Using a patient-reported outcome measure to assess quality of life at Western Sydney Sexual Health Centre
E. Mason A * , D. A. Lewis A B C , I. Zablotska A B C and L. Tomlins B
A * , D. A. Lewis A B C , I. Zablotska A B C and L. Tomlins B
A
B
C
Abstract
Attaining a good quality of life (QOL) is a priority for people living with HIV (PLHIV). We explored the interaction between QOL and the associated demographic, behavioural and clinical factors for PLHIV attending an outer-metropolitan clinical setting in Western Sydney, Australia. The clinic’s cohort of PLHIV is characterised by relatively high proportions of women, heterosexual men, and patients from culturally and linguistically diverse (CALD) communities.
We assessed QOL using the PozQol tool that is specifically designed for PLHIV. QOL scores and de-identified socio-demographic and clinical data were extracted from the electronic and paper medical records of PLHIV who completed a PozQol tool (September 2020–March 2022). We performed descriptive analyses and logistic regression to identify associations.
Among 188 patients, there were 77.7% men, 21.3% women, 1.1% transwomen; 67.0% were born overseas, 85.1% spoke English, 84.4% were Medicare-eligible, 85.9% were employed, 58.5% were diagnosed with HIV 6–20 years ago, and 33.0% within the past 5 years. Overall, 58.0% had a high or very high QOL. A low score in any domain was associated with Medicare-ineligibility. Low QOL scores in specific domains were associated with the following factors: health (being born overseas, having partners of both sexes), psychological (unemployment, having a mental health condition, having a viral load >20 copies/mL), social (unemployment), and functional (Medicare-eligibility, unemployment, having a viral load >20 copies/mL).
The PozQol tool has enhanced understanding of factors impacting on QOL for PLHIV attending our service in Western Sydney. Identifying patients with low QOL scores allows targeted clinical interventions to improve QOL, and re-alignment of clinical services to better support PLHIV.
Keywords: Australia, HIV, patient reported outcome measure, people living with HIV, PozQol, QOL, quality of life, Sydney.
Background
In 2016, the United Nations set the 90-90-90 targets as the world moved towards the elimination of HIV.1 These targets referred to the concept that by 2020, 90% of all people living with HIV (PLHIV) would be aware of their HIV status, 90% of those diagnosed with HIV would be taking anti-retroviral therapy (ART), and 90% of those on ART would have an undetectable viral load.1 Australia has since achieved and surpassed those goals, with 2021 data reporting that in Australia 91% of people know their status, 92% are receiving ART, and 98% are virally suppressed.2
Adherence to ART and viral suppression have been associated with a higher health-related quality of life (QOL) for PLHIV,3 with poor adherence and factors affecting this such as stigma and comorbid mental health issues associated with a lower QOL.3,4
However, even when achieving viral suppression, PLHIV continue to experience a lower QOL than the general population.5,6 In recognition of this, a ‘fourth 90’ target was proposed by Lazarus and colleagues in 2016 that 90% of PLHIV will also report a good health-related QOL.7 In Australia, the Eighth National HIV Strategy has identified QOL as a key priority for PLHIV with the goal that 75% of PLHIV will report a good QOL.8
Using empirical tools to measure QOL is vital in improving our current understanding of QOL experienced by PLHIV and adapting services to meet the goals of the National Strategy. One such tool is PozQol, which is an Australian developed, empirical, and validated tool specifically designed to measure QOL in PLHIV.9 PozQol aims to measure QOL across the domains of physical, psychological, social and functional health.9 In the Futures-10 study, PozQol was used to measure QOL in Australian PLHIV, with 71.8% reporting a ‘good’ QOL.10 Similar results using the PozQol tool were published in a recent study of PLHIV in Aotearoa New Zealand where 61% of respondents reported a high or very high QOL.11 These studies reported a relationship between QOL and factors such as stigma, poor mental and physical health, and unemployment.10,11
However, Australia’s national QOL indicator does not reflect the situation in all local health districts, which can vary greatly in terms of demographics and community profile. Western Sydney Sexual Health Centre (WSSHC) is a publicly funded sexual health clinic located in Western Sydney Local Health District (WSLHD), which is one of 15 local health districts in the NSW Health system. WSLHD is one of the State’s fastest growing areas with more than 1.3 million residents estimated by 2031.12 Residents come from diverse economic, social, and cultural backgrounds, and high levels of recent migration from neighbouring Asia-Pacific countries. As such, WSSHC provides an ideal clinical setting to develop and implement the PozQol tool as a means to determine the QOL of those PLHIV attending WSLHD’s Sexual Health service.
PozQol has been part of routine clinical care at WSSHC since September 2020. This research describes the number of PLHIV at WSSHC reporting a high or very high QOL and explore the relationship between PozQol scores and socio-demographic and clinical characteristics.
