly shared due to ethical or privacy reasons and may be shared upon reasonable request to the corresponding author if appropriate.
References
Ahluwalia SK, Matsui EC (2011) The indoor environment and its effects on childhood asthma. Clinical Immunology 11, 137-143.
| Google Scholar |
AIHW (2020) Asthma. Australian Institute of Health Welfare, Canberra. Available at https://www.aihw.gov.au/reports/chronic-respiratory-conditions/asthma
AIHW (2021) Older Australians. Australian Institute of Health and Welfare, Canberra. Available at https://www.aihw.gov.au/reports/older-people/older-australians/contents/summary
Apelberg BJ, Aoki Y, Jaakkola JJK (2001) Systematic review: exposure to pets and risk of asthma and asthma-like symptoms. Journal of Allergy and Clinical Immunology 107, 455-460.
| Crossref | Google Scholar | PubMed |
Asthma Australia (2021) Asthma control questionnaire. Available at https://asthma.org.au/wp-content/uploads/2021/09/The-Asthma-Control-Test-ACT-PDF-with-infographic_2021.pdf [Accessed 1 March 2024]
Bainbridge R, Mccalman J, Clifford A, Tsey K (for the Closing the Gap Clearinghouse) (2015) Cultural competency in the delivery of health services for Indigenous people. (AIHW: Canberra) Available at https://doi.org/10.25816/5ec4ba84d1241
Baptist AP, Hao W, Song PX, Carpenter L, Steinberg J, Cardozo LJ (2020) A behavioral intervention can decrease asthma exacerbations in older adults. Annals of Allergy, Asthma & Immunology 124, 248-253.e3.
| Google Scholar | PubMed |
Barton C, Proudfoot J, Amoroso C, Ramsay E, Holton C, Bubner T, Harris M, Beilby J (2009) Management of asthma in Australian general practice: care is still not in line with clinical practice guidelines. Primary Care Respiratory Journal 18, 100-105.
| Crossref | Google Scholar | PubMed |
Bonini M, Di Paolo M, Bagnasco D, Baiardini I, Braido F, Caminati M, Carpagnano E, Contoli M, Corsico A, Del Giacco S, Heffler E, Lombardi C, Menichini I, Milanese M, Scichilone N, Senna G, Canonica GW (2020) Minimal clinically important difference for asthma endpoints: an expert consensus report. European Respiratory Review 29(156), 190137.
| Crossref | Google Scholar | PubMed |
Bowatte G, Lodge C, Lowe AJ, Erbas B, Perret J, Abramson MJ, Matheson M, Dharmage SC (2015) The influence of childhood traffic-related air pollution exposure on asthma, allergy and sensitization: a systematic review and a meta-analysis of birth cohort studies. Allergy 70, 245-256.
| Crossref | Google Scholar | PubMed |
Broglio K (2018) Randomization in clinical trials: permuted blocks and stratification. JAMA 319, 2223-2224.
| Crossref | Google Scholar | PubMed |
Carvalho Coelho AC, Barretto Cardoso LS, Souza-Machado Cd, Souza-Machado A (2016) The impacts of educational asthma interventions in schools: a systematic review of the literature. Canadian Respiratory Journal 2016, 1-14.
| Crossref | Google Scholar |
Clark NM, Mitchell HE, Rand CS (2009) Effectiveness of educational and behavioral asthma interventions. Pediatrics 123, S185-S192.
| Crossref | Google Scholar | PubMed |
Cochrane MG, Bala MV, Downs KE, Mauskopf J, Ben-Joseph RH (2000) Inhaled corticosteroids for asthma therapy: patient compliance, devices, and inhalation technique. Chest 117, 542-550.
| Crossref | Google Scholar | PubMed |
Dick S, Friend A, Dynes K, Alkandari F, Doust E, Cowie H, Ayres JG, Turner SW (2014a) A systematic review of associations between environmental exposures and development of asthma in children aged up to 9 years. BMJ Open 4, e006554.
| Crossref | Google Scholar |
Dick S, Doust E, Cowie H, Ayres JG, Turner S (2014b) Associations between environmental exposures and asthma control and exacerbations in young children: a systematic review. BMJ Open 4, e003827.
