Supporting best practice in the management of chronic diseases in primary health care settings: a scoping review of training programs for Indigenous Health Workers and Practitioners
Odette Pearson A B * , Shwikar Othman A B , Kate Colmer C , Sana Ishaque C , Gloria Mejia D , Sarah Crossing A , David Jesudason B E , Gary Wittert B F , Paul Zimmet G , Sophia Zoungas H , Natalie Wischer I , Kim Morey A B , Jane Giles C , Sara Jones J , Alex Brown K L and Saravana Kumar JA
B
C
D
E
F
G
H
I
J
K
L
Abstract
To improve diabetes management in primary health care for the Aboriginal and Torres Strait Islander peoples population, training programs that are culturally and contextually relevant to the local context are required. Using a scoping review methodology, the aim of this review was to describe the characteristics of chronic disease management training programs for Aboriginal Health Workers and Practitioners, their effectiveness on knowledge and skills, and client-related outcomes, and the enablers, barriers to delivery and participation.
Following protocol parameters, a systematic search was conducted in relevant databases and grey literature. Two independent reviewers screened the title and abstract of each paper to determine if the study met the inclusion criteria.
Of the 23 included studies, most were developed with stakeholders, profession facilitated and delivered by cultural facilitators. All training programs included content knowledge, two included a professional support network, four provided on-the-job support and six had follow-up support post-training. Modes of delivery ranged from didactic, storytelling and hands-on learning. Two studies reported significant improvement in participants’ knowledge and confidence; one reported improvement in knowledge (12.7% increase pre-post training), and an increase in confidence in both clinical and non-clinical skills. Enablers (relevance, modes of learning, power of networking, improved knowledge, confidence and clinical practice) and barriers (adult learning capabilities, competing work-family commitments) were reported. Few studies reported on knowledge transfer into clinical practice and client-related outcomes.
Multifaceted training programs for Aboriginal health workers are well received and may improve workforce capability.
Keywords: Aboriginal health workers, chronic disease management, chronic diseases, community health workers, indigenous health workers, primary health care setting, scoping review, training programs, workforce.
Introduction
Aboriginal and Torres Strait Islander peoples are the first peoples of Australia, and are known to have the longest continuing culture in the world. However, the colonisation of Australia and its ongoing legacy has resulted in Aboriginal and Torres Strait Islander peoples bearing the burden of ill health, and having to continually advocate for better health and social outcomes. Chronic disease prevalence in the Aboriginal and Torres Strait Islander peoples population is significantly high, and accounts for 70% of the health gap between Aboriginal and non-Aboriginal Australians (AIHW 2016). Most chronic diseases are managed in primary health care settings. In Australia, National Aboriginal Community Controlled Health Organisations are the main primary health care provider for the Aboriginal and Torres Strait Islander peoples population, with more than 140 services across Australia and >50% of the population accessing these services (Gomersall et al. 2017; National Aboriginal Community Controlled Health Organisation (NACCHO) 2019). An integral position within the Aboriginal Community Controlled Health Organisation sector is the Aboriginal and Torres Strait Islander Health Worker (AHW) role established in the 1950s, and the more recently established (2006) Aboriginal and Torres Strait Islander Health Practitioner (AHP) role.
The minimum qualification of an AHW is a Certificate III in Aboriginal Primary Health Care, and for an AHP a Certificate IV in Aboriginal Primary Health Care. Numerous Registered Training Organisations across Australia deliver the qualifications, and the AHP profession has a practice registration board (Aboriginal and Torres Strait Islander Health Practice Board 2020). Skills and knowledge of both professions include clinical competencies and/or community education and health promotion, and provision of culturally appropriate, community-responsive and holistic health care (Harfield et al. 2018). However, regardless of the unique role of Aboriginal Health Workers and Practitioners (AHW/P) in the Australian health workforce, there is no nationally recognised scope of practice. These two professions have a responsibility to recognise and work within their competency levels and the scope of practice relevant to their specific role within a service. To support this, the National Aboriginal and Torres Strait Islander Health Worker Workforce Association has developed a national framework for determining the individual scope of practice for AHWs and AHPs (National Aboriginal and Torres Strait Islander Health Worker Association 2012; NSW Ministry of Health 2018; National Aboriginal Community Controlled Health Organisation (NACCHO) 2019; Aboriginal and Torres Strait Islander Health Practice Board 2020).
A growing body of evidence links the AHW/P workforce to improved health outcomes in diabetes care, mental health care, maternal and infant care, and palliative care (Croager et al. 2010; National Aboriginal Community Controlled Health Organisation (NACCHO) 2019). Despite the high prevalence of type 2 diabetes and its related complications among the Aboriginal and Torres Strait Islander community (Hare et al. 2022), diabetes management within the current core content of both qualifications is limited. Two new diabetes electives have recently become available; however, not all local Registered Training Organisations will offer these electives (Australian Government 2022).
Despite limited trial evidence available (Glazier et al. 2006), training interventions developed for mainstream populations have less effect in disadvantaged populations than those that are culturally and contextually relevant to the population. This aligns with the call to develop a health professional workforce that is ‘fit for purpose’ – a context-relevant workforce that understands the health system, and is aligned to the needs and culture of the community they serve (Pálsdóttir et al. 2016). Few trials have sought to implement and evaluate novel workforce approaches to reducing differential diabetes-related outcomes in the Aboriginal and Torres Strait Islander population (McDermott et al. 2015). However, models exist specifically designed for developing, implementing and evaluating workplace training, such as the New World Kirkpatrick Model (Kirkpatrick and Kirkpatrick 2016). The model highlights that effective training leads to improved job performance that positively contributes to outcomes for clients. Training that focuses on the identified ‘on the job’ behaviours is more likely to lead to an increase in work performance, thus, maximising results for organisations and clients (Kirkpatrick and Kirkpatrick 2016).
There is a range of terms used internationally to describe the role of Indigenous peoples worldwide who are health professionals with fundamental knowledge and skills to work in primary health care settings, and provide culturally safe health care for Indigenous peoples and communities (Aboriginal and Torres Strait Islander Health Practice Board 2020). This includes Community Health Workers, Indigenous Health Workers (IHWs), Community Health Representatives (CHRs), Community Support Workers and Community Health Aides and Practitioners. In Australia, AHWs and AHPs comprise this workforce. As such, AHW/P will be used in the body of this paper.
The aim of this review was to describe the characteristics of chronic disease management training programs for AHW/P, including the barriers, enablers and challenges to delivery and participation across the international literature. This review informs a larger project, ‘Translation of culturally and contextually informed diabetes training for Aboriginal health practitioners on Aboriginal client’s outcomes: a cluster randomised trial of effectiveness’ funded by the Medical Research Future Fund Primary Health Care Research Initiative (#APP1200314). The larger project directly responds to an Aboriginal primary health care workforce identified priority within the South Australian Aboriginal Diabetes Strategy (Gibson et al. 2016). The review brings Aboriginal and Torres Strait Islander peoples’ ways of knowing, being and doing to the forefront in applying the western scoping review methodology. Using a collaborative and relational rights-based approach co-led by an Aboriginal and non-Aboriginal multidisciplinary team of researchers aims to centre Aboriginal ways of knowing. By doing so, the Aboriginal and Torres Strait Islander peoples’ worldviews and lived experiences across health and workforce training contexts are reflected in this review. Specifically, the scoping review findings will inform the development, delivery and evaluation of a comprehensive, culturally and contextually informed diabetes training program for the Aboriginal primary health care workforce, in particular Aboriginal health workers and practitioners.
