Young people’s preferences and motivations for STI partner notification: observational findings from the 2024 Sex, Drugs and Rock ‘n’ Roll survey
Stephanie C. Munari A B * , Jane L. Goller
A B * , Jane L. Goller  B , Jacqueline Coombe
B , Jacqueline Coombe  B , Ana Orozco
B , Ana Orozco  A , Sarah Eddy
A , Sarah Eddy  A , Jane Hocking
A , Jane Hocking  B , Margaret Hellard A C D E # and Megan S. C. Lim
B , Margaret Hellard A C D E # and Megan S. C. Lim  A B D #
A B D #
A
B
C
D
E
# Megan Lim and Margaret Hellard should be considered co-senior authors
Handling Editor: Weiming Tang
Abstract
Partner notification is an important step in the control of sexually transmissible infections (STIs). STIs remain at high rates among young people and can have serious reproductive consequences if left untreated. This study aimed to determine the preferences and motivations for partner notification among young people in Australia.
Quantitative and free-text qualitative data were collected through the 2024 Sex, Drugs and Rock ‘n’ Roll survey, an annual cross-sectional survey conducted among people aged 15–29 years old in Victoria, Australia. Respondents were recruited using convenience sampling through social media advertisements. Counts and proportions were calculated for the preferences and motivations for partner notification by regular and casual sexual partners as well as methods of communication. Inductive content analysis was used to analyse free-text responses.
The partner notification module of the survey was completed by 1163 people (60.3% identified as women, 40.2% as heterosexual) who provided a total of 1720 free-text responses. The majority, 1056 (90.8%) stated that they would notify their sexual partners and 1142 (98.2%) would want to be notified by a sexual partner of an STI risk. Qualitative analysis highlighted that respondents felt that partner notification is the responsible thing to do to look after their own and their partner’s health and protect others by reducing transmission. Few stated that embarrassment and fear of repercussions may make them less likely to notify their partners or that it would depend on the type of relationship. Most preferred to notify regular partners face-to-face (941, 80.9%) and casual partners via text message (785, 67.5%).
Almost all young people want to notify and be notified by partners of an STI risk regardless of age, gender or sexual identity. Tailoring resources by communication method and partner type is one way in which practitioners and public health authorities can support young people in undertaking this important step in STI control.
Keywords: HIV, partner notification, public health, Drugs and Rock ‘n’ Roll survey, sexual health, sexually transmissible infections, STI, Victoria, young people.
Introduction
Sexually transmissible infections (STIs) are highly common among young people aged 15 to 29 years. The most common bacterial STIs in this age group include chlamydia, gonorrhoea and syphilis.1 STIs can lead to adverse consequences for the infected individual, their sexual partners and unborn children, along with perceived feelings of stigma and shame.2 Partner notification is the process of informing the sexual partners of a person infected with an STI of a potential STI exposure, suggesting that the partner seek medical care for testing, treatment and prevention advice.3 Also known as ‘contact tracing’, partner notification is a crucial part of STI control, aiming to identify and treat undiagnosed infections, limit disease progression, prevent reinfection and interrupt transmission.3 Current Australian contact tracing guidelines recommend tracing back 6 months for chlamydia, 2 months for gonorrhoea and 3–12 months for syphilis, depending on the stage of infection. For human immunodeficiency virus (HIV), guidelines recommend tracing back either from the onset of risk behaviour (e.g. condomless sex) or last known negative test result.4
Partner notification can be patient- or provider-initiated. Providers (e.g. general practioners (GPs), sexual health physicians) have a legal responsibility to discuss partner notification with their patients. The extent of practitioner involvement will often depend on the type of infection. For example, health department contact tracers might provide support in the partner notification process for syphilis and HIV due to the increased risk of morbidity and mortality. Patient-initiated notification is often quicker and easier to perform, and though many patients are willing to notify partners themselves, rates of engagement in this process are often low.5 Though there are some resources available to assist patients in notifying partners, including anonymous web-based partner notification tools (e.g. the Australian website ‘Let Them Know’),6 few provide tailored information by communication method and partner type.7,8 Additionally, many patients experience barriers to partner notification, including fear of stigma, embarrassment, partner retaliation and loss of relationship.9 Hence, it is vital to best support young people in undertaking this essential, yet at times daunting, sexual health intervention.
