Engaging older Australians in sexual health research: SHAPE2 survey recruitment and sample
Louise Bourchier A * , Meredith Temple-Smith
A * , Meredith Temple-Smith  B , Jane Hocking
B , Jane Hocking  A , Helen Bittleston
A , Helen Bittleston  A and Sue Malta
A and Sue Malta  A
A
A
B
Abstract
Sexual health research rarely includes older age groups and the sexual health needs of older Australians are not well understood. Older adults are online in increasing numbers; however, internet surveys involving samples of older adults and sensitive topics remain uncommon. In 2021, we developed an online survey to explore the sexual health needs of Australians aged 60+ years. We describe here survey recruitment and sample obtained, comparing it with national population data (Australian Bureau of Statistics) and the sample of the similar ‘Sex, Age and Me’ study from 2015.
We recruited 1470 people with a staggered three-phase strategy: (1) emails to organisations and community groups; (2) paid Facebook advertising; and (3) passive recruitment. Half (50.6%) found out about the study via an organisation or group and just over a third (35.7%) from Facebook.
The sample was equally balanced between men (49.9%) and women (49.7%) (0.4% other gender identities). Participants were aged 60–92 years (median 69 years) with all Australian States/Territories represented. Facebook recruits were younger, more likely to be working rather than retired, and more likely to live outside a major city, than those recruited by other means.
Using the recruitment methods described, we successfully obtained a diverse and fairly representative sample of older Australians within the constraints of a convenience sample and on a modest budget. This research sheds light on ways to engage an under-served demographic in sexual health research. Our experience shows that many older adults are amenable to recruitment for online sexual health surveys using the approaches outlined.
Keywords: ageing, health promotion, internet survey, older adults, public health, recruitment, sexual health, survey methods.
Introduction
Older adults’ sexual health and sexual behaviour has gathered more research attention in recent years, reflecting the emerging needs of ageing populations globally. It is well established that many older adults continue to be interested in sex, to engage in both partnered and solo sexual activity, and are able to articulate their changing sexual health needs.1–6 To address the evolving sexual health needs of older adults, quality research using appropriate study designs and recruitment methods is necessary. While the definition of ‘older adult’ varies between studies, typically ranging in age from between 50 years to 65 years onwards;1,7–11 for the purposes of the present study we defined ‘older adults’ as those aged 60 years and over following the rationale of Malta.12
Sexually transmissible infections (STIs) are rising among older age groups in Australia13,14 as they are in other countries,15–17 and condom use is lower among older Australians than among younger people.18–21 These factors, alongside the fact that older adults’ sexual health is not regularly addressed in the Australian primary care setting,22–24 indicate the need for more attention on older adults’ sexual health. In light of this, researchers have advocated for better access to relevant sexual health promotion materials and sexual healthcare for older Australians.17,25–28 Best practice in sexual health promotion and sexual health service provision has been explored for younger demographics but may look different from that needed for older people where more research is needed to ensure they are fit for purpose.
In recent years, several studies have sought to improve our understanding of the sexual health of older Australians and to explore how their needs could be better met.24,29,30 Two were large sexual health surveys: (1) the ‘Second Australian Study of Health and Relationships’ (ASHR2), which included older adults within a larger sample; and (2) ‘Sex, Age and Me’ (SA&M), which recruited only older adults. Each used a different recruitment strategy to access participants, which may have had an impact on study findings.
ASHR2 (2012–2013) collected data via a computer-assisted telephone survey and used population-based sampling to recruit approximately 20 000 people aged 16–69 years, of whom older adults aged 60–69 years were recruited proportionately to their percentage in the population.29 Survey results found lower rates of condom use among older men than among younger men, that STI knowledge was also poorer among older participants compared to younger participants,21,31 and that older Australians used dating apps and online dating, albeit at lower rates than younger age groups.32 Older participants were more likely to complete the survey via a landline telephone than younger people who were more likely to use a mobile phone, and older women were more likely to rely on a landline than were older men.33 These findings suggest that older adults’ participation was influenced by recruitment methods and that engagement with technology may vary by gender.
SA&M (2015) recruited older adults aged 60 years and over. It comprised a survey (n = 2137), plus qualitative interviews with a sub-set of survey participants (n = 53).30 The survey found low rates of STI testing despite high STI knowledge overall,25,27 and interview participants highlighted the importance of age-inclusive services and sexual health promotion relevant to older adults.28 The study used a multi-pronged approach to recruitment, which included advertising via radio, TV, social media, paper flyers, in-person events, and promotion through relevant organisations. Participants were able to complete the survey either online or on paper and the vast majority (98.3%, n = 2101) undertook the survey online.30 When asked how they found out about the study, 54% indicated that they had seen it on Facebook, and 13% said they had seen it on another website,30 demonstrating that online recruitment strategies can be effective for recruiting older Australians for sexual health research.
Another study, the qualitative ‘Sexual Health, Ageing, Perspectives and Education’ (SHAPE) Project was conducted in 2016–2017. This research explored the barriers to sexual health discussions between health care providers and older patients23,24 and concluded that a digital checklist tool could help facilitate these conversations in primary care.34 The older adults in the SHAPE project were aged 60 years and over and participated in interviews and focus groups (n = 21). They were recruited via promotional materials sent to relevant organisations, through the project website, researcher networks, and snowballing.24 Findings showed that these older adults had many sexual health education needs, but felt unable to bring up the topic in consultations or that their concerns were dismissed, with some reporting ageist attitudes by their health care professionals.23,24
To explore whether these findings from SHAPE were typical of today’s older Australians, we launched ‘SHAPE2’, an online survey to explore the sexual health information-seeking behaviours of people aged 60 years and over in Australia in 2021. Given the sensitive nature of this research and the different recruitment approaches used in previous studies, we report here the study methodology for SHAPE2 including study design, eligibility and recruitment methods. We compare the socio-demographic and behavioural profile of our participants with national population data and with the sample of the SA&M study conducted 6 years earlier. We used a staggered three-phase approach to recruit participants and were cognisant of the need to investigate how effective this was at achieving a diverse representation of people aged 60 years and over. This paper reflects on the experiences, strengths and limitations of our recruitment strategies, to assist others who may be considering recruiting older research participants for sexual health research.