Review questions
The review questions are:
What are the characteristics of chronic disease training programs for AHW/P, inclusive of the way in which the training programs are developed, delivered, depth and scope of content, facilitated, by whom, the length of time, and how they are evaluated?
From the perspectives of AHW/P, those delivering the training, health care managers and evaluators, what are the enablers and barriers or challenges in providing chronic disease training programs for AHW/P?
What are the outcomes of chronic disease training programs on knowledge, attitudes, practice and skills of AHW/P and client-related outcomes?
Review context
This review was undertaken by Wardliparingga, Aboriginal Health Equity Theme, at South Australian Health and Medical Research Institute. This unit undertakes community-identified research with the aim of improving the health and wellbeing of Aboriginal and Torres Strait Islander peoples in Australia. The co-theme leaders of Aboriginal Health Equity (OP, KM) and the inaugural theme leader (AB) are authors of this review. A/Prof Odette Pearson is a Kuku Yalanji/Torres Strait Islander and Co-Theme Leader in Wardliparingga Aboriginal Health Equity. Odette brings experience working in remote area primary health care settings within Australia, combined with her research knowledge on comprehensive diabetes management within Aboriginal primary health care settings. Professor Alex Brown is an Aboriginal medical doctor and researcher, who over the past 20 years has established an extensive and unique research program with a particular focus on outlining and overcoming health disparities among the Aboriginal Australian population. A/Prof Kim Morey is of Anmatyerre/Eastern Arrernte descent with family connections to Central Australia, with >25 years of experience in Aboriginal and Torres Strait Islander peoples health and community services, across policy, planning, service development, monitoring and systems performance, including 10 years in Aboriginal and Torres Strait Islander peoples health research. The review team comprises of researchers, clinicians and academics who work within Aboriginal primary care settings and/or have expertise in developing education and training programs and knowledge synthesis, in addition to connections with the Aboriginal and Torres Strait Islander peoples communities in South Australia.
Methods
The scoping review protocol was registered through the Open Science Framework that describes in detail the methodology (Colmer et al. 2020). The review followed the Joanna Briggs Institute approach (Peters et al. 2020), and was reported following the Preferred Reporting Items for Systematic Reviews and Meta-analyses Extension for Scoping Review (PRISMA-ScR; Moher et al. 2009; Tricco et al. 2018).
To determine effectiveness of training programs, the New World Kirkpatrick Model (Kirkpatrick Model) was used as a framework (Kirkpatrick and Kirkpatrick 2016). The framework defines four levels of evaluation: reaction of the participants to the training program (level 1); participant learning, including attitude, knowledge and confidence related to the topic/s (level 2), behaviour, including application and sharing learnt knowledge with families, friends and community (level 3); and client-related outcomes, such as improved medication compliance and attending follow-up appointments (level 4).
Eligibility criteria
The population, interest and context are outlined below in Table 1.
Exclusion criteria
This review excluded studies whose primary participants are patients and/or community members or other health professions, such as doctors, allied health workers or nurses; studies that included training programs developed for hospital-based care or that do not specify the health care setting; or training programs that focused on health promotion, early detection or screening. Opinions, commentaries and conference presentations were also excluded.
Search strategy (information sources)
The search strategy was developed in consultation with an academic librarian from the University of Adelaide. It included studies published in English from 1 January 1970 until 17 January 2022. The start year of the search coincides with the establishment of Aboriginal health workers across all Australian jurisdictions (National Rural Health Alliance Inc. 2006). PubMed, Embase, CINAHL, Informit: Indigenous Peoples, SCOPUS, MedNar, Trove, Proquest Dissertations & Theses Database, Google Advanced, Australian Institute of Aboriginal and Torres Strait Islander Studies, Australian Indigenous Health InfoNet, Primary Health Care Research & Information Service (PHCRIS), and the Lowitja Institute were searched using keywords and index terms that are provided (see Supplementary Appendix 1). In addition, the reference lists of all identified reports and articles were searched for additional studies.
Criteria and process
Following the search, all identified citations were uploaded to Covidence (Veritas Health Innovation 2018), and duplicates were removed. The title and abstracts of retrieved citations were reviewed against the inclusion criteria. One reviewer (KC) started the title and abstract reviews of the literature, and found that the protocol criteria of excluding one-off training sessions meant that potential studies of interest would be excluded. The review team felt it was important to compare training timings to see if there was a difference between one-off and ongoing training; for example, how does a 1-day workshop compare with 7 weeks of 1-h sessions. The exclusion criteria were modified to reflect this change.
Three independent reviewers (KC, GM, ET) screened all titles and abstracts (GM and ET screened half each). Following this, two independent reviewers (OP, KC) screened the full texts of the remaining articles, and detailed reasons for exclusion were recorded. Disagreements between the reviewers at each stage of the selection process were resolved through discussion or with additional reviewers (OP, SK).
Data extraction
Data were extracted by three independent reviewers (KC, SC, SO) using an agreed-upon template developed in Microsoft Excel. Extraction fields included, but were not limited to, author, year, study design, country (cultural and geographical), health care setting, health worker title and role, sample size, chronic disease focus, aim of the training program, curriculum, development phase, training characteristics, cultural facilitation, and a description of any on the job clinical support. A second Excel tab was used to map the effectiveness of the training program against the Kirkpatrick Model (Kirkpatrick and Kirkpatrick 2016). Fields included: learner outcome measures, satisfaction (level 1), learning, knowledge and confidence (clinical and non-clinical skills) and attitude (level 2), behaviour (level 3), and reported findings and clients’ related outcomes (level 4). Enablers, barriers, challenges, limitations and recommendations from the perspective of participants, managers and evaluators were also extracted.
Data synthesis
Studies were predominantly descriptive, so a narrative synthesis was conducted in addition to reporting statistical data. Studies’ findings were synthesised, and grouped according to study design, health condition, population characteristics and study characteristics. In addition, a summary of where the studies were conducted, sample size, length of training, level of evaluation used and effectiveness were reported.
In terms of the qualitative studies’ findings, the data synthesis involved meta-aggregation that included categorising and re-categorising the findings. These findings were identified by repeated reading of text of the included articles. Where available, direct themes, subthemes and metaphors were extracted as findings from the included articles, each finding was accompanied by one or more illustrations that supported the finding. An illustration was either a direct quotation representing a participant’s voice, authors’ observations or other supportive data (Munn et al. 2014a). Findings were also assigned one of the three levels of credibility according to the following criteria: (1) ‘unequivocal’: findings accompanied by an illustration that is not open to challenge, (2) ‘equivocal’: findings accompanied by an illustration that is open to challenge, and (3) ‘unsupported’: findings that are not supported by data. The decision to allocate the finding a level of credibility was discussed and collectively agreed upon by reviewers (SI, OP, SC, SO) based on their understanding of the degree of suitability between the finding and the supporting illustration(s). Unsupported findings were not included in the synthesis.
Unequivocal and equivocal findings were combined into author-identified categories based on the similarity in concept/meaning. There were at least two findings per category. Each category was given a description created by consensus between reviewers (SI, OP, SO). Synthesised findings were then created by combining at least two or more categories supported by findings and illustrations.