Using findings from the 2024 annual Sex, Drugs and Rock ‘n’ Roll (SDRR) survey, this study aimed to understand young people’s preferences and motivations for partner notification, including preferred methods of notifying and being notified by sexual partners. Variation in notification preferences by regular and casual partner type were also explored. Findings are intended to inform the development of practical and tailored resources to assist young people in notifying sexual partners of an STI risk.
Methods
Setting and participants
SDRR is an annual online cross-sectional survey conducted by the Burnet Institute among young people in Victoria, Australia.10 Participants were eligible to complete the survey if they were aged between 15 and 29 years and resided in Victoria. Participants were provided with an information sheet and asked to give consent at the beginning of the survey, with the survey taking approximately 20 min to complete. All participants were given the option to enter a draw to win a cash prize of A$250 upon survey completion.
Recruitment and sampling
Recruitment was conducted online from March to May 2024 using convenience sampling, with distribution occurring predominantly through paid targeted social media advertisements on platforms such as Facebook and Instagram. Promotional materials, including flyers, were also shared through researcher networks, including on local university notice boards. Participants who had completed this survey in previous years and consented to be contacted for future research were sent an email invitation to complete the survey again. Once more than 1000 consented and completed responses were obtained, the survey was closed. To be included in this study, respondents needed to have consented to participate in the survey and completed their date of birth, gender and at least the partner notification module of the survey.
Data collection and management
Survey questions were developed by the authors and researchers at the Burnet Institute. There was a total of 61 questions on various health topics, including sexual health and behaviours, pornography use, alcohol and other drug use, and mental health, including 12 questions on partner notification for STIs. All survey questions were written in English. A complete list of survey questions can be found in the supplementary material. Ethics approval was obtained from the Alfred Hospital Research Ethics Committee (project number 326/08). The survey was administered via the secure Research Electronic Data Capture11 and data were stored on secure Burnet Institute password-protected servers.
Variables
Demographic variables included age (15–19, 20–24, 25–29 years), gender (woman, man, other) and sexual identity (heterosexual, gay, homosexual or lesbian, bisexual, other). Participants who selected more than one sexual identity and/or any combination of ‘pansexual’, ‘asexual’, ‘queer’, ‘questioning’, ‘don’t know’, ‘don’t label’, ‘did not say’ or ‘other’, were categorised as ‘other’. Health seeking behaviours included the derived variables of having visited a health service (e.g. GP or sexual health clinic) in the last 12 months and having had an STI test in the last 6 months.
Outcome variables included intentions and motivations for notifying and being notified by current and past sexual partners. Using hypothetical scenarios, respondents were asked:
If they would notify or want to be notified
Why they would notify or want to be notified
How they would prefer to notify or be notified
A table listing several communication methods for notifying and being notified was provided, and respondents were asked to select all preferred options. Each outcome was also separated by regular and casual sex partner, where regular sex partner was defined as ‘a boyfriend, girlfriend or in a relationship’, and casual sex partner defined as ‘partners like a f**k buddy, one-night stand, friends with benefits or just seeing someone’.
Data analysis
Descriptive statistics, including counts and proportions, were used to describe participants’ intention to notify and be notified by sexual partners of an STI risk. A logistic regression model was used to determine differences in demographic characteristics associated with intentions for notification. Counts and proportions were also calculated for respondents who chose at least each communication method (defined as ‘acceptable’) and only each communication method (defined as ‘preferred’). Quantitative data analyses were performed using Stata 18 software (StataCorp. 2023, Stata Statistical Software: Release 18, College Station, TX: StataCorp LLC). Free-text responses were imported into NVivo 14 (Lumivero, release 14.24.0) data management software and were analysed using an inductive content analysis (ICA) approach.12 The first step of the ICA process involved reading all transcripts to become familiar with the data. Step two involved coding the broad categories of content (‘big-picture meaning units’12) within the transcript text. Step three involved reviewing the text within each of the big-picture codes to create sub-categories representing the varied ideas within each category. Step four included further refinement of each sub-category, where some sub-categories were collapsed or consolidated within other more relevant sub-categories to capture the richness of the data and minimise repetition. The final step involved synthesising and interpreting the data to create meaning. Preliminary codes for the first 100 responses were discussed with authors JC and JG, with no discrepancies identified. The framework was then refined upon repeat discussion to form the final set of codes.