Materials and methods
SHAPE2 study design
The SHAPE2 online survey employed a cross-sectional design, which is reported here guided by the CHERRIES checklist criteria for internet survey reporting.35 The survey was designed using Qualtrics software and included 63 questions, each on an individual screen, organised into nine blocks (see Supplementary material, Appendix A for survey questions). We used adaptive questioning, whereby some questions were displayed conditionally depending on previous responses, ensuring all survey items displayed to participants were relevant. The survey was tested for usability and technical functionality by colleagues of the researchers and was then pilot tested with approximately 10 older adults, before final refinements. We initially designed this study as an online survey because of logistical difficulties with administering hard copy surveys during the coronavirus disease 2019 (COVID-19) pandemic and due to budget constraints, however, later in the data collection process a small number of paper surveys were posted out to those who contacted the researchers requesting hard copies. The online survey took participants a median of 17 min to complete.
The survey included questions on sexual health information-seeking as well as on demographics, relationships, identity, and behaviours. The questions on sexual health information-seeking included whether participants had sought sexual health information since turning 60 years old, what sources they had accessed, what sexual health topics they had inquired about, whether they had found answers to their questions, where they would look for sexual health information in future, what topics they would like to know more about and what makes sexual health resources trustworthy and appealing (Supplementary material, Appendix A).
Population and sampling
Like both SA&M and the original SHAPE Project, an age of 60 years or over and Australian residency were the only inclusion criteria, thus allowing for greater comparison with these earlier studies. Our aim was to recruit a sample size of 500 participants over 2 months to obtain confidence intervals of approximately ±4% around a proportion of 50%. However, we adjusted our target upwards and extended our recruitment timeline after strong initial response numbers.
We sought to recruit a sample as representative of older Australians as possible within the limitations of a convenience sample. We monitored basic demographic characteristics of participants as survey responses were submitted (age, location, gender, sexual orientation) and adjusted our recruitment strategy where necessary to recruit as diverse and representative a sample as was feasible. This study was undertaken on a modest budget of AUD400, which was used for paid Facebook advertising.
Study ethics
Ethical approval was granted by the University of Melbourne Human Research Ethics Committee (HREC ID 2057393). Prior to survey commencement, prospective participants were provided with a plain language statement, which included information about the study, expected time commitment, contact details for the researchers, information about data storage and security, and support services in case the survey brought up anything troubling for them. Before commencing, participants provided consent and proceeded to the survey questions; those that declined were exited from the survey. The survey was anonymous, and participants were not asked any identifying information.
Respondents could review and change previous responses using a ‘back’ button, skip questions they preferred not to answer and could exit the survey at any time. As the survey was anonymous; however, responses that were already entered could not be withdrawn. During data collection we checked responses to free-text questions periodically to identify any potential signs of distress (e.g. reference to past sexual assault). A small number of comments were identified as potentially indicating distress and were brought to the attention of the ethics committee. However, follow up with these respondents was not possible due to the survey’s anonymous design.
Recruitment
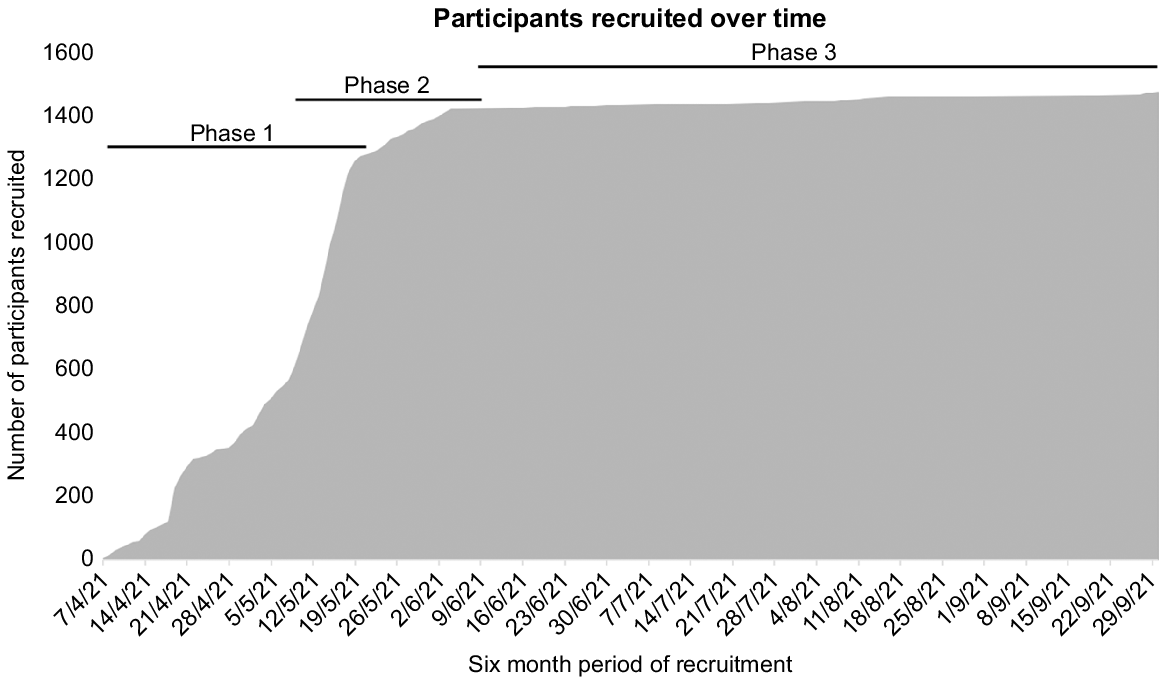
The survey opened on the 31 March 2021 with an initial soft release where it was promoted within researchers’ networks and on Twitter. Recruitment began in earnest on 7 April 2021 and was conducted in three staggered phases. Phase 1 (7 April–20 May 2021) involved emailing organisations that serve or attract older adults; Phase 2 (8 May–7 June 2021) used paid Facebook advertising targeting the population of interest; and Phase 3 (8 June–31 September) was the passive recruitment phase where the survey remained open, but active recruitment ceased. No incentives were given for participation.