Results
Study inclusion (selection of sources of evidence)
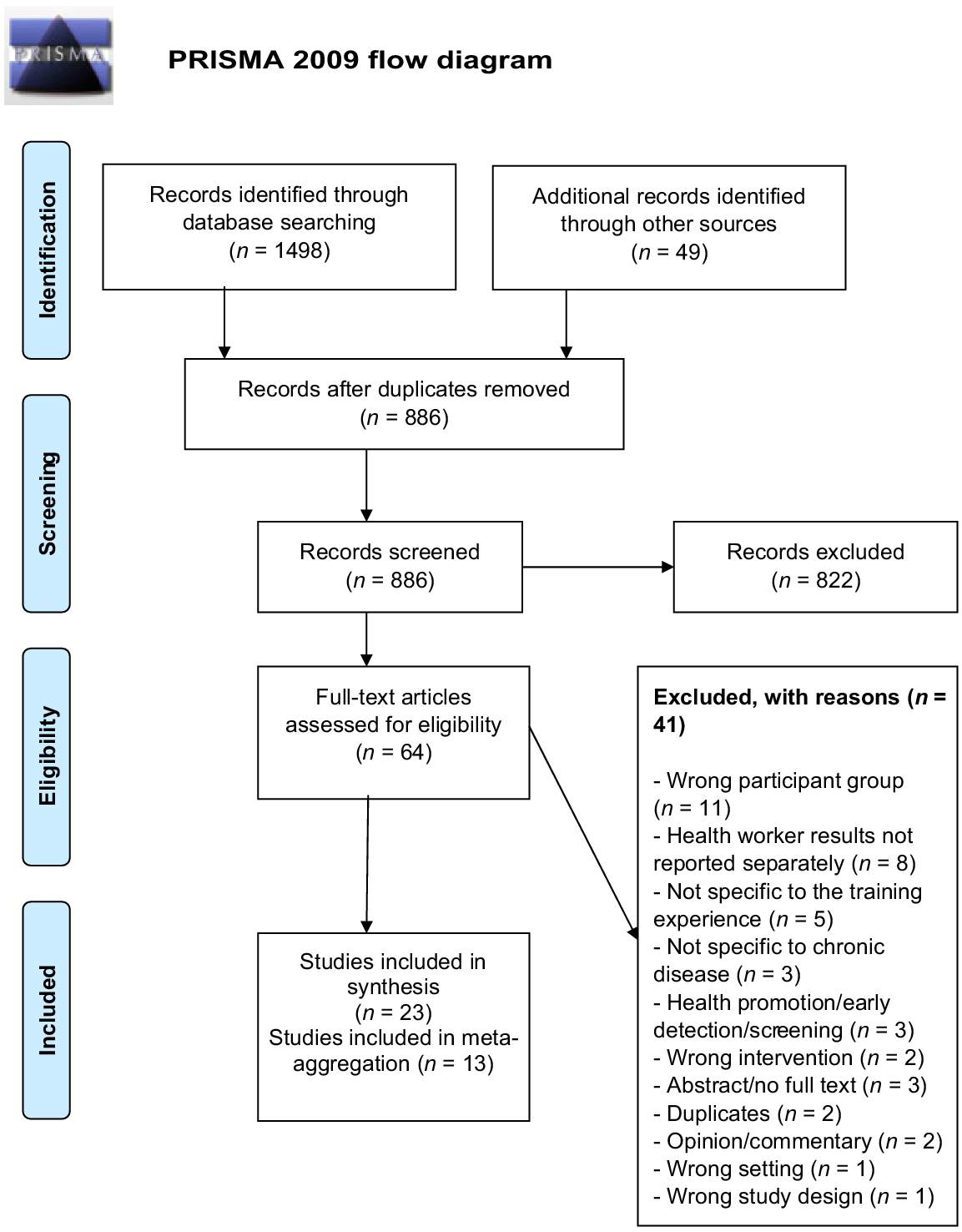
The initial search yielded 1547 references, 661 duplicates were removed, leaving 886 studies to screen against the title and abstract. Of those, 822 studies were irrelevant to the study aim, objectives and research questions. Sixty-four studies were retrieved for full text review, with 41 studies excluded for the following reasons: wrong participant group (n = 11), population includes more than AHW/AHPs (n = 8), not specific to the training experience (n = 5), not specific to chronic disease (n = 3); health promotion/early detection/screening (n = 3), wrong intervention (n = 2), conference abstract or no full text (n = 3), duplicate (n = 2), opinion or commentary (n = 2), wrong setting (n = 1) and wrong study design (n = 1). This left 23 final included studies; of those, 13 studies were included in the qualitative data synthesis (meta-aggregation). Fig. 1 outlines the PRISMA Flow Diagram (Moher et al. 2009).
Risk of bias and quality assessment
Although critical appraisal of included studies is not required for a scoping review (Grant and Booth 2009), information, such as appropriateness of statistical analyses, study design and methods, was extracted to report the methodological quality of the included studies (see Table 2). According to the Joanna Briggs Institute Levels of Evidence, the majority of studies were set at level 2 (pre and post-test design) and level 3 (qualitative design; Munn et al. 2014b).
Authors Year Country | Study design and methods | Chronic condition | Study aim | Sample size and characteristics | Length of training | Length of follow-up post training | Level of evaluationA | Evaluation methods | Effectiveness/outcome | Qualitative data synthesis | |
|---|---|---|---|---|---|---|---|---|---|---|---|
Amos et al. (2002) Australia | Qualitative (education program and satisfaction evaluation) | Eye health | Developing and strengthening the knowledge base of health workers | 8 AHWs | 5-day program | Nil | 1 | Satisfaction survey | The course was found to be relevant and informative. | Yes | |
Mixed methods (a quasi-experimental (pre-post) and focus group) | Diabetes | To determine whether an interactive distance training program was an effective model for training CHWs | 23 CHWs (14 identified as Native American) | Weekly teleconference sessions for 6 months, 2-day training held in 3rd month | 6 months | 2 and 3 | Surveys at baseline and 6 months post (DKT, DAS, DCS), program evaluation, 4 focus groups (1½ h each) | DKT: significant improvement of (increased 12.7% from pre to post-test), using paired t-tests. Participants’ confidence (DCS): significant improvement in both clinical and nonclinical skills (average of 3.65 at baseline to 4.28 in non-clinical and 3.26–4.43 for clinical) to post-test using paired t-test. DAS: participants demonstrated improved attitudes on the seriousness of diabetes (4.1-4.4). There was a significant change in participants confidence in clinical skills after completing the program (3.30–4.40) and (3.62–4.29 for non-clinical skills), using paired t-tests. Focus groups: themes relating to improved self-efficacy, expansion of role, opportunity to learn, organisational support, support and validation, and managing complexity of diabetes. | – | ||
Croager et al. (2010) Australia | Quantitative A quasi-experimental (pre, post and follow-up test) | Cancer | To increase cancer knowledge and awareness of the resources and services available | 35 Aboriginal health staff from rural and remote WA | 4-day program | 6–10 months | 1 and 2 | Confidence, knowledge survey | Impact evaluation indicated that the program is culturally relevant. Of the 29 participants (83% response rate) that completed evaluation at course completion. Nine participants completed follow up. End of course: statistically significant improvements in all the confidence items, improved cancer knowledge in three of the five knowledge items, using paired-sample t-tests. ‘List the three major treatments for cancer’, ‘What are three population cancer screening programs in WA’ and ‘What are the three most common cancers in Aboriginal women’, Follow-up: increased confidence was only sustained for 2 items: ‘I know what cancer is’ (P < 0.05) and ‘I can describe the different common cancers’ (P < 0.05). Increased level of knowledge was not sustained during the follow up | – | |
Mixed methods (pre-post survey, and open-ended questions) | Cancer | To promote cancer awareness and cancer knowledge | 30 in total, incl. 25 Alaska Native Community Health Aides/Practitioners (CHA/Ps) working in primary care | 5-day course | 6 months | 2 and 3 | Two group teleconferences (2 weeks post), viewer log of digital stories, survey (6 months post) | One month post course participants reported showing their stories over 57 times to more than 959 views. Participants gained insight into their own personal experience with cancer. All participants reported that they liked combining digital storytelling with cancer education as a culturally respectful way to support learning and as a health messaging tool. This also increased their knowledge acquisition and understanding. After the course, participants reported that they were feeling very knowledgeable (average scale value (4.2 versus 2.8 before)) undertaking the course. | Yes | ||
Quantitative (education program and post-evaluation survey, open-ended questions and checkbox) | Cancer | Learn how CHWs perceived digital storytelling as part of the ‘Path to Understanding Cancer’ curriculum and as a culturally respectful tool for sharing cancer-related health messages | 67 in total, incl. 38 Alaska Native CHWs working in primary care | 5-day course | 6 months – 3 years | 1, 2 and 3 | End of course written evaluation, (n = 67), Internet survey between 6 months and 3 years post training (n = 24) | All participants completed the course evaluation. Participants reported that digital storytelling supported their learning and increased their cancer knowledge. 84% of participants (56 of 67) described ways they felt differently about cancer, however, 48 completed the course. Up to 3 years post training, only 24 completed the follow up. Participants reported showing their digital story and changing their own behaviour. | Yes | ||
Quantitative (cross-sectional) (education program and post-evaluation survey) | Cancer | To offer webinars on cancer | 11 Alaska Native CHA/Ps working in primary care | 10 webinars (1 h each) | Nil | 1, 2 | Survey after each webinar (11 unique learners completed 41 evaluation surveys) | All learners reported that they intended to change their behaviour to reduce their own cancer risk such as 91% of the learners planned to increase their physical activity. All learners reported that they planned to talk with their patients more often about cancer risk reduction behaviours. Learners reported feeling on average between ‘more’ and ‘much more’ comfortable, confident, prepared, and knowledgeable to talk with patients about cancer. | Yes | ||
