Outreach nurses critical for delivery of HIV care to women in western Victoria
Andrew P. Gador-Whyte A , Christine Roder B C , Rochelle Hamilton B D , Helen Fay B , Emily Huning E , Emma Nicholson B F , Kathryn Mackie G H , Eugene Athan B C and Amanda J. Wade
A , Christine Roder B C , Rochelle Hamilton B D , Helen Fay B , Emily Huning E , Emma Nicholson B F , Kathryn Mackie G H , Eugene Athan B C and Amanda J. Wade  B I *
B I *
A
B
C
D
E
F
G
H
I
Sexual Health - https://doi.org/10.1071/SH23153
Submitted: 11 August 2023 Accepted: 24 October 2023 Published online: 9 November 2023
Abstract
Women living with HIV in regional Victoria face barriers accessing care. We evaluated the care cascade and outreach nurse support required for women attending our service between 2005 and 2020. A total of 33 women attended; 97% (32/33) were on antiretroviral therapy; 67% (22/33) retained in care, 27% (9/33) transferred and 6% (2/33) lost to follow up. Of women retained in care, 95% (21/22) were on antiretroviral therapy and 91% (20/22) had virological suppression. A total of 91% (30/33) required outreach nurse care (median care episodes 100/woman; IQR 44–179) – most frequently (87%; 26/30) liaising with pharmacies and prescribers. Outreach nurses are critical in achieving UNAIDS targets for women in western Victoria.
Keywords: capacity building, case management, healthcare disparities, health services, living with HIV, pregnancy, rural health, women.
Women living with HIV in Victoria represent a diverse group – tailored services are required to overcome barriers to care.1,2 Almost two-thirds of people living with HIV in rural and regional Australia travel more than 50 km to seek HIV care.3 Women often have caring responsibilities to negotiate.4 We evaluated the care cascade and the outreach nurse support required for women attending our HIV service.
The Barwon Health HIV Service provides interdisciplinary care, including antiretroviral therapy (ART), psychiatric and pharmacy support, throughout western Victoria. The outreach nurses meet patients at their homes, community services, primary care services or hospital clinics. Cisgender women living with HIV attending between January 2005 and December 2020 were included. Care episodes were defined as the Department of Health’s Victorian Integrated Non-Admitted Health contacts. Study outcomes were: patient engagement status – retained in care (attended clinic within the past year), transferred or lost to follow up (LTFU); commencement of ART (defined as a script being written); virological suppression (defined as <50 copies/mL at last review if retained in care); viral load (VL) at 36 weeks’ gestation; mother-to-child transmission; proportion referred to the outreach nurse; types of care required; and care episodes per woman. Ethics approval was obtained.
Twenty percent (33/168) of people attending were women. Median age at referral was 29 years (IQR 21–40). Fifty-five percent (18/33) were Australian born; 11% (3/28) lived in insecure housing. A total of 70% (23/33) lived in a major city (Geelong (22); Melbourne (1)), 21% (7/33) in an inner regional area and 9% (3/33) in an outer regional area (by Australian Statistical Geography Standard Remoteness Structure coding; https://www.abs.gov.au/statistics/standards/australian-statistical-geography-standard-asgs-edition-3/jul2021-jun2026/remoteness-structure/remoteness-areas). Sixty-one percent (17/28) were working or studying, 25% (7/28) were unemployed and 14% (4/28) received the Disability Support Pension.
Twenty-two of 33 (67%) women were retained in care, nine (27%) transferred and two (6%) LTFU. Women attended for a median of 31 months (IQR 8–53). Of the women retained in care, 21/22 (95%) were on ART, and one was an elite controller. Twenty of 22 (91%) women had virological suppression, one woman had 81 copies/mL and one another woman had 181 copies/mL. Twenty-one women (64%) had mental health diagnoses, the most common being anxiety disorders (17; 52%) and major depression (13; 39%). Three (9%) had attempted suicide. Nineteen pregnancies in nine women resulted in 14 live births – nine deliveries at our hospital and five elsewhere. The VL at 36 weeks was: undetectable (9), 81 copies/mL (1), 57 copies/mL (1), 46 copies/mL (1), and unknown at another service (2). A total of 86% (12/14) infants screened HIV-negative – two infants had not completed the testing schedule and were linked back into care.