Materials and methods
The PozQoL tool was introduced into routine clinical care at WSSHC in September 2020. PozQol is an empirically validated 13-item tool, which measures health-related quality of life specifically for PLHIV across four domains: (1) health concerns; (2) psychological; (3) social; and (4) functional. The health concerns domain captures the individual’s perspective on their health including managing HIV. The psychological domain assesses the patient’s mood, coping, perspective on the future and self-esteem. The social domain captures perception of issues such as sense of belonging, social supports and stigma. The functional domain focuses on the patient’s perspective of their independence and standard of living. Total PozQol summary scores can range from 13 to 65. Scores in the psychological domain can range from 4 to 20, and scores in all other domains can range from 3 to 15. The overall score, and scores in each domain are categorised into low, medium, high and very high.13
Clinical staff (medical, nursing and social work) were trained in use of the tool prior to implementation and encouraged to complete it during routine clinic consultations for patients attending for HIV care. During the appointment, staff would provide a brief explanation of the tool, and patients could opt to complete this in the consultation room with a pen and paper version. Non-English-speaking patients could complete the tool via a formally translated version if available from the PozQol website or with the assistance of an interpreter. Staff would calculate and record the summary scores. Summary scores were used clinically as they were considered simpler for staff to calculate during consultations. The administering staff member would then discuss the scores with the patient and could make referrals based on these; for example, to the social work team on site, community organisations or peer support programs. The completed paper-based tools were filed in patient’s paper files and scanned into the electronic medical records.
A refresher education session for staff was held 12 months after the tool’s introduction. Activities to increase the use of the tool included verbal reminders at daily clinical meetings, written reminders added to the appointment system, and updates sent to clinicians on the proportion of patients allocated to their care who had completed at least one PozQol tool.
All patient records with tools completed between September 2020 and March 2022 were retrospectively reviewed. For each patient who had completed a tool during the specified period, PozQol scores, socio-demographic and clinical data were extracted into a Microsoft Excel spreadsheet and de-identified. The dataset was retained in Microsoft Excel, in the secure NSW Health Microsoft Teams application.
Extra variables included demographics such as age, country of birth, Medicare eligibility, Indigenous status (self-identification of Aboriginal and/or Torres Strait Islander heritage) and language (preferred language for consults, listed as English if interpreter not required). Demographic data was self-reported at the time of registration for creation of the medical record, with updates to details such as Medicare eligibility updated as needed. Clinical variables included time since HIV diagnosis, most recent CD4 count and viral load, presence of both HIV-related and non-HIV-related comorbidities, and a history of ever being diagnosed with a mental health condition. Behavioural data such as gender of partners and a history of ever using injecting drugs were collected. These variables were selected as they were able to be collected retrospectively from existing routinely collected data from medical records and based on important factors associated with QOL in the existing literature. Outcomes of interest were the PozQol scores. An overall low QOL was classified as an overall PozQol summary score of ≤36. Summary scores in each domain were categorised as low (≤10 for psychological domain, ≤9 for functional domain and ≤6 for the social and health concerns domains), or not low (moderate, high, very high) according to the scoring system of the PozQol tool.13 Where there was missing data from at least one domain, the score from that domain and the overall score were not able to be calculated. Therefore, those with a score missing in a specific domain were excluded from analysis of that specific domain and from calculations of the overall score. The authors selected these categories to compare those that scored low and those that did not more readily. A composite outcome of a low score in any domain was created.
Ethics approval was granted by the Western Sydney Local Health District Research Ethics Committee (2021/ETH00587).
Statistical analysis
Data analyses were completed in Stata 14 (StataCorp. 2015. Stata Statistical Software: Release 14, College Station, TX, USA). We report descriptive statistics on the sample. Bivariate logistic regression was used to determine associations between patient characteristics and low scores in each individual domain. Multivariate logistic regression was undertaken to determine independent relationships between a low score in any domain, and patient characteristics, accounting for potential confounders.
Multivariate regression models were constructed using a standard approach of the forward stepwise model selection and included variables that were significantly associated with the outcome of interest in bivariate analysis. To determine statistical significance, we used the Type I error threshold of 5% (P-value of 0.05). The final model included age, Medicare eligibility, employment status and viral load. For the associations of interest, we report odds ratios for the bivariate analysis (OR), adjusted odds ratios for the multivariate analysis (aOR) and 95% confidence intervals (95% CI).