Quantitative (cross-sectional) (education modules and post-evaluation survey) | Cancer | To inform CHA/Ps of specific cancer info, to support them to engage in cancer risk reduction behaviours, and to improve their capacity and intent to share info | 79 Alaska Native CHA/Ps working in primary care (out of 379 participants) | 10 standalone cancer education modules (2 h each) | Nil | 1 and 2 | Knowledge based quiz and end of module evaluation survey at the end of each module; total of 459 surveys) | A total of 86% of unique CHA/P learners reported feeling more or much more capable on at least one of these items. Learners reported on about 80% of surveys that they felt more or much more knowledgeable about cancer, or more or much more comfortable, confident, or prepared to talk about cancer with their patients, friends, family, and in their communities. The participants reported that the modules were enjoyable, appreciated and informative. | Yes | ||
Quantitative (cross-sectional) (education modules and post-evaluation survey) | Cancer | To inform CHA/Ps of specific cancer info, to support them to engage in cancer risk reduction behaviours, and to improve their capacity and intent to share info. | 89 Alaska Native CHA/Ps working in primary care | 10 standalone cancer education modules (2 h each) | Nil | 1 and 2 | Survey at the end of each module (total of 428 end of module evaluation surveys were completed by 89 unique Alaska CHA/Ps) | 100% of participants reported that they had learned what they were hoping to learn 97% found the modules were respectful of them and their culture. | Yes | ||
Davidson et al. (2008) Australia | Mixed Methods (pre-post-test and semi-structured interviews) | CVD | To increase cardiovascular knowledge and confidence | (21 total participants): Group 1: 9 AHWs from urban areas Group 2: 12 AHWs from rural areas | Group 1: 1 day/week for 10 weeks Group 2: 2 × 3 – day blocks, 1 month apart | One month after (through an interview) | 1, 2 and 3 | CVD knowledge and confidence surveys pre and post, semi-structured interviews 1 month post | Knowledge: statistically significant increases in pre/post test scores (9.93–17.43 respectively), using Paired t-tests. 28% increase in CVD knowledge scores at the end of the course. Confidence: statistically significant increases in confidence nearly doubled across each of the three domains: (confidence in knowledge, skills and communication) from pre-test 4.46, 4.29, 5.52 and post-test to 8.08, 8.16, 8.34 respectively, for all participants). No significant difference observed for the size of change pre-post-test based on the course delivery schedule. | Yes | |
Quantitative Cross-sectional (education program and post evaluation survey) | Cancer | To present overviews and updates related to cancer, and to address culturally relevant cancer care issues | 131 Native American or Alaska Native community workers from 29 tribal clinics | Monthly topics 1 h each/telehealth | Nil | 1 | Satisfaction survey | Of the 131 providers who participated, 71 returned the survey (54%). Likert scale was used to gather info about the use of telehealth for professional education sessions. Overall satisfaction was high with a mean rating of 3.6 on a 4-point scale. Participants rated their feelings about telehealth pre and post their first session, with scores increasing from 3.0 to 3.48. Open ended feedback indicated that participants found sessions valuable and supported the use of telehealth. | – | ||
Higgins et al. (2012) Australia | Mixed methods (pre-post-test design, and follow up phone interview) | Chronic disease | To improve health professionals’ capacity to support CDSM and deliver a client centred approach | 58 AHWs (total of 321 health professionals) | 1 or 2 days depending on the location | Sub-sample telephone interview 2 months post | 2 and 3 | CDSM self-efficacy scale, intended practice change, anticipated barriers to practice change and self-reported practice change. | Highly significant change in CDSM self- efficacy between pre (M = 48.61, s.d. = 8.63) and post training (M = 54.93, s.d. = 7.72), using analysis of variance (ANOVA). Participants self-reported practice changes after 2 months. No other data sets reported AHW data separately. | Yes | |
Jull et al. (2019) Canada | Qualitative (phase 1 and 2: Integrated knowledge translation approach (using focus groups and interviews) | Cancer | To train and support community support workers (CSWs) to prepare community members for shared decision making with health care providers | 5 Inuit Nunangat CSWs from a variety of clinical care settings | Four learning modules and a booklet to guide conversations with community members. | Nil | 1, 2, 3, 4 | Knowledge, skills through focus groups, face to face meetings, and interviews and written field notes. | The community support workers, and community member volunteers who were patients in the cancer care system found the shared decision-making strategy to be useful and feasible in cancer care. The booklet makes it easy to talk with the patients about what is important. The shared decision making should be used as early as possible in the cancer care journey. | Yes | |
King and Sinn (1999) Australia | Qualitative (interview using Semi-structured questionnaire) | Diabetes | To deliver a specialist diabetes postgraduate training program, to improve access to a specialist diabetes health worker for Aboriginal people | 5 AHWs from across SA attended Flinders University Diabetes Educators course | Four modules, each with 1 week intensive (incl. 40 h of clinical placement) | Follow-up interview several weeks after the completion of the module | 1 | Interview | Participants reported that the course had a positive impact personally and professionally. Networking with the other AHWs was highly valued. The course was enjoyable, relevant and very helpful. Two out of five students completed the course. | Yes | |
King et al. (2007) Australia | Qualitative (interview using semi-structured questionnaire) | Diabetes | To deliver a specialist diabetes postgraduate training program, to improve access to a specialist diabetes health worker for Aboriginal people | 18 AHWs from 14 ACCHOs across metro, rural and remote SA attended Flinders University Graduate Certificate in Health: Diabetes Management and Education | Five modules, each with 1 week intensive (incl. 40 h of clinical placement) | Nil | 1, 2 and 3 | Observation of practice and field work, interviews. | AHWs reported they were more confident and competent, which was confirmed through interviews with supervisors. The majority of the participants believed the course was relevant to the diabetes health care needs of Aboriginal people. AHWs and supervisors provided a number of examples of how AHWs have put knowledge into clinical practice. | Yes | |
Mixed methods (longitudinal design using surveys and focus group) | Diabetes | To build community health representatives (CHRs) and relationships through a monthly training program | 107 CHRs responded to the survey and 53 participated in focus group discussion to provide feedback on monthly training sessions | Monthly training sessions | Nil | 1, 2 and 3, 4 | Retrospective surveys, focus groups | Participants found the training was useful with some reporting changes to their practice with clients. The participants felt strongly that communication and teamwork had improved. They also felt that the referral process was improved. They also reported that patient behaviour had improved this including changes in diet, exercise, medication adherence and provider follow up. | – | ||