During Phase 1, emails were sent in batches to approximately 2500 organisations, community groups (e.g. Council on the Ageing (COTA) Victoria, Probus, University of the Third Age, Men’s Sheds) and social groups via government councils. These contacts were found via internet searches. The email explained the study and the recruitment flyer was attached (Fig. 1). Recipients were encouraged to share the link and flyer with their members or communities as they saw fit (e.g. via newsletters, social media, or noticeboards). While we contacted online dating sites in Phase 1, none of them promoted the SHAPE2 survey.
For Phase 2, we launched a paid Facebook advertisement that was displayed only to older adults within Australia. After a week, we added a second advertisement to be displayed only to older women in Australia in an effort to recruit more women. We ran both advertisements concurrently for 2 weeks. For the final week, we stopped the second advertisement and continued only with the general advertisement, for which we changed the geographical settings so it was shown only in three States/Territories where we sought to increase participation. After 4 weeks, Facebook advertising ended as our AUD400 budget was reached.
After active recruitment ceased, we continued to record a small number of survey responses every few days and prospective participants continued to make contact by email and phone. Because of this, we left the survey open and allowed responses to trickled in, forming Phase 3 of recruitment. After 3 months of this passive recruitment, the survey was closed on 30 September 2021 after it had been open for a total of 6 months. This is the same timeframe for data collection as SA&M, providing opportunity for comparison.
Results
A total of 1470 participants were recruited. During the first part of Phase 1, we recruited 543 participants (31 days). While Phase 1 and 2 were running concurrently, we recruited a further 725 participants (13 days), 149 more people were recruited during the later part of Phase 2 (18 days), and Phase 3 yielded only a further 53 participants (115 days) (Fig. 2).
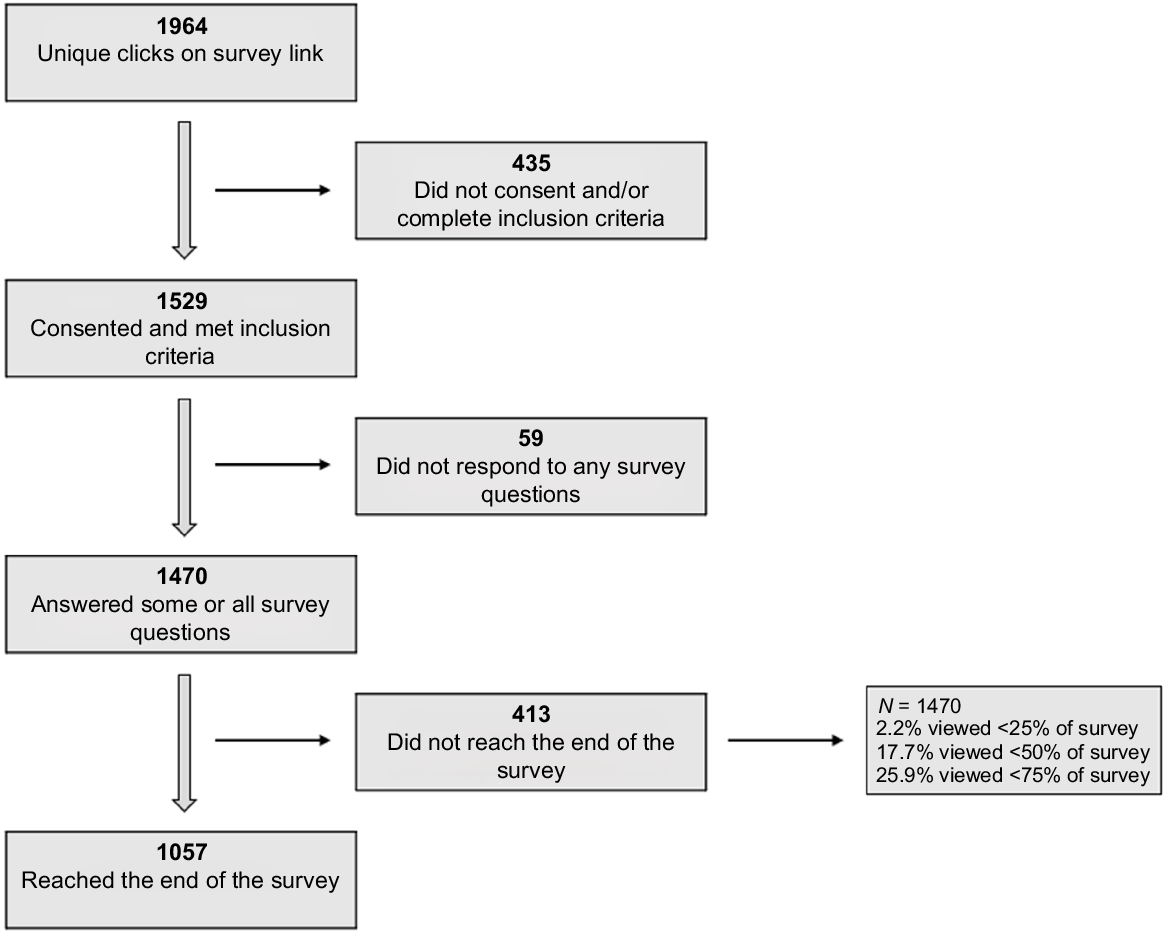
It is not possible to know how many people viewed the advertisement for the study, and we cannot calculate the response rate. However, of the 1964 individuals who clicked on the survey link, 1529 (77.9%) consented and met inclusion criteria, 1470 (74.8%) provided responses that could be used in the analysis, having answered some or all survey questions and 1057 (53.9%) reached the end of the survey. A breakdown of response numbers is in Fig. 3.
Respondents were not prevented from attempting the survey more than once; instead, multiple entries were identified and removed during data cleaning. This was performed by identifying duplicate IP addresses and checking key demographics (age, gender, postcode) to identify attempts from the same individual. Where duplicates were identified the most complete response was retained and where multiple entries were complete, the most recent was retained. Sixty three entries were deleted, the majority of which had not progressed beyond the inclusion criteria screens, suggesting these people opened the survey before coming back later to complete it. Interestingly, there were 21 IP addresses with more than one response recorded where the key demographics were distinct, suggesting partners or friends using the same device to respond to the survey, including an instance where four people used the same device. Where the IP address was the same, but key demographics distinct, responses were retained on the basis of these being different respondents.