Results
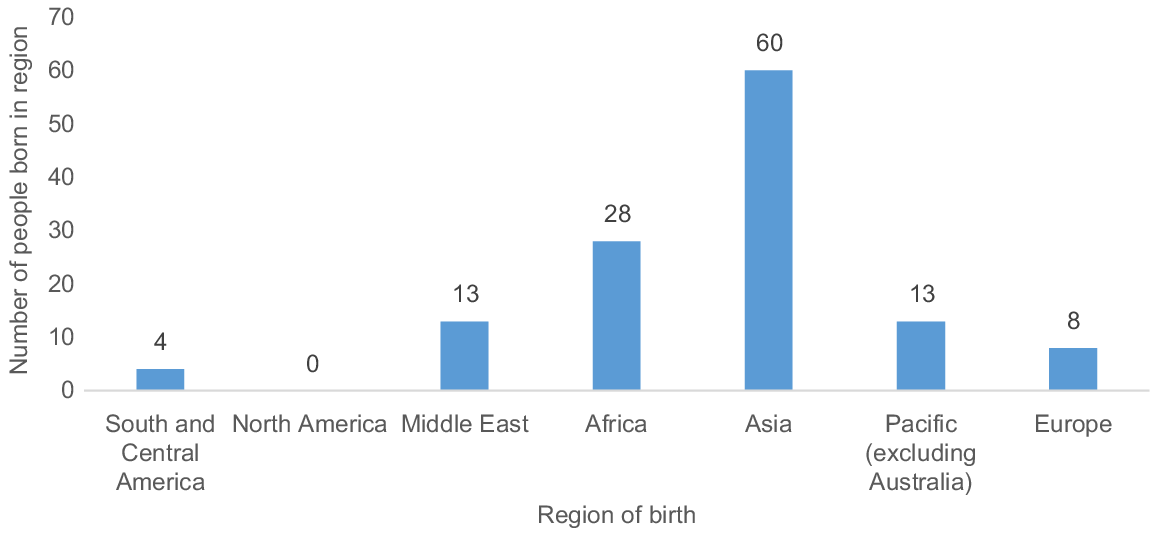
A total of 188 patients completed a PozQol tool over the 19-month study period. This represents 48.6% of the total cohort of PLHIV at WSSHC engaged in care at this time. Those engaged in care at WSSHC could be expected to attend once every 4–6 months. Only two patients had a missing score in any domain. The socio-demographic characteristics are in Table 1. The median age was 42 years (range 20–71 years). The majority were men (146, 77.7%); in addition, there were 40 (21.3%) women and two (1.1%) transwomen included. Around two-thirds (126, 67.0%) were born outside Australia, however, most spoke English (160, 85.1%) and most were eligible for Medicare (157, 84.4%). For those born outside Australia, there were 43 different countries of birth reported, the most common being the Philippines (19, 15.0%), Thailand (10, 7.9%) and China (10, 7.9%). Of the 126 patients born overseas, 60 (47.6%) were born in Asian countries, 28 in African countries (22.0%), 13 in the Pacific region (10.2%), and 13 in the Middle East (10.2%) (Fig. 1).
| N | % | ||
|---|---|---|---|
| Age, median (range): 42 years (20–71) | |||
| Gender | |||
| Male | 146 | 77.7 | |
| Female | 40 | 21.3 | |
| Transwomen | 2 | 1.1 | |
| Indigenous status | |||
| No | 185 | 98.4 | |
| Yes | 3 | 1.6 | |
| Born in Australia | |||
| No | 126 | 67.0 | |
| Yes | 62 | 33.0 | |
| Language spoken at home | |||
| English | 160 | 85.1 | |
| Other | 28 | 14.9 | |
| Medicare eligible | |||
| No | 29 | 15.6 | |
| Yes | 157 | 84.4 | |
| Employed | |||
| No | 25 | 14.1 | |
| Yes | 152 | 85.9 | |
| Behavioural characteristics | |||
| Partners | |||
| Same sex | 91 | 48.4 | |
| Opposite sex | 75 | 39.9 | |
| Both sexes | 22 | 11.7 | |
| Injecting drug use | |||
| No | 172 | 93.0 | |
| Yes | 13 | 7.0 | |
Most patients reported being employed (152, 85.9%). Just under half had partners of the same sex only (91, 48.4%), a small number had partners of both sexes (22, 11.7%), and the remainder had partners of the opposite sex only (75, 39.9%). A small number of patients (13, 7.0%) reported any current or past history of injecting drug use.
The clinical characteristics are in Table 2. Around one-third of patients had been diagnosed with HIV in the past 5 years (62, 33.0%). Most patients had an undetectable viral load of ≤20 copies (173, 92%), and only one patient had a viral load >200 copies/mL. Most patients had a CD4 count >500 cells/μL (157, 83.5%) and most reported no history of any HIV-related disease or complications (142, 75.5%). Almost two-thirds reported one or more comorbidity (120, 63.8%), and just under a quarter reported a history of mental health conditions (43, 22.9%).