Quantitative (-re-post-test design) | Diabetes | To increase CHW knowledge about diabetes and increase capacity of community health organisations | 111 CHWs in Hawaii (comprised of five major islands); 69% were from Native Hawaiian and other Pacific Peoples back grounds Seven cohorts completed the course over 3 years | 4 h over three modules | Nil | 1 and 2 | Pre- and post-Ddiabetes knowledge survey. Satisfaction survey. | All participants agreed that the course provided useful information about diabetes, its risk factors and complications. Overall, statistically significant improvement in mean test scores of 1.92 (P < 0.0001) or a 20.97% increase. Urban (9.06–11.42 pre, post-test) versus Rural (9.57–11.00 for pre-post-test), using paired t tests. Urban classes had greater improvement than rural classes. | – | ||
McRae et al. (2008) Australia | Mixed Methods (pre, immediate and post questionnaires, and follow-up interviews) | CVD | To deliver a medicine education program with focus on cardiovascular disease | 59 AHWs were offered training across 10 sites in western NSW. 80% attended ≥1 session | 4 units (1.5 h each) | Nil | 1 | Learner satisfaction survey. 27 completed all four units. At follow up, a total of 47 AHWs had attended the training units. | All participants found that the information was clear and easy to understand, and they felt that they learnt a lot about the cardiovascular medicines. The presenter was interested in their topics and encouraged them to get involved. AHWs found the program interesting, accessible and relevant. 32 out of 47 (68%) feedback survey were completed by the AHWs. | – | |
Quantitative (pre-post-test design) | CVD | To increase CHW knowledge and increase long-term information competency over 6 months | 46 CHWs in Hawaii (comprised of five major islands); 61% were from Native Hawaiian and other Pacific Peoples backgrounds | 5 h (3 modules over 2 days) | 6 months | 1 and 2 | CVD knowledge test at baseline, post training and after 6 months, Satisfaction survey. | Statistically significant improvement in both short term and long-term knowledge. 1. Pre-seminar score (11.1 ± 3.0), versus the post-seminar score (14.6 ± 2.0), P < 0.0001, using paired t tests. 2. Pre-seminar scores (mean 12.1 ± 2.6 s.d.), versus 6 months post-seminar (14.2 ± 1.2), P < 0.0004, demonstrate long-term information competency. | – | ||
Orr (1993) USA | Mixed methods (pre-post-test design and interview) | Diabetes and vision impairment | To deliver culturally sensitive curriculum on ageing and vision loss, and training in independent living skills | 250 health care providers from 78 tribes across USA (majority CHWs) | 1 week intensive | Two follow-up surveys, and an interview; however, the exact time not stated | 1 and 2, 3, 4 | Pre- and post-training tests (attitudes and beliefs), written curriculum review, interviews, training program evaluation | Qualitative feedback indicated improvements in knowledge/skills, confidence and changes in attitudes towards visually impaired persons. They learnt skills they could teach to visually impaired elders and their family members. Increased their level of awareness about the nature and prevalence of blindness and visual impairment. Curriculum contents was more useful, and they reported feeling more comfortable and confident discussing vision loss with their clients’ family members. The CHRs noted that the independent living skills they taught their blind and visually impaired elderly clients and family members helped them to improve safety in their home environments. This improved the clients’ level of independence and functioning. | – | |
Quantitative (pre-post evaluation design) | Diabetes | To determine if diabetes training could improve CHW knowledge of diabetes and the management of diabetes | 10 CHWs identified by tribal community w/training conducted in a Native American community centre | 24 h (4-h sessions over 6 weeks) | Nil | 1 and 2 | Satisfaction survey, DKT, DAS | Participants reported that the training materials were helpful. Increase in diabetes knowledge pre-score range (range 63.6–90.4 (s.d. 9.1) to post-score range (90.9–100 (s.d. 4.1)), using paired t-tests. Seven participants completed both pre- and post-tests. Pre-test evaluation ranged from 0.39 to 0.91 (standard deviation [s.d.] 0.17) and increased marginally for all participants resulting in a post-test range of 43.4–95.6 (s.d. 0.18) and an upward movement in both the median and the mean. Subtle change in attitudes over the course of the training. | – | ||
Sebastian et al. (2021) Australia | Qualitative (qualitative research design using interview) | Chronic conditions | To explore participants’ perceptions of the characteristics of the B.strong brief intervention training program as enablers and barriers to the program’s uptake at Aboriginal PHC services, and for trainees implementing BIs | 24 participants (AHW/Ps, tertiary qualified health professionals, managers/supervisors) from ATSICCHOs and government operated PHC services in metro, rural and remote Qld. 12 participants (50%) were Aboriginal | 1 day face-to-face workshop (8 h) and six online modules (2 h duration each) | Nil | 1 and 2 | CFIR | Cultural appropriateness of the program, its perceived applicability in the daily work of health staff’ daily work, the trustworthiness and quality of the program, and the availability and accessibility of the training were identified to be important enablers to implementing the program into their clinical practice. | Yes | |
Thorpe and Browne (2009) Australia | Mixed methods (pre-post evaluation survey and interviews) | CVD | To develop and evaluate the efficacy of a model for ongoing professional development of AHWs who have graduated from Certificate course in CVD | 18 AHWs working in ACCHOs in metro and rural Vic. | 6 months of mentoring | Nil | 1 and 2, 3 | Pre- and post-competency self-assessment, qualitative interviews | Mentoring seen to be valuable and enhanced their skills and felt more confident about performing various functions in the workplace, such as health promotion planning and patient education. Average total of the confidence scores increased from 3.4 to 4 after 6 months. | Yes | |
Zeunert et al. (2002) Australia | Mixed methods (Impact evaluation survey and focus group) | Diabetes, kidney disease, CVD | To extend AHW knowledge and skills in transferring nutrition knowledge to community | 4 AHWs from an ACCHO in remote SA | Five modules (6 h each over five visits) | Nil | 1 and 2, 3, 4 | Process (satisfaction) and impact evaluation (knowledge, skills), focus group (satisfaction, knowledge, confidence) | Increased nutrition knowledge and skills. Increased AHW capacity to work with and communicate nutrition messages to community. Numerous individuals reported change in their eating patterns and their lifestyle factors. | – |
Nil, no follow up.