We asked participants where they had heard about the survey. A total 29.7% did not complete this question (2.5% declined to answer and 27.2% did not reach the question which was near the end of the survey). However, of the 1070 people who responded, half (50.6%) found out through a newsletter/organisation or club and just over a third (35.7%) found out through Facebook (Table 1).
| Source of recruitment | SHAPE2A | Sex, Age and MeB | |||
|---|---|---|---|---|---|
| N = 1070C | N = 2137 | ||||
| n | % | n | % | ||
| Newsletter/from an organisation or club of which I am a member | 541 | 50.6 | 158 | 7.4 | |
| 382 | 35.7 | 1136 | 53.2 | ||
| From a friend or family member | 55 | 5.1 | 65 | 3.1 | |
| Other social media (e.g. Twitter, Instagram) | 9 | 0.8 | 11 | 0.5 | |
| From a GP or other health professional | 3 | 0.3 | 12 | 0.6 | |
| Other online source (website, blog, forum, dating service) | 1 | <0.1 | 441 | 20.7 | |
| Media (newspaper, magazine, radio, television) | 1 | <0.1 | 272 | 12.7 | |
| Other | 42 | 3.9 | 127 | 5.9 | |
| Not reported | 36 | 3.4 | 24 | 1.1 | |
Sample recruited
We successfully recruited a sample with approximately equal numbers of male and female participants, that included ages 60–92 years (median age 69 years), and with respondents from throughout Australia. Participant characteristics are in Table 2 and comparisons made with Australian Bureau of Statistics (ABS) population data, and the SA&M sample from 2015. SHAPE2 participants are further broken down by whether they were recruited via Facebook or by other means.
| SHAPE2 | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Total sample | Participants recruited via Facebook | Participants recruited via other means | ABS population data for ages 60+ A | Sex, Age and Me sample 30 | |||||
| N = 1470 | N = 382 B | N = 652 B | N = 5 788 780 | N = 2137 | |||||
| n | % | n | % | n | % | % | % | ||
| Gender | |||||||||
| Male | 734 | 49.9 | 167 | 43.7 | 366 | 56.1 | 47.3 | 67.7 | |
| Female | 730 | 49.7 | 214 | 56.0 | 282 | 43.3 | 52.7 | 32.0 | |
| Other gender identities | 6 | 0.4 | 1 | 0.3 | 4 | 0.6 | Not collected | 0.4 | |
| Age (years) | |||||||||
| 60–64 | 455 | 31.0 | 161 | 42.2 | 143 | 21.9 | 25.2 | 40.7 | |
| 65–69 | 387 | 26.3 | 120 | 31.4 | 156 | 23.9 | 22.1 | 34.3 | |
| 70–74 | 321 | 21.8 | 70 | 18.3 | 169 | 25.9 | 19.7 | 15.6 | |
| 75–79 | 187 | 12.7 | 20 | 5.2 | 115 | 17.7 | 14.1 | 5.8 | |
| 80–84 | 93 | 6.3 | 10 | 2.6 | 53 | 8.1 | 9.5 | 2.6 | |
| 85+ | 27 | 1.8 | 1 | 0.3 | 16 | 2.5 | 9.5 | 1.0 | |
| State/Territory | |||||||||
| New South Wales | 393 | 26.7 | 73 | 19.1 | 187 | 28.7 | 32.4 | 31.1 | |
| Victoria | 372 | 25.3 | 131 | 34.3 | 143 | 21.9 | 25.1 | 24.4 | |
| Queensland | 197 | 13.4 | 71 | 18.6 | 60 | 9.2 | 20.1 | 19.1 | |
| Western Australia | 174 | 11.8 | 31 | 8.1 | 94 | 14.4 | 9.9 | 9.3 | |
| Australian Capital Territory | 154 | 10.5 | 10 | 2.7 | 113 | 17.3 | 1.4 | 3.4 | |
| South Australia | 110 | 7.5 | 45 | 11.8 | 25 | 3.8 | 7.9 | 9.1 | |
| Tasmania | 58 | 4.0 | 13 | 3.4 | 28 | 4.3 | 2.6 | 3.0 | |
| Northern Territory | 12 | 0.8 | 8 | 2.1 | 2 | 0.3 | 0.6 | 0.7 | |
Postcodes were compared to ABS data to determine remoteness36 and socio-economic deciles.37 Close to two thirds of survey participants were located in major cities (63.8%), approximately a third in regional locations (35.0%), and a small number in remote locations (1.2%) (Table 3). Postcodes from all socio-economic deciles were represented in the sample but skewed towards more advantaged geographical areas (Table 3).