| N | % | ||
|---|---|---|---|
| Time since HIV diagnosis | |||
| 0–5 years | 62 | 33.0 | |
| 6–20 years | 110 | 58.5 | |
| >20 years | 16 | 8.5 | |
| Duration of anti-retroviral therapy | |||
| 0–5 years | 69 | 37.5 | |
| 6–20 years | 102 | 55.4 | |
| >20 years | 13 | 7.1 | |
| Most recent viral load (copies/mL) | |||
| ≤20 | 173 | 92.0 | |
| 21–200 | 14 | 7.5 | |
| >200 | 1 | 0.5 | |
| Most recent CD4 count (cells/μL) | |||
| ≤200 | 1 | 0.5 | |
| 201–500 | 3 | 16 | |
| >500 | 157 | 83.5 | |
| HIV-related disease | |||
| No | 142 | 75.5 | |
| Yes | 46 | 24.5 | |
| Other comorbidities | |||
| No | 68 | 36.2 | |
| Yes | 120 | 63.8 | |
| Mental health comorbidities | |||
| No | 145 | 77.1 | |
| Yes | 43 | 22.9 | |
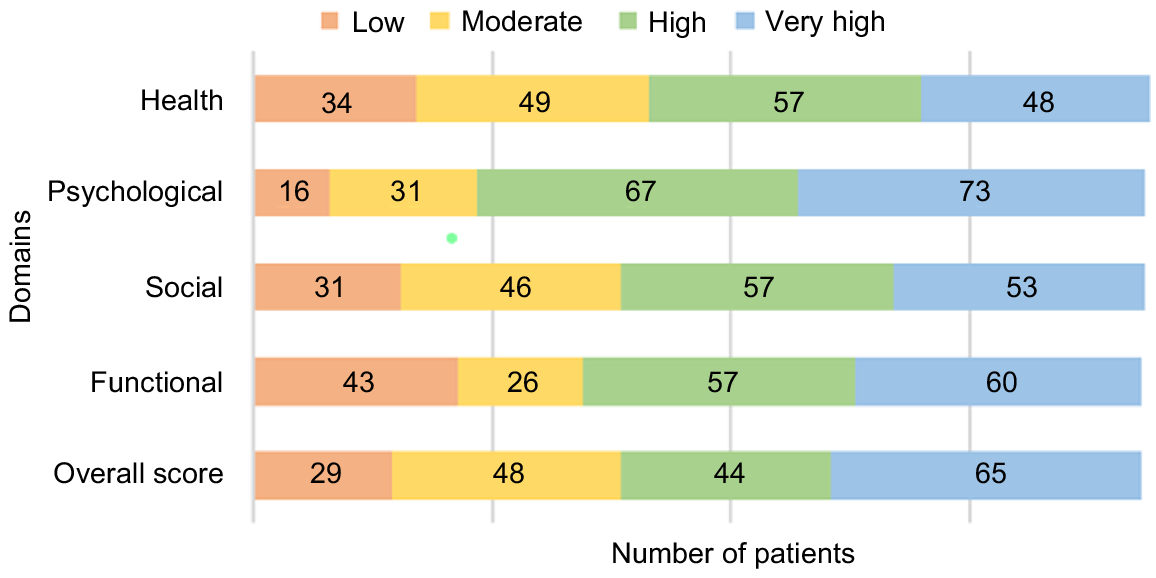
The mean overall PozQol score was 47.7, with scores ranging from 19 to 65. Overall, 109 (58.0%) patients had total PozQol scores in the high or very high category. There were 29 (15.4%) patients who had an overall low PozQol score. The distribution of scores by PozQol domains is in Fig. 2. Over one-third of patients (65, 34.6%) had a low score in any domain.
PozQol scores across four domains of heath, psychological, social, and functional. Health concerns: Low, QOL ≤ 6; Moderate, QOL 7–9: High, QOL 10–12; Very high,, QOL ≥ 13. Psychological: Low QOL ≤ 10; Moderate, QOL 11–13; High, QOL 14–16; Very high, QOL ≥ 17. Social: Low, QOL ≤ 6; Moderate, QOL 7–9: High, QOL 10–12; Very high, QOL ≥ 13. Functional: Low, QOL < 9; Moderate, QOL 10–11; High, QOL 12–14; Very high, QOL ≥ 15. Overall PozQol score: Low, QOL ≤ 36; Moderate, QOL 37–45; High, QOL 46–53; Very high, QOL ≥ 54.
Low scores in the health domain were more likely in patients who were born overseas (OR = 2.67; 95% CI, 1.04–6.83), and those reporting partners of both sexes (OR = 3.07; 95% CI, 1.04–9.08). Low scores in the psychological domain were more likely in patients who were unemployed (OR = 6.14; 95% CI, 2.04–18.48), had a viral load of >20 copies/mL (OR = 4.85; 95% CI, 4.85–17.54) and who had a history of a mental health condition (OR = 3.89; 95% CI, 1.36–11.08). A low score in the social domain was more likely in patients who were unemployed (OR = 4.37; 95 %CI, 1.73–11.05). A low score in the functional domain was more likely in patients who were Medicare-ineligible (OR = 3.02; 95%CI, 1.30–7.04), and those who were unemployed (OR = 2.78; 95% CI, 1.13–6.82) (Table 3).