None of the included studies had a comparator.
AHW, Aboriginal health worker; CHWs, Community Health Workers; DKT, Diabetes Knowledge Tool (Policicchio and Dontje 2018); DAS, Michigan Diabetes Research and Training Centre Diabetes Attitude Survey (Policicchio and Dontje 2018); DCS, Diabetes confidence Survey (Colleran et al. 2012); CVD, cardiovascular disease; CDSM, chronic disease self-management; ACCHO, Aboriginal Community Controlled Health Organisation (ACCHO); CFIR, Consolidated Framework for Implementation Research (Sebastian et al. 2021).
Study characteristics
Nine quantitative (Look et al. 2008; Croager et al. 2010; Doorenbos et al. 2011; Cueva et al. 2013, 2018a, 2018b, 2019; Moleta et al. 2017; Policicchio and Dontje 2018), four qualitative (King and Sinn 1999; Amos et al. 2002; King et al. 2007; Sebastian et al. 2021) and nine mixed methods studies (Orr 1993; Zeunert et al. 2002; Davidson et al. 2008; McRae et al. 2008; Thorpe and Browne 2009; Colleran et al. 2012; Higgins et al. 2012; Cueva et al. 2016; King et al. 2017; Jull et al. 2019) were included in the review. Twelve studies used a quasi-experimental design through conducting pre-, immediate and post-evaluation questionnaires; four studies used a cross-sectional survey as an evaluation following the education program (Doorenbos et al. 2011; Cueva et al. 2018a, 2018b, 2019). Four studies used a qualitative descriptive design, with either focus groups, interviews or semi-structured interviews as the data collection method (see Table 2).
Twelve studies were conducted in the USA (Orr 1993; Look et al. 2008; Doorenbos et al. 2011; Colleran et al. 2012; Cueva et al. 2013, 2016, 2018a, 2018b, 2019; King et al. 2017; Moleta et al. 2017; Policicchio and Dontje 2018), 10 studies in Australia (King and Sinn 1999; Amos et al. 2002; Zeunert et al. 2002; King et al. 2007; Davidson et al. 2008; McRae et al. 2008; Thorpe and Browne 2009; Croager et al. 2010; Higgins et al. 2012; Sebastian et al. 2021), and one in Canada (Jull et al. 2019).
Two studies were published in the 1990s (Orr 1993; King and Sinn 1999); seven in the 2000s (Amos et al. 2002; Zeunert et al. 2002; King et al. 2007; Davidson et al. 2008; Look et al. 2008; McRae et al. 2008; Thorpe and Browne 2009); and 14 from the 2010s and onwards. Studies were conducted in urban, rural or remote primary care settings.
The included studies focused on managing common chronic diseases, such as diabetes, cancer, cardiovascular or more than one chronic disease. Seven studies focused on diabetes only (Orr 1993; King and Sinn 1999; King et al. 2007; Look et al. 2008; Colleran et al. 2012; Cueva et al. 2018a; Policicchio and Dontje 2018); eight studies provided cancer education training programs (Croager et al. 2010; Doorenbos et al. 2011; Cueva et al. 2013, 2016, 2018a, 2018b, 2019; Jull et al. 2019); four studies explored cardiovascular disease (Davidson et al. 2008; McRae et al. 2008; Thorpe and Browne 2009; Moleta et al. 2017); three studies covered several chronic conditions, such as diabetes, kidney disease and cardiovascular disease (Zeunert et al. 2002; Higgins et al. 2012; Sebastian et al. 2021); and one study focused on eye health (Amos et al. 2002).
Participants’ characteristics
Participants who received the training were AHW/AHPs, Community Health Workers or Community Health Practitioners (CHPs) working across metropolitan, rural or remote areas. The sample size was small for the qualitative studies (5–24 participants), whereas the quantitative studies ranged between 10 and 131 participants. For mixed methods studies, the sample size was in the range of 4–250 participants, with an overall total of 1120 participants across different study types.
Participants follow up and retention
Only nine studies followed up participants post the training. Follow up ranged from 1 month (Davidson et al. 2008) to 3 years (Cueva et al. 2013), with an average of 6 months for five included studies (Croager et al. 2010; Colleran et al. 2012; Cueva et al. 2013, 2016; Moleta et al. 2017). Only three studies reported a dropout rate that was between 40% and 70% during the follow-up period of the training program (King and Sinn 1999; Doorenbos et al. 2011; Policicchio and Dontje 2018; Table 2).
Evaluation methods
All 23 studies used evaluation tools to assess their training program. Variation in study objectives meant diverse measurement tools were used across included studies. Ten studies used a satisfaction survey and/or program evaluation questionnaire on completion of the training program (Amos et al. 2002; Zeunert et al. 2002; Look et al. 2008; McRae et al. 2008; Doorenbos et al. 2011; Cueva et al. 2013, 2018a, 2018b, 2019; Policicchio and Dontje 2018). Similarly, 10 studies used validated questionnaires as pre- and post-test survey to measure the participants’ knowledge, skills and confidence, such as the Diabetes Knowledge Tool (DKT), Diabetes Attitude Survey (DAS), Diabetes Confidence Survey (DCS) and Brief Intervention (BI) to measure knowledge and confidence or skills and attitude of the participants at baseline and follow up (Orr 1993; Zeunert et al. 2002; Davidson et al. 2008; Look et al. 2008; Thorpe and Browne 2009; Croager et al. 2010; Colleran et al. 2012; Moleta et al. 2017; Policicchio and Dontje 2018; Jull et al. 2019). Only five studies used questionnaires to measure change in attitude and behaviour or participant intention to use the learned knowledge in practice (King et al. 2007; Colleran et al. 2012; Higgins et al. 2012; Cueva et al. 2013; King et al. 2017). Some studies used multiple methods of evaluation of their training program (Table 2).
Characteristics of the training programs
Similar characteristics were found among training programs: development/design, preparation and facilitation; components; and mode of delivery. A majority of the training programs (n = 16, 70%) were developed in collaboration with stakeholders, although only a few of the studies reported that participants and managers underwent formal preparation for the training. The majority of the included studies had facilitators of the same profession and/or clinical experts in the field, with nearly 35% (n = 8) of the studies reporting that training included components delivered by cultural facilitators. Every training program included time spent on providing content knowledge (curricular knowledge) to participants. Content on the topic was available to participants in written, verbal and practical formats. Of the 23 training programs, two studies included a professional support network (Colleran et al. 2012; Cueva et al. 2018b), four studies provided on-the-job support (King et al. 2007; Davidson et al. 2008; Colleran et al. 2012; King et al. 2017) and six studies had follow-up support post the training program (Orr 1993; Zeunert et al. 2002; Davidson et al. 2008; Thorpe and Browne 2009; Colleran et al. 2012; Higgins et al. 2012; Table 3). In terms of mode of delivery, the majority of studies included interactive methods, including instructor-led classroom; hands-on learning, such as role play, simulation and skills development; and lectures (Table 3).