Results
A total of 2720 people commenced the survey of which 1007 were excluded, as they did not provide consent; 246 participants were excluded due to incomplete year of birth or sex responses; and 304 participants were excluded for incomplete responses to the partner notification module. Of the remaining 1163 respondents, 701 (60.3%) identified as women, 467 (40.2%) identified as heterosexual, 956 (82.2%) had visited a health service in the last 12 months and 249 (21.4%) had an STI test in the last 6 months. The median age of the sample was 21.6 years (range 15.1–30.0) (Table 1). Two respondents were aged 30 years to account for birthdays occurring in the month of survey completion, as participants only provided month and year of birth.
| Demographic | Would you notify? | Would you want to be notified? | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | Univariate logistic regression | Yes | Univariate logistic regression | ||||||||||
| 95% CI | 95% CI | ||||||||||||
| n/N | % | n/N | % | OR | LL | UL | n/N | % | OR | LL | UL | ||
| Age group (years) | |||||||||||||
| 15–19 | 446/1163 | 38.35 | 410/446 | 91.93 | Ref | 437/446 | 97.98 | Ref | |||||
| 20–24 | 374/1163 | 32.16 | 336/374 | 89.84 | 0.78 | 0.48 | 1.25 | 365/374 | 97.59 | 0.84 | 0.33 | 2.13 | |
| 25–29 | 343/1163 | 29.49 | 310/343 | 90.38 | 0.82 | 0.50 | 1.35 | 340/343 | 99.13 | 2.33 | 0.63 | 8.69 | |
| Gender identity | |||||||||||||
| Man | 306/1163 | 26.31 | 278/306 | 90.85 | Ref | 300/306 | 98.04 | Ref | |||||
| Woman | 701/1163 | 60.28 | 635/701 | 90.58 | 0.97 | 0.61 | 1.54 | 687/701 | 98.00 | 0.98 | 0.37 | 2.58 | |
| OtherA | 156/1163 | 13.41 | 143/156 | 91.67 | 1.12 | 0.55 | 2.28 | 155/156 | 99.36 | EmptyB | |||
| Sexuality | |||||||||||||
| Heterosexual | 467/1163 | 40.15 | 418/467 | 89.51 | Ref | 456/467 | 97.64 | Ref | |||||
| Gay, homosexual or lesbian | 91/1163 | 7.82 | 85/91 | 93.41 | 1.66 | 0.69 | 4.00 | 88/91 | 96.70 | 0.71 | 0.19 | 2.59 | |
| Bisexual | 203/1163 | 17.45 | 190/203 | 93.60 | 1.71 | 0.91 | 3.23 | 202/203 | 99.51 | 4.87 | 0.62 | 38.0 | |
| OtherC | 402/1163 | 34.57 | 363/402 | 90.30 | 1.09 | 0.70 | 1.70 | 396/402 | 98.51 | 1.59 | 0.58 | 4.34 | |
| Visited a health service in the last 12 monthsD | |||||||||||||
| Yes | 956/1163 | 82.20 | 872/956 | 91.21 | Ref | 943/956 | 98.64 | Ref | |||||
| No | 201/1163 | 17.28 | 179/201 | 89.05 | 0.78 | 0.48 | 1.29 | 195/201 | 97.01 | 0.45 | 0.17 | 1.19 | |
| STI test in last 6 monthsD | |||||||||||||
| Yes | 249/1163 | 21.41 | 233/249 | 93.57 | Ref | 246/249 | 98.80 | Ref | |||||
| No | 911/1163 | 78.33 | 823/911 | 90.34 | 0.45 | 0.17 | 1.19 | 894/911 | 98.13 | 0.64 | 0.19 | 2.21 | |
| Total | 1163/1163 | 100 | 1056/1163 | 90.8 | 1142/1163 | 98.19 | |||||||
Preferences for notifying and being notified
Most (1056, 90.8%) respondents stated that they would notify a sexual partner if they had an STI and recommend their partners get tested, 10 (0.9%) stated they would not notify, and 79 (6.8%) stated it would depend on the situation. Most (1142, 98.2%) respondents also stated they would want to be notified by a sexual partner if their partner had an STI and 13 (1.1%) said they would not want to be notified or that it would depend on the situation. Univariate logistic regression showed no differences in the odds of wanting to notify or be notified by age, gender, sexuality or health seeking behaviours. Multivariate analysis was not undertaken due to univariate analysis confirming that there were no differences in the characteristics of people who would want to notify or be notified. Counts, proportions and logistic regression results are shown in Table 1.