| Health | Psychological | Social | Functional | ||
|---|---|---|---|---|---|
| Odds ratio low score by domain (95% confidence interval) | |||||
| Socio-demographic characteristics | |||||
| Age, median (range): 42 years (20–71) | 0.98 (0.95–1.01) | 1.03 (0.99–1.07) | 1.01 (0.98–1.04) | 1.00 (0.97–1.03) | |
| Gender | |||||
| Male | 1.00 | 1.00 | 1.00 | 1.00 | |
| Female | 0.74 (0.28–1.94) | 1.11 (0.37–3.39) | 1.18 (0.51–2.71) | 1.05 (0.49–2.24) | |
| Born in Australia | |||||
| Yes | 1.00 | 1.00 | 1.00 | 1.00 | |
| No | 2.67 (1.04–6.83) | 0.79 (0.27–2.28) | 1.48 (0.62–3.53) | 1.56 (0.73–3.37) | |
| Language spoken at home | |||||
| English | 1.00 | 1.00 | 1.00 | 1.00 | |
| Other | 2.06 (0.82–5.18) | 0.80 (0.17–3.71) | 1.88 (0.72–4.89) | 1.84 (0.76–4.46) | |
| Medicare eligible | |||||
| Yes | 1.00 | 1.00 | 1.00 | 1.00 | |
| No | 2.38 (0.97–5.82) | 0.75 (0.16–3.50) | 0.76 (0.25–2.38) | 3.02 (1.30–7.04) | |
| Employed | |||||
| Yes | 1.00 | 1.00 | 1.00 | 1.00 | |
| No | 1.21 (0.42–3.52) | 6.14 (2.04–18.48) | 4.37 (1.73–11.05) | 2.78 (1.13–6.82) | |
| Behaviour | |||||
| Partners | |||||
| Same sex | 1.00 | 1.00 | 1.00 | 1.00 | |
| Opposite sex | 1.65 (0.72–3.77) | 0.80 (0.27–2.37) | 2.17 (0.94–4.98) | 1.43 (0.68–2.97) | |
| Both sexes | 3.07 (1.04–9.08) | 0.43 (0.05–3.62) | 1.15 (0.29–4.52) | 1.52 (0.52–4.44) | |
| Injecting drug use | |||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | |
| Yes | 1.36 (0.35–5.25) | 0.93 (0.11–7.72) | 0.93 (0.20–4.42) | 2.25 (0.69–7.28) | |
| Health-related | |||||
| Time since HIV diagnosis | |||||
| 0–5 years | 1.00 | 1.00 | 1.00 | 1.00 | |
| 6–20 years | 0.93 (0.42–2.05) | 1.43 (0.43–4.75) | 1.47 (0.61–3.58) | 1.22 (0.57–2.58) | |
| >20 years | 0.60 (0.12–2.98) | 2.04 (0.34–12.26) | 1.53 (0.36–6.58) | 0.85 (0.21–3.44) | |
| Most recent viral load (copies/mL) | |||||
| ≤20 | 1.00 | 1.00 | 1.00 | 1.00 | |
| >20 copies | 2.48 (0.79–7.80) | 4.85 (1.34–17.54) | 2.81 (0.89–8.88) | 2.42 (0.81–7.22) | |
| HIV-related disease | |||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | |
| Yes | 0.61 (0.24–1.58) | 2.63 (0.92–7.53) | 0.54 (0.19–1.50) | 1.24 (0.57–2.68) | |
| Other comorbidities | |||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | |
| Yes | 0.57 (0.27–1.22) | 4.29 (0.95–19.50) | 0.86 (0.39–1.91) | 0.72 (0.36–1.45) | |
| Mental health condition | |||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | |
| Yes | 0.85 (0.34–2.11) | 3.89 (1.36–11.08) | 1.47 (0.62–3.48) | 1.40 (0.64–3.04) | |
Bold data represents significant associations.
A low score in any domain on bivariate regression was more likely in patients who were Medicare ineligible (OR = 2.71; 95% CI, 1.21–6.07), unemployed (OR = 2.42; 95% CI, 1.03–5.70), and had a viral load ≥20 copies/mL (OR = 3.13; 95% CI, 1.06–9.24). On multivariate regression analysis, a low score in any domain was found to be more likely in patients who were Medicare ineligible (aOR = 3.58; 95% CI, 1.43–8.97) and patients with a viral load of ≥20 copies/mL (aOR = 3.76; 95% CI, 1.16–12.23) (Table 4).
| N (total) | N (%) (low in any domain) | Bivariate regression – low in any domain Odd ratio (95% confidence interval) | Multivariate regression – low in any domain Adjusted odds ratio (95% confidence interval) | ||
|---|---|---|---|---|---|
| Socio-demographic characteristics | |||||
| Age, median (range): 42 years (20–71) | 1.00 (0.97–1.02) | 1.00 (0.97–1.04) | |||
| Gender | |||||
| Male | 146 | 51 (34.9) | 1.00 | ||
| Female | 40 | 14 (35.0) | 0.87 (0.44–1.71) | ||
| Born in Australia | |||||
| Yes | 126 | 48 (38.1) | 1.00 | ||
| No | 62 | 17 (27.4) | 1.63 (0.84–3.16) | ||
| Language spoken at home | |||||
| English | 28 | 14 (50.0) | 1.00 | ||
| Other | 160 | 51 (31.9) | 2.14 (0.95–4.81) | ||
| Medicare eligible | |||||
| Yes | 157 | 49 (31.2) | 1.00 | 1.00 | |
| No | 29 | 16 (55.2) | 2.71 (1.21–6.07) | 3.58 (1.43–8.97) | |
| Employed | |||||
| Yes | 152 | 47 (30.9) | 1.00 | 1.00 | |
| No | 25 | 13 (52.0) | 2.42 (1.03–5.70) | 2.30 (0.90–5.90) | |
| Behaviour | |||||
| Partners | |||||
| Same sex | 91 | 28 (30.8) | 1.00 | ||
| Opposite sex | 75 | 30 (40.0) | 1.50 (0.79–2.85) | ||
| Both sexes | 22 | 7 (31.8) | 1.05 (0.39–2.86) | ||
| Injecting drug use | |||||
| No | 172 | 58 (33.7) | 1.00 | ||
| Yes | 13 | 6 (46.2) | 1.68 (0.54–5.24) | ||
| Health-related | |||||
| Time since HIV diagnosis | |||||
| 0–5 years | 62 | 17 (27.4) | 1.00 | ||
| 6–20 years | 110 | 43 (39.1) | 1.70 (0.86–3.34) | ||
| >20 years | 16 | 5 (31.3) | 1.20 (0.36–3.98) | ||
| Most recent viral load (copies/mL) | |||||
| ≤20 | 173 | 56 (32.4) | 1.00 | 1.00 | |
| >20 copies | 15 | 9 (60.0) | 3.13 (1.06–9.24) | 3.76 (1.16–12.23) | |
| HIV-related disease | |||||
| No | 142 | 47 (33.1) | 1.00 | ||
| Yes | 46 | 18 (39.1) | 1.30 (0.65–2.58) | ||
| Other comorbidities | |||||
| No | 68 | 25 (36.8) | 1.00 | ||
| Yes | 120 | 40 (33.3) | 0.86 (0.46–1.60) | ||
| Mental health condition | |||||
| No | 145 | 47 (32.4) | 1.00 | ||
| Yes | 43 | 18 (41.9) | 1.50 (0.75–3.02) | ||
Bold data represents significant associations.