| Training development, preparation and facilitation | Training components | Mode of delivery | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Authors/year/study design | Training collaboratively developed with stakeholders | Participants prepared for training | Managers prepared for training | Facilitation | Training included cultural facilitator | Content | Onsite support during training | Post training clinical support/learning | Instructor-led classroom (interactive) | Hands-on learning (role play, simulation, skill development) | Lecture based | Online learning (synchronous) | Online learning asynchronous) | Reported improvement? | |
| Amos et al. (2002) Qualitative | ✓ | NR | ✓ | Ophthalmic nurse | X | Clinical placement, demonstrations | X | X | ✓ | ✓ | X | X | X | NR | |
| Colleran et al. (2012) Mixed methods | NR | NR | NR | NR | NR | PPT, case studies, syllabus, Q and A, demonstrations | ✓ | ✓ Weekly telecon for 6 months | ✓ | ✓ | ✓ | ✓ Weekly teleconference | X | ✓ | |
| Croager et al. (2010) Quantitative | ✓ | NR | NR | Clinical experts | ✓ | Presentations, clinical visits, experiential, yarning | X | X | ✓ | ✓ | ✓ | X | X | ✓ | |
| Cueva et al. (2016) Mixed methods | NR | NR | NR | NR | NR | Digital story, course manual | X | X | ✓ | X | X | X | X | ✓ | |
| Cueva et al. (2013) Quantitative | NR | NR | NR | RN and guests | ✓ | Course manual, digital story | X | X | ✓ | X | X | X | X | ✓ | |
| Cueva et al. (2019) Quantitative | ✓ | NR | NR | NR | ✓ | Storytelling, conversational | X | X | ✓ | NA | X | ✓ | X | ✓ | |
| Cueva et al. (2018a) Quantitative | ✓ | NR | NR | NA (online) | NA | Online knowledge quizzes, storytelling | X | X | NA | NA | NA | X | ✓ | ✓ | |
| Cueva et al. (2018b) Quantitative | ✓ | NR | NR | NA (online) | NA | Visuals, storytelling, interactivity, cultural teachings, and respect for diverse Alaska Native learners’ cultures | X | X | NA | NA | NR | X | ✓ | ✓ | |
| Davidson et al. (2008) Mixed methods | ✓ | NR | NR | Clinical and local experts | ✓ | AHW heart health manual, assessment criteria, worksheets, resources, action learning, hospital site visits (experiential learning), clinical practice observation | Participants encouraged to choose workplace mentor; no info as to how and if this occurred | ✓ Participants encouraged to choose workplace mentor; no info as to how and if this occurred | ✓ | ✓ | X | X | X | ✓ | |
| Doorenbos et al. (2011) Quantitative | NR | NR | NR | Clinical experts | X | Lecture | X | X | X | X | X | ✓ Telehealth | X | NR | |
| Higgins et al. (2012) Mixed Methods | NR | NR | NR | NR | NR | Workbook | NA | ✓ Practical tools to support clinical practice | ✓ | ✓ | X | X | X | ✓ | |
| Jull et al. (2019) Qualitative | ✓ | NR | NR | NR | NR | Booklets in Inuit and English languages | X | NR | ✓ | ✓ Field test w/community member volunteers | X | X | X | ✓ | |
| King and Sinn (1999) Qualitative | NR | NR | NR | Experts | X | NR | X | X | ✓ | ✓ | ✓ | X | X | NR | |
| King et al. (2007) Qualitative | ✓ Adjustments made from AHW feedback 1999 paper above | ✓ | NR | Experts | X | Glossary of medical terminology. Culturally relevant | ✓ Two project officers worked as mentors (details not provided) | X | ✓ | ✓ | ✓ | X | X | ✓ | |
| King et al. (2017) Mixed methods | ✓ Feedback from clinicians | NR | NR | Local providers | NR | Teaching materials, competency assessment, learning objectives | ✓ | X | NR | NR | NR | NR | NR | ✓ | |
| Look et al. (2008) Quantitative | ✓ | NR | NR | Clinician and senior CHW | ✓ | Workbook, cultural material, presentations, case studies, role plays, group learning exercises | X | X | ✓ Small class size | ✓ | X | X | X | ✓ | |
| McRae et al. (2008) Mixed Methods | ✓ | X | ✓ | Local community pharmacist | X | CDROM, workbooks, boardgames, presentation | NA | X | ✓ | NR | ✓ | X | ✓ CD-ROM | NR | |
| Moleta et al. (2017) Quantitative | ✓ | NR | NR | Clinician and senior CHW | ✓ | Workbook, presentations, case studies, role plays, knowledge games, stories, glossary, skits | X | X | ✓ | ✓ | ✓ | X | X | ✓ | |
| Orr (1993) Mixed methods | ✓ | NR | NR | Local experts | X | Lecture, group discussion, role play, clinical and client resources, acive hands-on and paired learning, simulation | ✓ Client resources | ✓ A week-long training course for CHRs representing six tribes in Oklahoma | ✓ | ✓ | ✓ | X | X | ✓ | |
| Policicchio and Dontje (2018) Quantitative | ✓ | ✓ | NR | Public health nurse w/guest presenters from the tribe | NR | Handouts (resources), website, course summary, flip charts, role play, games, art, group discussion | X | X | ✓ | ✓ | ✓ | X | X | ✓ | |
| Sebastian et al. (2021) Qualitative | ✓ | ✓ | ✓ | Two Aboriginal trainers | ✓ | Participant handbooks, practitioner, guides and tools, client, resources (brochurs) | X | X | ✓ | X | X | X | ✓ | NR | |
| Thorpe and Browne (2009) Mixed Methods | X | ✓ | ✓ | NA | ✓ | Training CD, mentoring workbook, one reflective teleconference, mentoring | ✓ | ✓ | NA | NA | NA | NA | NA | ✓ | |
| Zeunert et al. (2002) Mixed methods | ✓ | NR | NR | Nutritionists | X | Training manual, label reading activity, board game, case studies | X | ✓ | ✓ | ✓ | X | X | X | ✓ | |
✓, Yes; X, No; NR, not reported; NA, not applicable.
Length of training and mode of delivery
The frequency and duration of the training sessions varied and ranged from 1 day to 6 months. Two studies provided online training through 10 webinars, each lasting for an hour (Doorenbos et al. 2011; Cueva et al. 2019). Two studies used a blended learning approach of face-to-face and online training for the participants. Sebastian et al. (2021) delivered a 1-day (8 h) face-to-face workshop and six online modules, each lasting 2 h. Similarly, Colleran et al. (2012) provided weekly teleconference sessions over 6 months with two training days halfway through. The remaining studies provided training through face-to-face workshops as a traditional mode of delivery (Table 2).
Some training programs were provided for one or 2 days (Higgins et al. 2012; Moleta et al. 2017) to a week of intensive training (Orr 1993). Four studies provided the training over 4–5 days (Amos et al. 2002; Croager et al. 2010; Cueva et al. 2013, 2016). Training was longer in four studies − 6 weeks (Policicchio and Dontje 2018), 10 weeks (Davidson et al. 2008) and 6 months (Thorpe and Browne 2009; Colleran et al. 2012; Table 2).
In terms of the training materials and curriculum development, studies reported that the training curriculum ranged from three modules (Look et al. 2008; Moleta et al. 2017) to 10 modules that lasted for 2 h each (Cueva et al. 2018a, 2018b). An average of four to five modules were reported in five studies (King and Sinn 1999; Zeunert et al. 2002; King et al. 2007; McRae et al. 2008; Jull et al. 2019; Table 2).