Motivations for notifying and being notified
Participants who selected ‘Yes’, ‘No’ or ‘It depends’ when asked if they would notify or want to be notified were given the option to provide a free-text response as to why they chose that option. The number of responses for each question is provided in Table 2.
| Question and response | No. of free-text responses/no. of responses to question | |
|---|---|---|
| ‘If you had an STI, would you notify your current or past sexual partner/s that you have an STI and recommend they get tested?’ | ||
| Yes | 870/1056 | |
| No | 10/10 | |
| It depends | 55/79 | |
| Total | 935 | |
| ‘If you had sex with someone with an STI, would you want them to let you know they have an STI and that you should get tested?’ | ||
| Yes | ≥775/1142 | |
| No or It depends | ≤10/13 | |
| Total | 785 | |
Wanting to notify and be notified
For people who responded ‘Yes’ to Question 1 or 2 (Table 2), the most common reasons for wanting to notify was to protect and support their partners by reducing the impacts on their health and safety, including enabling them to seek medical advice. The most common motivations behind wanting to be notified by a partner consisted of valuing and wanting to look after their own health. People wanted to take action as quickly as they could by seeking medical advice, including testing and treatment, with significant awareness of the risk of complications if the STI was left untreated. This was followed by many who spoke about feeling a moral and ethical obligation to notify their partners and that notifying was the responsible thing to do. Of note, some spoke of the disrespect and betrayal they would feel if they were not notified. Another common motivation for both wanting to notify and be notified was seeking to reduce further transmission of the STI and protect others. The next most common reasons included a notion of treating others the way you want to be treated; notifying being a decent, respectful and courteous action; valuing and expecting honesty from a partner; and having the right to know about an issue that affects their health. Some viewed this as part of informed consent when agreeing to have sex with someone.
If someone has information that could help someone’s health, don’t they have a responsibility to share it? (20-year-old, other)
I don’t want someone to end up with PID [pelvic inflammatory disease] because I was too egocentric or embarrassed to tell them. (23-year-old, other)
Not wanting to notify
The predominant motivations for not wanting to notify a partner of an STI risk included feeling embarrassed, scared or uncomfortable; ill-feelings towards partners; a fear of getting into trouble; and a history of sexual assault.
I would be too embarrassed and scared to [notify]. (17-year-old, woman)
It depends
When asked if participants would notify or want to be notified, reasons for when this might depend largely centred around the type of relationship they had with their partner. This included whether participants were still in contact with their partner/s, if participants felt comfortable and safe contacting their partner/s, how well participants knew their partner/s, if they were on good terms, and whether participants could trust their partner/s with this kind of information. Other participants stated they might feel too embarrassed or awkward telling their partner/s or fear receiving a negative reaction, such as being stigmatised. Practical reasons included whether participants still had their partner/s contact information, the time elapsed since they had sex and whether it could be done anonymously.