Discussion
This study offers an insight into QOL for Australian PLHIV in a clinic-based setting with a unique culturally and linguistic diverse population. Less than two-thirds (58%) of patients in this study reported a high or very high QOL. This is well below the 75% goal set out in the Australian National Strategy,8 and far below the goal that 90% of PLHIV should enjoy a good health-related QOL.7 This is congruent with recent research using the PozQol tool in Aotearoa New Zealand where similar proportions of PLHIV reported a high or very high QOL,11 but well below the 71% reporting a good quality of life in the Australian Futures-10 study.10 It should be noted that the population of patients at WSSHC varies from those included in the Futures-10 study, which accounts for national reporting of QOL among PLHIV. Compared to the Futures-10 cohort, the population included in our study is younger, includes a greater proportion of women (21.3% vs 9.6%) and a lesser proportion of Australian-born PLHIV (33.0% vs 72.2%). The socio-demographic characteristics associated with a low QOL such as unemployment, physical and mental health were consistent with findings in existing Australian literature.14–17 The Futures-10 study analyses scores using the mean PozQol score,10 rather than the summary score, meaning the threshold for classifying QOL as ‘good’ slightly differs between the Futures-10 study and our study.
Medicare is Australia’s universal health insurance scheme that provides free or low-cost health services to citizens, permanent residents, and some temporary residents dependent on visa class. Medicare-eligibility was an important factor in our study, with Medicare-ineligible patients more likely to have low QOL scores in any PozQol domain. While most people in Australia are currently able to access HIV-related care and medications with no cost in Australia, additional challenges with immigration such as visa concerns, language barriers and social isolation have the potential to impact QOL.17 An Australian study has shown that patients without Medicare access are highly motivated to engage in treatment and adhere to medications;18 however, barriers such as stigma, and fear of visa cancellation may affect people’s ability to engage in care.17 In 2023 the federal government began funding to provide ART to all Medicare-ineligible PLHIV, where previously these patients could access only these medications through self-importation, drug company donation or enrolment in clinical trials. It remains to be seen if the recent change in funding arrangements for HIV antiretroviral provision for Medicare-ineligible individuals, attending care within Australia, will impact on their QoL scores in the future.19
Patients who had a viral load of more than 20 copies/mL were more likely to have a low score in any domain. The majority of these patients had a viral load between 21 and 200 copies, indicating low level viraemia, which has been associated with suboptimal adherence in the literature.20,21 Many factors affecting adherence such as the experience of stigma and mental health comorbidities have also been shown to impact QOL,3,5 which may explain this finding. However, even when PLHIV achieve viral suppression, their health-related QOL remains lower than the general population.5
Employment is well documented to be associated with an improved QOL for PLHIV.6,10,15,22 Employment status is linked to socio-economic status and has been shown to be positively associated with improved physical and mental health.6,22 It is possible that those experiencing better overall health and QOL are more likely to be employed, and employment itself provides structure, meaning and social connectedness, all of which contribute further to QOL.6
In our sample, people born overseas were more likely to report a low QOL in the health domain. People born overseas, particularly gay and bisexual men, constitute a large and increasing portion of PLHIV in Australia and face many challenges navigating the health system to access HIV-related care including language barriers, financial concerns and Medicare eligibility.17,23 These challenges may be magnified at the intersections of gender, religion and sexuality, and are often further compounded by stigma and discrimination.17
To improve understanding of QOL for PLHIV at WSSHC in the future, a prospective study design whereby the PozQol tool is embedded into routine care and completed with all patients at regular intervals would be beneficial. This would allow assessment of important indicators of QOL such as the experience of stigma and discrimination, and to explore other aspects of QOL such as social connectedness and self-rated physical and mental health. It would also allow patients and clinicians to track QOL together over time and reflect on changes in QOL following interventions. PozQol asks questions not necessarily covered in routine clinical consults, enabling patients to discuss issues relating to QOL with clinicians. In doing so, it may empower patients to more deeply and actively engage in navigating their own healthcare journey.