| SHAPE2 | ||||
|---|---|---|---|---|
| Total sample (N = 1470) | Participants recruited via Facebook (N = 382) | Participants recruited via other means (N = 652) | ||
| Location | N = 1456 | N = 376 | N = 650 | |
| Major cities | 929 (63.8%) | 209 (55.6%) | 451 (69.4%) | |
| Regional | 510 (35.0%) | 162 (43.1%) | 195 (30.0%) | |
| Remote | 17 (1.2%) | 5 (1.3%) | 4 (0.6%) | |
| Socio-economic status of postcode (decile) A | N = 1456 | N = 376 | N = 650 | |
| 1–2 | 188 (12.9%) | 61 (16.2%) | 58 (8.9%) | |
| 3–4 | 244 (16.8%) | 73 (19.4%) | 104 (16.0%) | |
| 5–6 | 251 (17.2%) | 80 (21.3%) | 88 (13.5%) | |
| 7–8 | 293 (20.1%) | 82 (21.8%) | 114 (17.5%) | |
| 9–10 | 480 (33.0%) | 80 (21.3%) | 286 (44.0%) | |
| Employment status B | N = 1467 | N = 381 | N = 650 | |
| Retired | 963 (65.6%) | 201 (52.8%) | 488 (75.1%) | |
| Working full-time | 166 (11.3%) | 58 (15.2%) | 48 (7.4%) | |
| Working part-time | 171 (11.7%) | 55 (14.4%) | 63 (9.7%) | |
| Casual work | 63 (4.3%) | 20 (5.3%) | 21 (3.2%) | |
| Volunteer work | 144 (9.8%) | 21 (5.5%) | 88 (13.5%) | |
| Unemployed and looking for work | 22 (1.5%) | 8 (2.1%) | 6 (0.9%) | |
| Unemployed and not looking for work | 14 (1.0%) | 11 (2.9%) | 1 (0.2%) | |
| Student | 7 (0.5%) | 3 (0.8%) | 3 (0.5%) | |
| Carer | 32 (2.2%) | 12 (3.2%) | 13 (2.0%) | |
| Disability support pension | 45 (3.1%) | 23 (6.0%) | 10 (1.5%) | |
| Other | 51 (3.5%) | 13 (3.4%) | 28 (4.3%) | |
| Sexual orientation | N = 1085 | N = 380 | N = 647 | |
| Heterosexual | 924 (85.2%) | 325 (85.5%) | 545 (84.2%) | |
| Homosexual (lesbian or gay) | 76 (7.0%) | 26 (6.8%) | 48 (7.4%) | |
| Bisexual | 46 (4.2%) | 19 (5.0%) | 25 (3.9%) | |
| Asexual | 12 (1.1%) | 2 (0.5%) | 10 (1.6%) | |
| Something else | 27 (2.5%) | 8 (2.1%) | 19 (2.9%) | |
| Relationship status | N = 1087 | N = 380 | N = 651 | |
| Living with my husband/wife/partner | 672 (61.8%) | 215 (56.6%) | 421 (64.7%) | |
| Single and not dating | 183 (16.8%) | 73 (19.2%) | 101 (15.5%) | |
| Committed relationship, living in separate houses | 92 (8.5%) | 35 (9.2%) | 56 (8.6%) | |
| Single and dating | 33 (3.0%) | 19 (5.0%) | 13 (2.0%) | |
| Long-distance relationship with a partner I have met in person | 31 (2.9%) | 12 (3.2%) | 14 (2.2%) | |
| Long-distance relationship with a partner I have not met in person | 8 (0.7%) | 2 (0.5%) | 4 (0.6%) | |
| Something else | 68 (6.3%) | 24 (6.3%) | 42 (6.5%) | |
Two thirds of respondents were retired (65.6%), one quarter were working either full-time, part-time or casually (27.1%), and the remainder designated other employment statuses (Table 3). Participants were able to state their occupation in a free-text question and gave a wide range of current or past jobs including cafe owner, dentist, taxi driver, teacher, public servant, mail sorter, corrections officer, farmer, flight attendant, nurse, and minister of religion among others.
Of those who answered the sexual orientation question (73.8% of participants), the majority were heterosexual (85.2%), and 11.2% either homosexual or bisexual (Table 3). Of those who answered the relationship status question (73.9% of participants), three out of five (61.8%) were in a cohabiting relationship with their spouse or partner, 19.8% were single and either dating or not-dating, while 8.5% were in a committed relationship but living separately, sometimes termed a LAT relationship (living apart together)38 (Table 3). It was not feasible to compare with ABS or SA&M as these data were categorised differently across datasets.
Discussion
In this paper, we outline the recruitment methods and sample obtained from the SHAPE2 online sexual health survey of older adults in Australia conducted in 2021. Our results can be summarised by three main findings. First, we found that older adults are willing to participate in online research, including on the sensitive topic of sexual health. Second, the recruitment methods of combining emails to organisations and paid Facebook advertising were successful for obtaining a fairly large and representative convenience sample on a low budget. Third, participants recruited via Facebook had different characteristics from those recruited via other means. We also identified certain similarities and differences with the sample collected for SA&M 6 years earlier and discuss these below.
Sample demographics
Our sample closely represented Australian population data in terms of gender, with around a 1:1 ratio of males and females. This was different from SA&M where men were overrepresented with a 2:1 ratio between males and females. As older men are typically earlier technology adopters than older women,33,39 this may be indicative of older women’s increasing engagement with technology in recent years. Additionally, one of our Facebook advertisements was displayed to older women only, which helped correct an initial gender discrepancy, demonstrating the utility of targeted advertising.
While we captured a wide range of ages, our sample was skewed toward the younger age bands, particularly for those recruited via Facebook. The SHAPE2 sample was less skewed towards younger age groups than SA&M, but both were affected by this overrepresentation of younger ages. As co-morbidities and cognitive challenges increase with age, and rates of internet access decline with age,40 it is unsurprising that fewer of the oldest age groups participated. This does, however, represent a limitation of SHAPE2 as it did for SA&M.
Geographical distribution by State/Territory was broadly reflective of national statistics, with the exception of the Australian Capital Territory (ACT) which was over-represented in the SHAPE2 sample. Our sample was, however, less representative by State/Territory than SA&M, with the reason for this disparity unknown. In 2020, 65.9% of Australians over 65 years were living in Major Cities, 32.6% in Inner or Outer Regional areas, and 1.5% in Remote and Very Remote settings,41 which is close to the proportions of the SHAPE2 sample. These findings demonstrate that the recruitment methods used were effective at reaching Australians from a wide range of locations.
It is estimated that between 4%42,43 and 10%44 of the Australian general population identify as lesbian, gay or bisexual, indicating that our sample (11.2% homosexual or bisexual) is over representative of minority sexual orientations. Of the SA&M sample, 10.3% identified as gay, lesbian or bisexual, suggesting similarities in recruitment and/or a higher level of interest in sexual health research among sexual minority communities. A small number of the organisations emailed to promote the SHAPE2 study were LGBT specific, which likely increased participation among these demographics.