Some I don’t have contact with, others I no longer trust with that information about me. (20-year-old, woman)
...I think it would depend on the person because there isn’t always a safe space to inform them of this. (21-year-old, woman)
Preferred notification methods
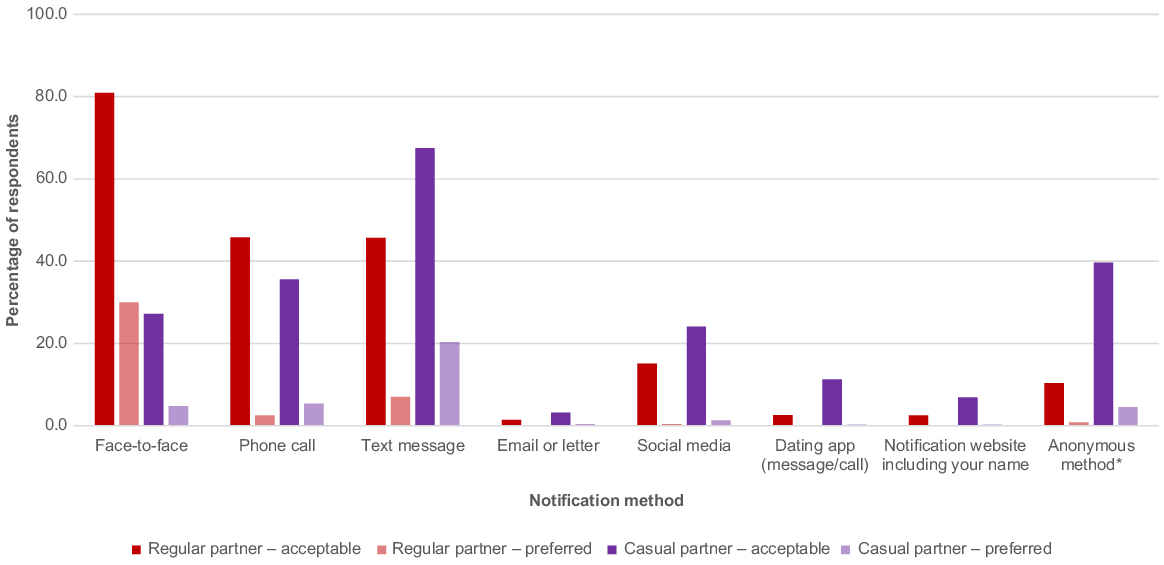
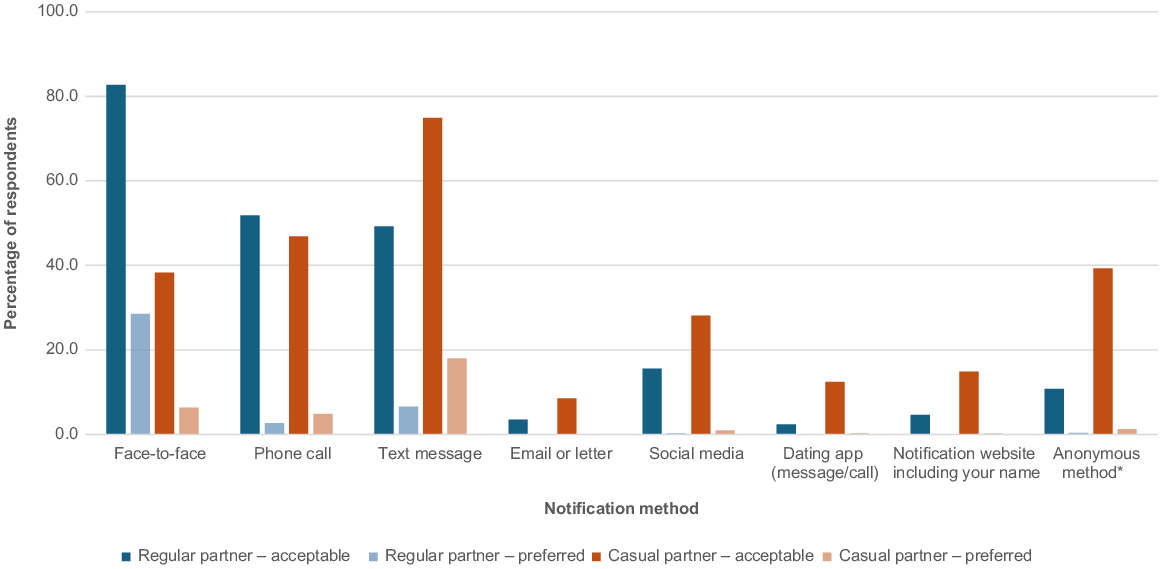
When hypothetically asked how they would prefer to notify a regular partner, 941 (80.9%) respondents chose face-to-face, 533 (45.8%) phone call, 531 (45.7%) text message and 176 (15.1%) social media. When notifying casual partners, 785 (67.5%) chose text message, 414 (35.6%) phone call, 361 (27.2%) face-to-face and 280 (24.1%) social media. When hypothetically asked how they would prefer to be notified by a regular partner, 962 (82.7%) chose face-to-face communication, 603 (51.8%) phone call, 573 (49.3%) text message and 181 (15.6%) social media. When being notified by a casual partner, 871 (74.9%) chose text message, 545 (46.9%) phone call, 445 (38.3%) face-to-face communication and 327 (28.1%) social media.