Future studies using objective tools such as PozQol should focus on collecting data from a broad range of settings to improve our understanding of QOL for PLHIV in Australia. A particular focus should be on PLHIV under-represented in current research such as those who are overseas born or from culturally and linguistically diverse backgrounds, women, and heterosexuals. Targeted research at individual clinics such as WSSHC could assist in reaching some of these under-represented populations who may be less likely to be engaged with community organisations and initiatives. This may also contribute to a greater understanding of targeting HIV prevention strategies to specific areas such as Western Sydney, where there has not been the same success in decreasing HIV diagnoses as seen in inner city areas.24
Further research building an understanding of evidence-based interventions to improve QOL in PLHIV, such as peer navigation programs,25 will promote re-alignment of services and resource allocation to provide holistic care for PLHIV. Digital resources such as those found on the PozQol website13 as well as the use of digital scales would facilitate more widespread use of the PozQol tool by increasing accessibility.
Limitations
While this study offers a unique insight into QOL for PLHIV attending a clinic in Western Sydney, the authors recognise there are limitations of our study. The fact that this study was conducted within one Australian publicly funded sexual health service does not mean the findings are generalisable to other HIV treatment facilities across the country.
We acknowledge that the number of PLHIV who completed tools represented under half the total cohort of PLHIV retained in care at WSSHC, which may have resulted in a selection bias. As the sample and total cohort were comparable in several baseline characteristics e.g. gender, country of birth and preferred language (data not shown), the sample may be broadly representative of WSSHC’s patient population in demographic terms. However, to further examine potential bias, we also assessed the complexity of those patients who completed the PozQol tool as well as those who did not, through review of an internal clinic database which categorises patients into low, medium and high clinical complexity. In doing so, we found that patients of a higher clinical complexity were less likely to have completed a tool compared to patients of a low clinical complexity which is likely driven by time limitations and competing clinical priorities (data not shown). The reduced sample size was likely impacted by the challenges of introducing a new clinical tool to an already busy service. We acknowledge that the tool was introduced and used during the height of the COVID-19 pandemic, when face-to-face appointments were limited, thereby limiting opportunities to complete the tool.
In addition, staff may have found it easier to introduce the tool in clinical practice with patients with proficient English, as allocated appointment times may not have allowed for completion of the tool with an interpreter. To address the low response rate, we implemented verbal reminders at daily clinical meetings, reminders on the appointment booking system and provided feedback to clinicians on the overall response rate and the proportion of patients in their care who had completed a PozQol tool.
Lastly, the retrospective design of this study only allowed collection of data that was available as part of routine clinical care. This means that important factors affecting QOL such as stigma and discrimination were not able to be studied.
Conclusion
In conclusion, the data from our study suggests that patients at WSSHC experience an overall substantially lower QOL compared to the QOL goal identified in the National HIV Strategy and compared to the nationally collected data reported in Futures-10. Use of a standardised tool such as PozQol more broadly in clinical settings within Australia would improve overall understanding of QOL among PLHIV at a service level and allow the deployment of localised interventions to improve this. If this clinic-based data could be captured and collated on a larger scale, it may allow greater understanding of QOL for groups under-represented in the national survey data such as Futures-10 and provide much needed detail at the local level. At a policy level more comprehensive data could be used to inform policies, programs and funding aimed at improving QOL for PLHIV. Clinical services may utilise PozQol to tailor service provision, clinical care and referral pathways to the needs of their patient population and improve QOL through a patient-centred care approach. Finally, at an individual level, PozQol can offer patients valuable insight into their quality of life over time. This insight may empower individuals to actively engage with health services and feel a greater sense of ownership over their health and wellbeing.
Data availability
The data that support this study cannot be publicly shared due to ethical or privacy reasons and may be shared upon reasonable request to the corresponding author if appropriate.
References
1 UNAIDS. 90-90-90: an ambitious treatment target to help end the AIDS epidemic. Joint United Nations Programme on HIV/AIDS. Available at https://www.unaids.org/en/resources/documents/2017/90-90-90 [cited 4 September 2022]
3 Oguntibeju OO. Quality of life of people living with HIV and AIDS and antiretroviral therapy. HIV AIDS 2012; 4: 117-124.
| Crossref | Google Scholar | PubMed |
4 Katz IT, Ryu AE, Onuegbu AG, Psaros C, Weiser SD, Bangsberg DR, Tsai AC. Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. J Int AIDS Soc 2013; 16: 18640.
| Crossref | Google Scholar | PubMed |
5 Miners A, Phillips A, Kreif N, et al. Health-related quality-of-life of people with HIV in the era of combination antiretroviral treatment: a cross-sectional comparison with the general population. Lancet HIV 2014; 1: e32-e40.