| Crossref | Google Scholar | PubMed |
Ducharme FM, Dell SD, Radhakrishnan D, Grad RM, Watson WTA, Yang CL, Zelman M (2015) Diagnosis and management of asthma in preschoolers: a Canadian Thoracic Society and Canadian Paediatric Society position paper. Paediatrics & Child Health 20, 353-361.
| Crossref | Google Scholar | PubMed |
Dunbar-Jacob J, Erlen JA, Schlenk EA, Ryan CM, Sereika SM, Doswell WM (2000) Adherence in chronic disease. Annual Review of Nursing Research 18, 48-90.
| Google Scholar | PubMed |
Eakin MN, Rand CS (2012) Improving patient adherence with asthma self-management practices: what works? Annals of Allergy, Asthma & Immunology 109, 90-92.
| Crossref | Google Scholar | PubMed |
Gibson PG, Coughlan J, Wilson AJ, Abramson M, Bauman A, Hensley MJ, Walters EH (2000) Self-management education and regular practitioner review for adults with asthma. Cochrane Database of Systematic Reviews 2002, Cd001117.
| Crossref | Google Scholar |
Gillette C, Rockich-Winston N, Kuhn JBA, Flesher S, Shepherd M (2016) Inhaler technique in children with asthma: a systematic review. Academic Pediatrics 16, 605-615.
| Crossref | Google Scholar | PubMed |
Hollenbach JP, Cloutier MM (2015) Childhood asthma management and environmental triggers. Pediatric Clinics of North America 62, 1199-1214.
| Crossref | Google Scholar | PubMed |
Horak F, Doberer D, Eber E, Horak E, Pohl W, Riedler J, Szépfalusi Z, Wantke F, Zacharasiewicz A, Studnicka M (2016) Diagnosis and management of asthma – statement on the 2015 GINA guidelines. Wiener klinische Wochenschrift 128, 541-554.
| Crossref | Google Scholar | PubMed |
Janssens T, Ritz T (2013) Perceived triggers of asthma: key to symptom perception and management. Clinical & Experimental Allergy 43, 1000-1008.
| Crossref | Google Scholar | PubMed |
Jenkins CR, Chang AB, Poulos LM, Marks GB (2009) Asthma in Indigenous Australians: so much yet to do for Indigenous lung health. Medical Journal of Australia 190(10), 530-531.
| Crossref | Google Scholar | PubMed |
Lau N, Norman A, Smith MJ, Sarkar A, Gao Z (2018) Association between traffic related air pollution and the development of asthma phenotypes in children: a systematic review. International Journal of Chronic Diseases 2018, 1-12.
| Crossref | Google Scholar |
Mensah GA, Kiley JP, Gibbons GH (2018) Generating evidence to inform an update of asthma clinical practice guidelines: perspectives from the National Heart, Lung, and Blood Institute. Journal of Allergy and Clinical Immunology 142, 744-748.
| Crossref | Google Scholar | PubMed |
Mims JW (2015) Asthma: definitions and pathophysiology. International Forum of Allergy & Rhinology 5, S2-S6.
| Google Scholar |
Mosnaim GS, Pappalardo AA, Resnick SE, Codispoti CD, Bandi S, Nackers L, Malik RN, Vijayaraghavan V, Lynch EB, Powell LH (2016) Behavioral interventions to improve asthma outcomes for adolescents: a systematic review. The Journal of Allergy and Clinical Immunology: In Practice 4, 130-141.
| Google Scholar | PubMed |
Mosnaim GS, Akkoyun E, Eng J, Shalowitz MU (2017) Behavioral interventions to improve asthma outcomes: a systematic review of recent publications. Current Opinion in Allergy & Clinical Immunology 17, 194-200.
| Crossref | Google Scholar | PubMed |
National Asthma Council Australia (2015) The hidden cost of asthma. Deloitte access economics. Available at https://www.nationalasthma.org.au/living-with-asthma/resources/health-professionals/reports-and-statistics/the-hidden-cost-of-asthma-2015
National Asthma Council Australia (2022a) Asthma action plans. National Asthma Council Australia. Available at https://www.nationalasthma.org.au/health-professionals/asthma-action-plans/asthma-action-plan-library [Accessed 28 September 2022]
National Asthma Council Australia (2022b) How-to videos. National Asthma Council Australia. Available at https://www.nationalasthma.org.au/living-with-asthma/how-to-videos [Accessed 29 September 2022]
Nucleus Medical Media (2022) Asthma. Nucleus Medical Media. Available at https://nmal.nucleusmedicalmedia.com/view-item?ItemID=75489 [Accessed 29 September 2022]
Papi A, Brightling C, Pedersen SE, Reddel HK (2018) Asthma. The Lancet 391, 783-800.