Almost one-third of participants chose only face-to-face communication with regular partners when notifying (349, 30.0%) and being notified (332, 28.5%). One-fifth of participants chose only text message for communicating with casual partners when notifying (236, 20.3%) and being notified (209, 18.0%) . Results for preferred methods to notify (Fig. 1) and be notified (Fig. 2) can be found below.
Percentage of respondents who chose at least each communication method (acceptable) and only each communication method (preferred) for notifying a regular and casual sexual partner that they are at risk of having an STI, N = 1163. *Anonymous methods include text or email via a notification website, through a friend or third person, with support from a health professional, or using an anonymous social media account or dating app.
Percentage of respondents who chose at least each communication method (acceptable) and only each communication method (preferred) for being notified by a regular and casual sexual partner that they are at risk of having an STI, N = 1163. *Anonymous methods include text or email via a notification website, through a friend or third person, with support from a health professional, or using an anonymous social media account or dating app.
Discussion
Our study found that, overwhelmingly, young people want to notify and be notified by sexual partners that they are at risk of having an STI, regardless of their age, gender and sexual identity. Young people want to notify and be notified by partners because they feel it is the responsible thing to do, to look after their own and their partner’s health and protect others by reducing transmission. Few stated that embarrassment and fear of repercussion may make them less likely to notify, and often a choice to notify would depend on the type of relationship shared. When notifying or being notified by a regular partner, face-to-face was the preferred method of communication, whereas for casual partners, respondents preferred to notify or be notified via text message. Around a quarter of respondents felt that notifying or being notified by a casual partner via social media was an acceptable method of communication, although few would like to use a dating app for notification. These relevant and practical findings can directly inform sexual health strategies designed to assist young people in undertaking what can be a daunting but crucial step in STI control.
Partner notification rates, in practice, are slightly lower than our findings of hypothetical intention to notify at around 74–92%,13–16 highlighting differences between intention and reality and the presence of known barriers discussed below. Our results also show that notification intention is influenced by relationship type, as has been found in previous studies.17 The reasons for wanting to notify and be notified by sexual partners of an STI risk are consistent across the literature. These reasons include wanting to reduce transmission, care for their partner and feeling that it was the right thing to do, along with barriers, including fear of embarrassment, social stigma, retaliation or loss of relationship.5,9,16–18 Previous studies looking at notification methods also showed face-to-face and phone call were preferred options.9,16,19 Our findings show an increase in text message favourability compared to that found by Hopkins et al.19, likely reflecting the increased use of smartphone technology.20 Few studies have looked at the use of social media. Contesse et al. found that men who have sex with men were generally comfortable with use of geo-spatial networking apps for HIV and STI partner notification, either by partner services staff using a health department profile or by a hypothetical built-in anonymous messaging system.21 Similar to Tomnay et al.22, we found that young people preferred to use anonymous communication methods for notifying and being notified by casual partners compared to regular partners, which may reflect the ways in which they met their casual partners, such as online and through dating apps.
There are several strategies that can be used to support young people’s engagement in partner notification. In their recent recommendations to improve digital partner notification, Kocur et al. highlight that interventions need to empower and support the index patient, be convenient and integrate with other systems, and normalise partner notification as a social responsibility and an act of caring.5 Some strategies likely to assist young Australians with partner notification uptake include providing resources (such as a comparison table or interactive decision tool) that help the index patient choose their preferred method of notification, including tailoring by different partner types,23 pre-recorded demonstrations and adaptable scripts for face-to-face or telephone notification, example text message templates (such as that provided on the Management of Chlamydia Cases in Australia24 and Better To Know25 websites) and providing STI information and local testing options.5 Partner notification messaging should also reinforce positive aspects, such as collective responsibility, including looking after one’s own and their partner’s health, which were key motivators found in our study. Such resources could be made available on general practice, state-based public health unit, state and federal government, and sexual health organisation websites (including in different languages). Workforce training and resources that can be implemented into existing workflows to support clinicians in discussing and undertaking partner notification can also strengthen the crucial role that primary care providers play in STI control. Supporting the uptake of patient-initiated partner notification is particularly pertinent, as the work of GPs and health department contact tracers continues to be resource limited, particularly for common STIs such as chlamydia and gonorrhoea.