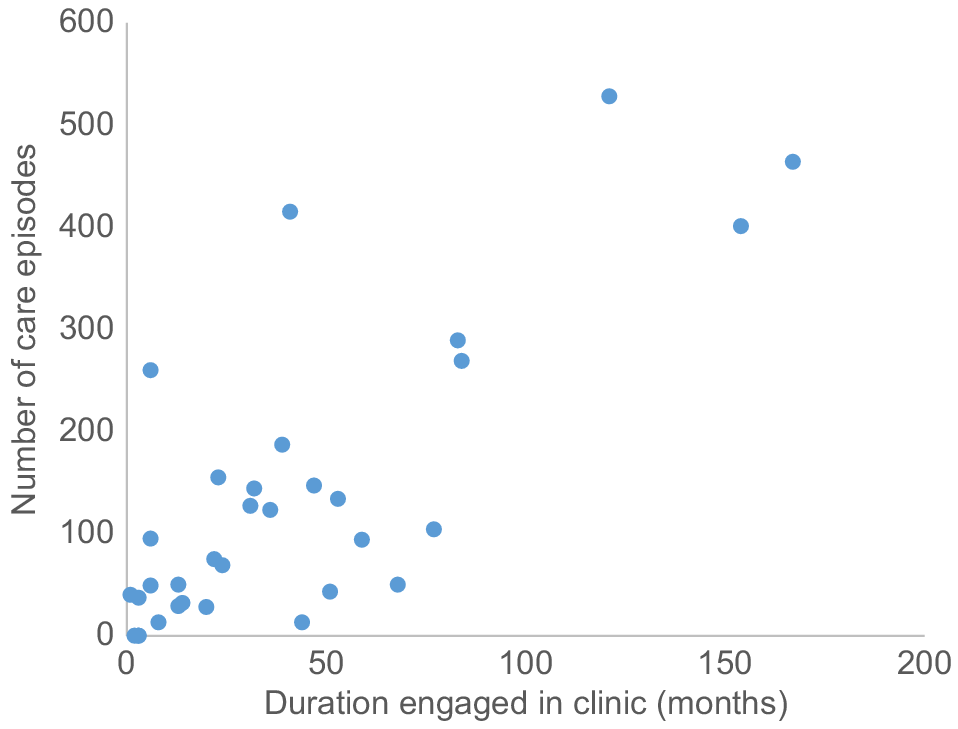
Ninety-one percent of women (30/33) were referred to the outreach nurse (median care episodes 100/woman; IQR 44–179) (Fig. 1). Types of outreach nursing care required included: liaising with pharmacies and ART prescribers 26/30 (87%), linkage to a GP 24/30 (80%), education 20/30 (67%), supporting pathology collection 16/30 (53%), vaccination scheduling 16/30 (53%), linkage to HIV community group 13/30 (43%) and assistance with housing 12/30 (40%). The median number of types of outreach care provided per woman was eight (IQR 5–10).
Number of care episodes provided by the outreach nurse and duration of engagement with the service (months), by woman living with HIV.
This cohort of women living with HIV required outreach nurse support to realise the benefits of ART. The range of care, frequency and continuity of outreach nurse support was key to high retention in care and rates of ART commencement, virological suppression and prevention of mother-to-child transmission. This study highlights the potential of outreach nurses in the HIV elimination response in low prevalence areas including regional Australia.
Data availability
The data that support this study cannot be publicly shared due to ethical or privacy reasons and may be shared upon reasonable request to the corresponding author if appropriate.
References
1 Moreira C, Boughey A, Ryan KE, Higgins N, Rotty J, West M, et al. Two decades of surveillance data show late presentation among a diverse group of women diagnosed with HIV in Victoria, Australia. Aust N Z J Public Health 2019; 43(5): 413-418.
| Crossref | Google Scholar | PubMed |
2 Giles M, MacPhail A, Bell C, Bradshaw S, Furner V, Gunathilake M, et al. The barriers to linkage and retention in care for women living with HIV in an high income setting where they comprise a minority group. AIDS Care 2019; 31(6): 730-736.
| Crossref | Google Scholar | PubMed |
3 Norman T, Power J, Rule J, Chen J, Bourne A. HIV futures 10: quality of life among people living with HIV in Australia (monograph series number 134). Melbourne: Australian Research Centre in Sex, Health and Society, La Trobe University; 2022. doi:10.26181/21397641