| Crossref | Google Scholar | PubMed |
Price D, Roche N, Virchow JC, Burden A, Ali M, Chisholm A, Lee AJ, Hillyer EV, Von Ziegenweidt J (2011) Device type and real-world effectiveness of asthma combination therapy: an observational study. Respiratory Medicine 105, 1457-1466.
| Crossref | Google Scholar | PubMed |
Reddel HK, Hurd SS, FitzGerald JM (2014) World Asthma Day. GINA 2014: a global asthma strategy for a global problem. The International Journal of Tuberculosis and Lung Disease 18, 505-506.
| Crossref | Google Scholar | PubMed |
Reddel HK, Sawyer SM, Everett PW, Flood PV, Peters MJ (2015) Asthma control in Australia: a cross-sectional web-based survey in a nationally representative population. Medical Journal of Australia 202, 492-496.
| Crossref | Google Scholar | PubMed |
Riera A, Ocasio A, Tiyyagura G, Thomas A, Goncalves P, Krumeich L, Ragins K, Trevino S, Vaca FE (2017) A web-based educational video to improve asthma knowledge for limited English proficiency Latino caregivers. Journal of Asthma 54, 624-631.
| Crossref | Google Scholar | PubMed |
Schatz M, Kosinski M, Yarlas AS, Hanlon J, Watson ME, Jhingran P (2009) The minimally important difference of the Asthma Control Test. Journal of Allergy and Clinical Immunology 124, 719-723.e1.
| Crossref | Google Scholar | PubMed |
Shah RF, Gupta RM (2017) Video instruction is more effective than written instruction in improving inhaler technique. Pulmonary Pharmacology & Therapeutics 46, 16-19.
| Crossref | Google Scholar | PubMed |
Shahunja KM, Sly PD, Begum T, Biswas T, Mamun A (2021) Family, neighborhood and psychosocial environmental factors and their associations with asthma in Australia: a systematic review and meta-analysis. Journal of Asthma 12, 2539-2552.
| Crossref | Google Scholar |
Sleath B, Ayala GX, Gillette C, Williams D, Davis S, Tudor G, Yeatts K, Washington D (2011) Provider demonstration and assessment of child device technique during pediatric asthma visits. Pediatrics 127, 642-648.
| Crossref | Google Scholar | PubMed |
Stanescu S, Kirby SE, Thomas M, Yardley L, Ainsworth B (2019) A systematic review of psychological, physical health factors, and quality of life in adult asthma. NPJ Primary Care Respiratory Medicine 29, 37.
| Crossref | Google Scholar | PubMed |
To T, Stanojevic S, Moores G, Gershon AS, Bateman ED, Cruz AA, Boulet L-P (2012) Global asthma prevalence in adults: findings from the cross-sectional world health survey. BMC Public Health 12, 204.
| Crossref | Google Scholar | PubMed |
Tripepi G, Chesnaye NC, Dekker FW, Zoccali C, Jager KJ (2020) Intention to treat and per protocol analysis in clinical trials. Nephrology (Carlton) 25, 513-517.
| Crossref | Google Scholar | PubMed |
Twisk J, Bosman L, Hoekstra T, Rijnhart J, Welten M, Heymans M (2018) Different ways to estimate treatment effects in randomised controlled trials. Contemporary Clinical Trials Communications 10, 80-85.
| Crossref | Google Scholar |
Urek MC, Tudorić N, Plavec D, Urek R, Koprivc-Milenović T, Stojić M (2005) Effect of educational programs on asthma control and qualitiy of life in adult asthma patients. Patient Education and Counseling 58, 47-54.
| Crossref | Google Scholar | PubMed |
Yang IV, Lozupone CA, Schwartz DA (2017) The environment, the epigenome, and asthma. Clinical Immunology 140, 14-23.
| Google Scholar |