This study has several strengths. First, recruitment was conducted online via social media, a platform in which young people are highly engaged. Second, a large sample size was used and with a composition that reflected the general Victorian population, not just people diagnosed with an STI. Third, the inclusion of free-text responses added richness and complexity to the quantitative findings.
Study limitations include the use of convenience sampling during recruitment that may have led to possible selection bias.
Those who completed the survey are likely to have been more engaged in their health, which is reflected by more than 80% of our sample having visited a health service in the last 12 months. This may lead to an overrepresentation of people who may be more likely to notify their partners. Additionally, the use of hypothetical scenarios was chosen to maximise the number of responses but may have led to a disparity between intended and actual partner notification actions. For example, some participants might have intended to notify in the survey, when in reality they might not. Though not included in this survey, the type of STI may also influence notification intentions, as different STIs carry differing levels of stigma, transmission risk and management pathways. Finally, as the survey was only advertised in Victoria and recruited more women and other gender groups than the average Australian population, the sample may not be representative of all young people in Australia.
STIs are continuing to rise, particularly among young people, and emerging threats, such as antimicrobial resistance and novel diseases (e.g. Mpox), present new challenges to STI control. Empowering young people to engage in partner notification by providing tailored and practically relevant partner notification resources can help to reduce transmission and reproductive complications associated with STIs, benefiting not only the individual and their partner but also the wider community.
Data availability
The datasets generated and analysed during this study are not publicly available due to participant privacy and confidentiality but are available from the corresponding author on reasonable request, pending approval from the Alfred Health Research Ethics Committee.
Conflicts of interest
ML and JC are Associate Editors of Sexual Health. To mitigate this potential conflict of interest they had no editor-level access to this manuscript during peer review. MH receives funding from Gilead Science and Abbvie for investigator-initiated research unrelated to this area of work. All other authors declare no conflicts of interest.
Declaration of funding
The research received no specific project funding. SM is supported by a Burnet Institute PhD scholarship, JH and MH by a National Health and Medical Research Council (NHMRC) Investigator Grant (GNT2025960 and GNT1194322, respectively) and ML by a NHMRC Career Development Fellowship.
Acknowledgements
The authors thank all the young Victorians who participated in the survey. We gratefully acknowledge the support that Burnet Institute receives from the Victorian Operational Infrastructure Support Program.
References
2 The Lancet Child Adolescent Health. Youth STIs: an epidemic fuelled by shame. Lancet Child Adolesc Health 2022; 6(6): 353.
| Crossref | Google Scholar |
3 Ferreira A, Young T, Mathews C, Zunza M, Low N. Strategies for partner notification for sexually transmitted infections, including HIV. Cochrane Database Syst Rev 2013; 2013(10): CD002843.
| Crossref | Google Scholar |
4 Australasian Society for HIV Viral Hepatitis and Sexual Health Medicine (ASHM). How far back to trace; 2022. Available at https://contacttracing.ashm.org.au/how-far-back-to-trace/ [updated September 2022]
5 Kocur W, McLeod J, Bloch SCM, MacDonald JJ, Woodward C, McInnes-Dean A, et al. Improving digital partner notification for sexually transmitted infections and HIV through a systematic review and application of the Behaviour Change Wheel approach. Sex Health 2024; 21: SH23168.
| Crossref | Google Scholar |
6 Melbourne Sexual Health Centre. Let them know; 2024. Available at https://letthemknow.org.au [cited 11 September 2024]
7 Australasian Society for HIV Viral Hepatitis and Sexual Health Medicine (ASHM). Ways of notifying contacts; 2024. Available at https://contacttracing.ashm.org.au/ways-of-notifying-contacts/ [cited 11 September 2024]
8 Healthdirect Australia. Sexually transmitted infections (STI); 2024. Available at https://www.healthdirect.gov.au/sexually-transmitted-infections-sti [cited 11 September 2024]
9 Reed JL, Huppert JS, Gillespie GL, Taylor RG, Holland CK, Alessandrini EA, et al. Adolescent patient preferences surrounding partner notification and treatment for sexually transmitted infections. Acad Emerg Med 2015; 22(1): 61-6.