| Crossref | Google Scholar | PubMed |
6 Degroote S, Vogelaers D, Vandijck DM. What determines health-related quality of life among people living with HIV: an updated review of the literature. Arch Public Health 2014; 72: 40.
| Crossref | Google Scholar |
7 Lazarus JV, Safreed-Harmon K, Barton SE, Costagliola D, Dedes N, del Amo Valero J, Gatell JM, Baptista-Leite R, Mendão L, Porter K, Vella S, Rockstroh JK. Beyond viral suppression of HIV–the new quality of life frontier. BMC Med 2016; 14(1): 94.
| Crossref | Google Scholar |
9 Brown G, Mikołajczak G, Lyons A, et al. Development and validation of PozQoL: a scale to assess quality of life of PLHIV. BMC Public Health 2018; 18: 527.
| Crossref | Google Scholar | PubMed |
10 Norman T, Power J, Rule J, Chen J, Bourne A. HIV futures 10: quality of life among people living with HIV in Australia. Monograph series number 134. Australian Research Centre in Sex, Health and Society, La Trobe University; 2022. Available at https://www.latrobe.edu.au/arcshs/work/hiv-futures-10
11 McAllister S, Iosua E, Hollingshead B, Bruning J, Fisher M, Olin R, Mukakayange J, Greenwood C, de Gouw A, Priest P. Quality of life in people living with HIV in Aotearoa New Zealand: an exploratory cross-sectional study. AIDS Care 35(10): 1518-1525.
| Crossref | Google Scholar |
12 Western Sydney Local Health District. About us. 2024. Updated. Available at https://www.wslhd.health.nsw.gov.au/About-Us [26 May 2024]
13 Australian Research Centre in Sex, Health and Society, La Trobe University. PozQol: Valuing quality of life among people with HIV. 2023. Available at https://www.pozqol.org/ [cited 24 July 2023]
14 Mao L, Kidd MR, Rogers G, Andrews G, Newman CE, Booth A, Saltman DC, Kippax SC. Social factors associated with Major Depressive Disorder in homosexually active, gay men attending general practices in urban Australia. Aust N Z J Public Health 2009; 33: 83-86.
| Crossref | Google Scholar | PubMed |
15 Herrmann S, McKinnon E, Hyland NB, Lalanne C, Mallal S, Nolan D, Chassany O, Duracinsky M. HIV-related stigma and physical symptoms have a persistent influence on health-related quality of life in Australians with HIV infection. Health Qual Life Outcomes 2013; 11: 56.
| Crossref | Google Scholar | PubMed |
17 Ziersch A, Walsh M, Baak M, Rowley G, Oudih E, Mwanri L. “It’s not an acceptable disease”: a qualitative study of HIV-related stigma and discrimination and impacts on health and wellbeing for people from ethnically diverse backgrounds in Australia. BMC Public Health 2021; 21: 779.
| Crossref | Google Scholar | PubMed |
18 Herrmann S, Wardrop J, John M, Gaudieri S, Lucas M, Mallal S, Nolan D. The impact of visa status and Medicare eligibility on people diagnosed with HIV in Western Australia: a qualitative report. Sex Health 2012; 9(5): 407-413.
| Crossref | Google Scholar | PubMed |
19 AFAO [Media release]. World AIDS day marked by fresh commitment to end HIV transmission. 2021. Available at https://www.healthequitymatters.org.au/media-centre/world-aids-day-marked-by-fresh-commitment-to-end-hiv-transmission-2 [10 September 2022]
20 Konstantopoulos C, Ribaudo H, Ragland K, Bangsberg DR, Li JZ. Antiretroviral regimen and suboptimal medication adherence are associated with low-level human immunodeficiency virus viremia. Open Forum Infect Dis 2015; 2(1): ofu119.
| Crossref | Google Scholar |
21 Castillo-Mancilla JR, Morrow M, Coyle RP, Coleman SS, Zheng J-H, Ellison L, Bushman LR, Kiser JJ, Anderson PL, MaWhinney S. Low-level viremia is associated with cumulative adherence to antiretroviral therapy in persons with HIV. Open Forum Infect Dis 2021; 8(9): ofab463.
| Crossref | Google Scholar |
22 Rueda S, Raboud J, Mustard C, Bayoumi A, Lavis JN, Rourke SB. Employment status is associated with both physical and mental health quality of life in people living with HIV. AIDS Care 2011; 23: 435-443.
| Crossref | Google Scholar | PubMed |
23 Philpot SP, Aung E, Prestage G, Mao L, Chen T, Varma R, McIver R, Templeton DJ, Stackpool G, Robinson S, Carmody C, Power C, Grulich AE, Bavinton BR. Qualitative interviews with overseas-born gay and bisexual men recently diagnosed with HIV from non-English speaking countries: report of results. Sydney: Kirby Institute, UNSW Sydney; 2021. Available at https://doi.org/10.26190/3gk3-2z83
25 Krulic T, Brown G, Bourne A. A scoping review of peer navigation programs for people living with HIV: form, function and effects. AIDS Behav 2022; 26: 4034-4054.
| Crossref | Google Scholar | PubMed |