A similarity between SHAPE2 and SA&M is that both studies exceeded their initial targets during the early stages of recruitment. SA&M initially aimed to recruit 600 participants, but adjusted their goal upwards after receiving over 300 responses in the first week.30 SHAPE2 initially aimed to recruit 500 people over 2 months and adjusted this upwards after exceeding this number in the first month of recruitment. This strong response rate builds on the existing research, showing that older adults are willing to participate in sexual health research and are amenable to doing so online.30,45
Social media vs other recruitment methods
Many older Australians are online, particularly the ‘younger-old’ aged in their 60s and 70s40 and many are using social media, with Facebook the most popular platform for older age groups.46 Just over a third of our sample found out about the survey via Facebook, contributing to the evidence that social media is effective for recruiting older people for sexual health surveys,30,45 much as it has been shown to be effective for recruiting young people for sexual health research47,48 and for recruiting diverse and hard to reach populations for health research broadly.49
A greater proportion of our sample, however, came via newsletters/organisations or clubs (contacted by email during Phase 1). This is in contrast to SA&M, which recruited around half their sample from Facebook and a smaller proportion from newsletters/organisations or clubs. These differences in recruitment methods may contribute to why our sample was a better fit to ABS population data. While our email campaign was effective, it was not highly efficient. During Phase 1, recruitment we sent out approximately 2500 emails. Given that only 541 people indicated they found out about the survey via a newsletter or group, this shows that this recruitment method is labour-intensive and low yield, with most emails generating no response. Additionally, a potential limitation of the SHAPE2 sample is that it may over-represent the types of people who are involved in community groups and clubs.
By the end of recruitment Phases 1 and 2, we had recruited 1417 participants, representing 96% of our final sample. The low number recruited during Phase 3 of passive recruitment shows that few people accessed the survey through onwards-sharing after the active recruitment phase, demonstrating minimal benefit from leaving the survey open.
In comparing those in our sample recruited via Facebook with those recruited via other means, Facebook recruits tended to be younger (median age of 67 years as compared to 69 years for the overall sample) and were less likely to be retired. This finding that Facebook is more effective for recruiting the ‘younger-old’ is consistent with a 2017 online survey of dementia caregivers in the United States that found Facebook effective for recruiting participants aged 65–74 years, but not for those aged 75 years and over.50 They were slightly less likely to be in major cities and were more evenly spread across socio-economic deciles, whereas those recruited via other means disproportionately came from the highest deciles. They were also more likely to be female, however, this is attributable to part of the Facebook campaign being targeted only to women.
Strengths and limitations
A strength of SHAPE2 recruitment was the low budget used to recruit a sizeable sample. Our experience shows that a mixture of email promotion combined with Facebook advertising is not only feasible, but also economical for recruitment. While the reach of paid Facebook advertising is dependent on the amount of money spent, even our modest budget yielded good results. The SA&M researchers also found Facebook advertising to be ‘a cost-effective strategy’.30
While our recruitment strategies were effective, there are some limitations to our sample and its generalisability, as have been observed in other internet surveys of older adults.51 Older Australians are using the internet more than ever however not all are online, particularly those aged 85 years and over.40 As with other online-only surveys of older adults, people who are not online would not have been able to participate.39 One prospective participant who saw the flyer posted on a community noticeboard phoned to request paper copies for themself and others who did not have internet access. We posted out these hard copies, however, it would not have been financially feasible to include hard copy distribution as a core component of the recruitment strategy. There may also have been others without internet access who were interested, but who did not contact us. It is unclear, however, how effective it would have been to include hard copy distribution as part of our recruitment strategy. SA&M distributed hard copies, but few were returned, with the vast majority completing the survey online.30 This suggests that paper surveys are not preferred by many older adults, and those who are harder to reach would require a more resource-intensive approach to access them beyond the mere provision of a hard copy format. Including reply-paid envelopes was likely an important factor in the majority (96.6%) of 1876 survey responses of Australian retirement village residents being returned in paper format (only 3.4% online) in a 2015 study.52
A limitation of the SHAPE2 study is that it was only available in English; thus, people who do not read and write English confidently would have been unable to participate. Additionally, we did not include a question about ethnicity or country of birth in the demographic questions for our survey and as a result we do not know how representative the sample was in this respect.
Conclusion
This paper discusses the recruitment of older Australians for a sexual health survey, given sexual health is of increasing importance to Australia’s ageing population. In common with the similar SA&M study, we found that older adults are willing to participate in online sexual health research and that recruitment via social media is effective. In contrast with SA&M, the SHAPE2 sample was more representative in terms of gender and age, possibly attributable to the differences in recruitment and to changes in online engagement among older adults in the intervening years. These findings can help inform the design of future online surveys seeking to recruit older participants, particularly in researching sexual health and other sensitive topics.
Data availability
The data that support this study cannot be publicly shared due to ethical or privacy reasons and may be shared upon reasonable request to the corresponding author if appropriate.
References
1 Freak-Poli R, Kirkman M, De Castro Lima G, Direk N, Franco OH, Tiemeier H. Sexual activity and physical tenderness in older adults: cross-sectional prevalence and associated characteristics. J Sex Med 2017; 14(7): 918-927.
| Crossref | Google Scholar | PubMed |
2 Heywood W, Lyons A, Fileborn B, Hinchliff S, Minichiello V, Malta S, et al. Sexual satisfaction among older Australian heterosexual men and women: findings from the Sex, Age & Me study. J Sex Marital Ther 2018; 44(3): 295-307.
| Crossref | Google Scholar | PubMed |
3 Fisher L. Sex, romance, and relationships: AARP survey of midlife and older adults. Washington, D.C.: AARP; 2010. Available at http://www.aarp.org/research/topics/life/info-2014/srr_09.html [cited 25 November 2019]
4 Gott M, Hinchliff S. How important is sex in later life? The views of older people. Soc Sci Med 2003; 56(8): 1617-1628.
| Crossref | Google Scholar | PubMed |
5 Lindau ST, Schumm LP, Laumann EO, Levinson W, O’Muircheartaigh CA, Waite LJ. A study of sexuality and health among older adults in the United States. N Engl J Med 2007; 357(8): 762-774.
| Crossref | Google Scholar |
6 Fileborn B, Thorpe R, Hawkes G, Minichiello V, Pitts M, Dune T. Sex, desire and pleasure: considering the experiences of older Australian women. Sex Relation Ther 2015; 30(1): 117-130.