| Crossref | Google Scholar |
10 Eddy S, Douglass C, Raggatt M, Thomas A, Lim M. Trends in testing of sexually transmissible infections (STIs), sexual health knowledge and behaviours, and pornography use in cross-sectional samples of young people in Victoria, Australia, 2015-21. Sex Health 2023; 20(2): 164-72.
| Crossref | Google Scholar |
11 Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform 2019; 95: 103208.
| Crossref | Google Scholar |
12 Vears DF, Gillam L. Inductive content analysis: a guide for beginning qualitative researchers. FoHPE 2022; 23(1): 111-27.
| Crossref | Google Scholar |
13 van Aar F, van Weert Y, Spijker R, Gotz H, Op de Coul E, for the Partner Notification Group. Partner notification among men who have sex with men and heterosexuals with STI/HIV: different outcomes and challenges. Int J STD AIDS 2015; 26(8): 565-73.
| Crossref | Google Scholar |
14 Chitneni P, Beksinska M, Dietrich JJ, Jaggernath M, Closson K, Smith P, et al. Partner notification and treatment outcomes among South African adolescents and young adults diagnosed with a sexually transmitted infection via laboratory-based screening. Int J STD AIDS 2020; 31(7): 627-36.
| Crossref | Google Scholar |
15 Gursahaney PR, Jeong K, Dixon BW, Wiesenfeld HC. Partner notification of sexually transmitted diseases: practices and preferences. Sex Transm Dis 2011; 38(9): 821-7.
| Crossref | Google Scholar |
16 Bilardi JE, Fairley CK, Hopkins CA, Hocking JS, Temple-Smith MJ, Bowden FJ, et al. Experiences and outcomes of partner notification among men and women recently diagnosed with Chlamydia and their views on innovative resources aimed at improving notification rates. Sex Transm Dis 2010; 37(4): 253-8.
| Crossref | Google Scholar |
17 McMahan KD, Olmstead SB. Disclosure of sexually transmitted infections to sexual partners: a systematic critical literature review. J Sex Res 2024; 1-15.
| Crossref | Google Scholar |
18 Cavalcante EGF, Miranda MCC, Carvalho AZFHTd, Lima ICVd, Galvão MTG. Partner notification for sexually transmitted infections and perception of notified partners. Rev Esc Enferm USP 2016; 50(3): 450-7.
| Crossref | Google Scholar |
19 Hopkins CA, Temple-Smith MJ, Fairley CK, Pavlin NL, Tomnay JE, Parker RM, et al. Telling partners about chlamydia: how acceptable are the new technologies? BMC Infect Dis 2010; 10: 58.
| Crossref | Google Scholar |
20 Olson JA, Sandra DA, Colucci ES, Al Bikaii A, Chmoulevitch D, Nahas J, et al. Smartphone addiction is increasing across the world: a meta-analysis of 24 countries. Comput Hum Behav 2022; 129: 107138.
| Crossref | Google Scholar |
21 Contesse MG, Fredericksen RJ, Wohlfeiler D, Hecht J, Kachur R, Strona FV, et al. Attitudes about the use of geosocial networking applications for HIV/STD partner notification: a qualitative study. AIDS Educ Prev 2019; 31(3): 273-85.
| Crossref | Google Scholar |
22 Tomnay JE, Hulme-Chambers A, Bilardi J, Fairley CK, Huffam S, Chen MY. A qualitative study of means to improve partner notification after an HIV diagnosis among men who have sex with men in Australia. AIDS Patient Care STDS 2017; 31(6): 269-74.
| Crossref | Google Scholar |
23 Estcourt CS, Flowers P, Cassell JA, Pothoulaki M, Vojt G, Mapp F, et al. Going beyond ‘regular and casual’: development of a classification of sexual partner types to enhance partner notification for STIs. Sex Transm Infect 2022; 98(2): 108-14.
| Crossref | Google Scholar |
24 The University of Melbourne. Discuss partner management; 2024. Available at https://www.mocca.org.au/home/support-partner-management [cited 11 September 2024]
25 Australian Federation of AIDS Organisations, Anwernekenhe National HIV Alliance. Notify via SMS; 2024. Available at https://www.bettertoknow.org.au/notify-a-partner/notify-via-sms/ [cited 11 September 2024]