| Crossref | Google Scholar | PubMed |
7 Santos-Iglesias P, Byers ES, Moglia R. Sexual well-being of older men and women. Canad J Hum Sex 2016; 25(2): 86-98.
| Crossref | Google Scholar |
8 Lee DM, Nazroo J, O’Connor DB, Blake M, Pendleton N. Sexual health and well-being among older men and women in England: findings from the English Longitudinal Study of Ageing. Arch Sex Behav 2016; 45(1): 133-144.
| Crossref | Google Scholar | PubMed |
9 Ševčíková A, Sedláková T. The role of sexual activity from the perspective of older adults: a qualitative study. Arch Sex Behav 2020; 49: 969-981.
| Crossref | Google Scholar | PubMed |
10 Schick V, Herbenick D, Reece M, Sanders SA, Dodge B, Middlestadt SE, et al. Sexual behaviors, condom use, and sexual health of Americans over 50: implications for sexual health promotion for older adults. J Sex Med 2010; 7(S5): 315-329.
| Crossref | Google Scholar |
11 Palacios-Ceña D, Carrasco-Garrido P, Hernández-Barrera V, Alonso-Blanco C, Jiménez-García R, Fernández-de-las-Peñas C. Sexual behaviors among older adults in Spain: results from a population-based national sexual health survey. J Sex Med 2012; 9(1): 121-129.
| Crossref | Google Scholar | PubMed |
12 Malta S. Love, sex and intimacy in new late-life romantic relationships. Swinburne University of Technology; 2013. Available at https://researchbank.swinburne.edu.au/file/3db6aba6-fd1b-4c99-a9cf-166bce839a92/1/Sue%20Malta%20Thesis.pdf
13 Bourchier L, Malta S, Temple-Smith M, Hocking J. Do we need to worry about sexually transmissible infections (STIs) in older women in Australia? An investigation of STI trends between 2000 and 2018. Sex Health 2020; 17(6): 517-524.
| Crossref | Google Scholar |
14 Kirby Institute. HIV, viral hepatitis and sexually transmissible infections in Australia: annual surveillance report 2022. Sydney: Kirby Institute, UNSW; 2018. Available at https://www.kirby.unsw.edu.au/sites/default/files/documents/Annual-Surveillance-Report-2022_STI.pdf [cited 1 December 2023]
15 Bodley-Tickell AT, Olowokure B, Bhaduri S, White DJ, Ward D, Ross JDC, et al. Trends in sexually transmitted infections (other than HIV) in older people: analysis of data from an enhanced surveillance system. Sex Transm Infect 2008; 84(4): 312-317.
| Crossref | Google Scholar |
16 Minichiello V, Rahman S, Hawkes G, Pitts M. STI epidemiology in the global older population: emerging challenges. Perspect Public Health 2012; 132(4): 178-181.
| Crossref | Google Scholar | PubMed |
17 Poynten IM, Grulich AE, Templeton DJ. Sexually transmitted infections in older populations. Curr Opin Infect Dis 2013; 26(1): 80-85.
| Crossref | Google Scholar | PubMed |
18 Cheng Y, McGeechan K, Bateson D, Ritter T, Weisberg E, Stewart M. Age differences in attitudes toward safer sex practices in heterosexual men using an Australian Internet dating service. Sex Health 2018; 15(3): 223-231.
| Crossref | Google Scholar | PubMed |
19 Bateson DJ, Weisberg E, McCaffery KJ, Luscombe GM. When online becomes offline: attitudes to safer sex practices in older and younger women using an Australian internet dating service. Sex Health 2012; 9(2): 152-159.
| Crossref | Google Scholar | PubMed |
20 Stewart M, Ritter T, Bateson D, McGeechan K, Weisberg E. Contraception – what about the men? Experience, knowledge and attitudes: a survey of 2438 heterosexual men using an online dating service. Sex Health 2017; 14(6): 533-539.
| Crossref | Google Scholar | PubMed |
21 de Visser RO, Badcock PB, Rissel C, Richters J, Smith AMA, Grulich AE, et al. Safer sex and condom use: findings from the Second Australian Study of Health and Relationships. Sex Health 2014; 11(5): 495-504.
| Crossref | Google Scholar | PubMed |
22 Fileborn B, Lyons A, Heywood W, Hinchliff S, Malta S, Dow B, et al. Talking to healthcare providers about sex in later life: findings from a qualitative study with older Australian men and women. Australas J Ageing 2017; 36(4): E50-E56.
| Google Scholar | PubMed |
23 Malta S, Hocking JS, Lyne J, McGavin D, Hunter J, Bickerstaffe A, et al. Do you talk to your older patients about sexual health? Health practitioners’ knowledge of, and attitudes towards, management of sexual health among older Australians. Aust J Gen Pract 2018; 47(11): 807-811.
| Crossref | Google Scholar |
24 Malta S, Temple-Smith M, Bickerstaffe A, Bourchier L, Hocking J. ‘That might be a bit sexy for somebody your age’: older adult sexual health conversations in primary care. Australas J Ageing 2020; 39(S1): 40-48.
| Crossref | Google Scholar |
25 Lyons A, Heywood W, Fileborn B, Minichiello V, Barrett C, Brown G, et al. Sexually active older Australian’s knowledge of sexually transmitted infections and safer sexual practices. Aust N Z J Public Health 2017; 41(3): 259-261.
| Crossref | Google Scholar | PubMed |
26 Bourne C, Minichiello V. Sexual behaviour and diagnosis of people over the age of 50 attending a sexual health clinic. Australas J Ageing 2009; 28(1): 32-36.
| Crossref | Google Scholar | PubMed |
27 Heywood W, Lyons A, Fileborn B, Minichiello V, Barrett C, Brown G, et al. Self-reported testing and treatment histories among older Australian men and women who may be at risk of a sexually transmissible infection. Sex Health 2017; 14(2): 139-146.
| Crossref | Google Scholar | PubMed |
28 Fileborn B, Lyons A, Hinchliff S, Brown G, Heywood W, Dow B, et al. Improving the sexual lives of older Australians: perspectives from a qualitative study. Australas J Ageing 2017; 36(4): E36-E42.
| Crossref | Google Scholar | PubMed |
29 Richters J, Badcock PB, Simpson JM, Shellard D, Rissel C, de Visser RO, et al. Design and methods of the Second Australian Study of Health and Relationships. Sex Health 2014; 11(5): 383-396.
| Crossref | Google Scholar |
30 Lyons A, Heywood W, Fileborn B, Minichiello V, Barrett C, Brown G, et al. The Sex, Age, and Me study: recruitment and sampling for a large mixed-methods study of sexual health and relationships in an older Australian population. Cult Health Sex 2017; 19(9): 1038-1052.
| Crossref | Google Scholar | PubMed |
31 Grulich AE, de Visser RO, Badcock PB, Smith AMA, Richters J, Rissel C, et al. Knowledge about and experience of sexually transmissible infections in a representative sample of adults: the Second Australian Study of Health and Relationships. Sex Health 2014; 11(5): 481-494.
| Crossref | Google Scholar | PubMed |
32 Watchirs Smith L, Guy R, Degenhardt L, Yeung A, Rissel C, Richters J, et al. Meeting sexual partners through internet sites and smartphone apps in Australia: national representative study. J Med Internet Res 2018; 20(12): e10683.
| Crossref | Google Scholar |
33 Badcock PB, Patrick K, Smith AMA, Simpson JM, Pennay D, Rissel CE, et al. Differences between landline and mobile phone users in sexual behavior research. Arch Sex Behav 2017; 46(6): 1711-1721.
| Crossref | Google Scholar | PubMed |
34 Malta S, Temple-Smith M, Hunter J, McGavin D, Lyne J, Bickerstaffe A, et al. Could an online or digital aid facilitate discussions about sexual health with older Australians in general practice? Aust J Gen Pract 2018; 47(12): 870-875.
| Crossref | Google Scholar |
35 Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of internet E-surveys (CHERRIES). J Med Internet Res 2004; 6(3): e34.
| Crossref | Google Scholar | PubMed |
36 Australian Bureau of Statistics (ABS). 2017 postcode to 2016 remoteness area. Canberra; 2018. Available at https://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/1270.0.55.005July%202016?OpenDocument [cited 5 August 2022]
37 Australian Bureau of Statistics (ABS). Postal area, indexes, SEIFA 2016. Canberra; 2018. Available at https://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/2033.0.55.0012016?OpenDocument [cited 5 August 2022]
38 Levin I. Living apart together: a new family form. Curr Soc 2004; 52(2): 223-240.
| Crossref | Google Scholar |
39 Kelfve S, Kivi M, Johansson B, Lindwall M. Going web or staying paper? The use of web-surveys among older people. BMC Med Res Methodol 2020; 20(1): 252.
| Crossref | Google Scholar | PubMed |
40 Australian Bureau of Statistics (ABS). 2018 survey of disability, ageing and carers: use of information technology. Canberra; 2019. Available at https://www.abs.gov.au/statistics/health/disability/disability-ageing-and-carers-australia-summary-findings/latest-release [cited 11 August 2022]
41 Australian Institute of Health and Welfare (AIHW). GEN aged care data snapshot 2020 – third release. Canberra: GEN; 2020. Available at https://gen-agedcaredata.gov.au/Resources/Access-data/2020/October/Aged-care-data-snapshot%E2%80%942020
42 Australian Bureau of Statistics (ABS). General social survey: summary results, Australia. 2021. Available at https://www.abs.gov.au/statistics/people/people-and-communities/general-social-survey-summary-results-australia/2020 [cited 9 October 2021]
43 Wilson T, Temple J, Lyons A, Shalley F. What is the size of Australia’s sexual minority population? BMC Res Notes 2020; 13(1): 535.
| Crossref | Google Scholar | PubMed |
44 Rahman Q, Xu Y, Lippa RA, Vasey PL. Prevalence of sexual orientation across 28 nations and its association with gender equality, economic development, and individualism. Arch Sex Behav 2020; 49(2): 595-606.
| Crossref | Google Scholar | PubMed |
45 Malta S. Using online methods to interview older adults about their romantic and sexual relationships. In: Leontowisch M, editor. Researching later life and ageing: expanding qualitative research horizons. London: Palgrave Macmillan; 2012. p. 146–172. Available at https://doi.org/10.1057/9781137271372
46 Australian Communications and Media Authority (ACMA). Communications and media in Australia: how we communicate. 2021. Available at https://www.acma.gov.au/publications/2021-12/report/communications-and-media-australia-how-we-communicate [cited 7 December 2022]
47 Harfield S, Elliott S, Ramsey L, Housen T, Ward J. Using social networking sites to recruit participants: methods of an online survey of sexual health, knowledge and behaviour of young South Australians. Aust N Z J Public Health 2021; 45(4): 348-354.
| Crossref | Google Scholar | PubMed |
49 Whitaker C, Stevelink S, Fear N. The use of Facebook in recruiting participants for health research purposes: a systematic review. J Med Internet Res 2017; 19(8): e290.
| Crossref | Google Scholar | PubMed |
50 Corey KL, McCurry MK, Sethares KA, Bourbonniere M, Hirschman KB, Meghani SH. Utilizing Internet-based recruitment and data collection to access different age groups of former family caregivers. Appl Nurs Res 2018; 44: 82-87.
| Crossref | Google Scholar | PubMed |
51 Remillard ML, Mazor KM, Cutrona SL, Gurwitz JH, Tjia J. Systematic review of the use of online questionnaires of older adults. J Am Geriatr Soc 2014; 62(4): 696-705.
| Crossref | Google Scholar | PubMed |
52 Malta S, Williams SB, Batchelor FA. ‘An ant against an elephant’: retirement village residents’ experiences of disputes and dispute resolution. Australas J Ageing 2018; 37(3): 202-209.
| Crossref | Google Scholar | PubMed |
53 Australian Bureau of Statistics (ABS). National, state and territory population, June 2021. Canberra; 2021. Available at https://www.abs.gov.au/statistics/people/population/national-state-and-territory-population/latest-release