Outcomes of the training programs
Participants in the majority of studies reported that the course/module was informative, relevant and enjoyable (Orr 1993; King and Sinn 1999; Amos et al. 2002; Zeunert et al. 2002; King et al. 2007; Davidson et al. 2008; Look et al. 2008; McRae et al. 2008; Thorpe and Browne 2009; Cueva et al. 2013, 2018a, 2019; King et al. 2017; Moleta et al. 2017; Policicchio and Dontje 2018; Jull et al. 2019; Sebastian et al. 2021). In two studies, the training was felt to be respectful to the participants and relevant to their culture (Croager et al. 2010; Cueva et al. 2018b). In one study each, the training program positively impacted the participants personally and professionally (King and Sinn 1999), and the sessions supported the use of telehealth (Doorenbos et al. 2011; Table 2).
There was variation in the measures evaluated across studies. Studies reported one or more measures relating to participants’ knowledge, confidence, skills and attitude. Participants across several studies reported that they felt more knowledgeable, confident and comfortable talking with clients, and/or friends, family and communities about cancer (Cueva et al. 2016, 2018a, 2018b, 2019) or other chronic conditions (Policicchio and Dontje 2018; Sebastian et al. 2021). Participants also reported an increase in their nutrition knowledge, and skills and capacity to work with and communicate nutrition messages to the community (Zeunert et al. 2002). Moreover, using digital storytelling increased their knowledge about cancer (Cueva et al. 2013). In addition, using a booklet made it easier to talk with the clients about what is important (Jull et al. 2019; Table 2).
Several studies reported a statistically significant improvement in participants’ knowledge and confidence after the training (Davidson et al. 2008; Croager et al. 2010). Colleran et al. (2012) reported a significant improvement (t = 4.24, P < 0.001, effect size 0.93) in participants’ knowledge, with a 12.7% increase from pre- to post-training, and a significant increase in participants’ confidence in both clinical and non-clinical skills (Table 2).
Two studies reported a statistically significant improvement in participants’ knowledge after the training (mean 14.6 ± 2.0 s.d.; range 90.9–100, 4.1 s.d.) compared with pre-training (mean 11.1 ± 3.0 s.d.; (range 63.6–90.4, 9.1 s.d.), respectively, both used paired t-tests (Moleta et al. 2017; Policicchio and Dontje 2018). Look et al. (2008) reported a statistically significant improvement in participants’ knowledge, with a 20.97% increase. Two studies reported an improvement in participants’ confidence after the training (King et al. 2007; Thorpe and Browne 2009), and one study reported improvements in participants’ knowledge, skills, confidence and change in attitudes towards visually impaired persons; however, the data were not reported (Orr 1993; Table 2).
Common characteristics of these training program across all included studies were collaborative development of the training program with stakeholders (n = 16), having an expert in the field or of the same profession delivering the training (n = 14) and the training included cultural facilitators (n = 8). In terms of mode of delivery, these studies were interactive through an instructor-led approach (n = 18), and they provided hands-on learning through role play, simulation and skills development (n = 13).
Eleven studies from qualitative and quantitative designs reported participants’ feedback relating to behaviour change, transfer of learned knowledge to community members (Zeunert et al. 2002; King et al. 2007) and use in clinical practice (Orr 1993; Davidson et al. 2008; Thorpe and Browne 2009; Higgins et al. 2012; Cueva et al. 2013, 2016; Jull et al. 2019), and improvements in practice with clients, communication skills and teamwork (King et al. 2017). Furthermore, participants reported significant change in their confidence in clinical skills after completing the training program (Colleran et al. 2012; Table 2). Common characteristics of these training programs were collaborative development of the training program with stakeholders (n = 6), and having an expert in the field or of the same profession delivering the training (n = 6). In terms of mode of delivery, these studies were interactive through an instructor-led approach (n = 9), and they provided hands-on learning through role play, simulation and skills development (n = 7; Table 3).
At follow up, only three studies reported sustained knowledge and confidence. Moleta et al. (2017) reported sustained knowledge at 6 months following the training (pre- 12.1 ± 2.6 vs post- 14.2 ± 1.2, P < 0.0004) using paired t-tests, whereas Croager et al. (2010) reported sustained confidence. Participants who used digital storytelling during their clinical practice reported behaviour change after 3 years of follow up (Cueva et al. 2013; Table 2). These three studies have similarities in which the training programs were delivered by a clinical expert in the field (n = 3) and a cultural facilitator (n = 3), they were also interactive through using an instructor-led training approach (n = 3; Table 3).
None of the included studies used measurement tools to assess clients’ outcomes, although several studies reported an improvement in clients’ outcomes based on interviews with the health care workers. These studies reported that patient behaviour had improved, including changes in diet, exercise, medication adherence and provider follow up (Zeunert et al. 2002; King et al. 2017; Jull et al. 2019) or improved level of independence and functioning for elderly clients who were blind or had visual impairment (Orr 1993; Table 2). Common characteristics of these training programs were the training content developed with the stakeholders (n = 3) and the training program delivered by an expert in the field (n = 2; Table 3).
Based on the Kirkpatrick Model of evaluating effectiveness of training programs, most studies only utilised level 1 (reaction of the participants to the training program) and 2 (learning including attitude, knowledge and confidence), by which they administered a feedback evaluation survey to measure participant experiences and satisfaction post-training, and participant knowledge, confidence and skills. Seven studies were designed to meet level three of the Kirkpatrick Model, which focused on behaviour change and intention to use the knowledge that the participants’ received in their clinical practice (King et al. 2007; Davidson et al. 2008; Colleran et al. 2012; Higgins et al. 2012; Cueva et al. 2013, 2016; King et al. 2017). Four studies (Orr 1993; Zeunert et al. 2002; King et al. 2017; Jull et al. 2019) reported improved client-related outcomes as defined by level 4 according to the Kirkpatrick Model; however, none of these studies used measurement tools to assess the improvement.
In addition to the level of evaluation of the training programs, insights are gleaned from commonalities across training programs that achieved a similar significant outcome of improving knowledge, attitude, confidence and skills of AHW/AHPs, as well as client-related outcomes. Across all of the four levels of outcomes described above, the common characteristics were: training content developed collaboratively with the stakeholders (n = 3); facilitation from the same profession or clinical expert from the field (n = 4); training included a cultural facilitator (n = 2); inclusion of cultural content (n = 6); hands-on learning (e.g. role play, simulation, skill development) (n = 4); and interactive learning approaches using instructor-led training (n = 6).
Enablers and barriers (summary of qualitative findings)
Thirteen studies explored the experiences of Aboriginal health care workers participating in chronic disease training programs. These were: five qualitative studies (King and Sinn 1999; Amos et al. 2002; King et al. 2007; Jull et al. 2019; Sebastian et al. 2021), four quantitative studies with open-ended questions (Cueva et al. 2013, 2018a, 2018b, 2019) and four mixed methods studies (Davidson et al. 2008; Thorpe and Browne 2009; Higgins et al. 2012; Cueva et al. 2016).
A total of 62 findings and their illustrations were extracted and included in meta-aggregation. Of these, 48 were unequivocal, and 14 were credible. These findings were grouped into 14 categories, and meta-aggregated into six synthesised findings. Four of the six synthesised findings related to training program attributes: (1) relevance of the training program, (2) modes of learning, (3) power of support and networking, and (4) adult learning capabilities. The remaining two synthesised findings related to outcomes of the training programs: (1) improved knowledge, confidence and skills, and (2) knowledge transfer (for full details see Supplementary Appendix 2: Synthesised findings table).
Synthesised finding 1: Relevance of the training program formed by two categories: (1) participant perceptions of the training program, and (2) cultural safety. It comprises seven unequivocal and five credible findings.
A training program needs to meet the knowledge and practice gaps of participants, and be delivered at the educational level and experience of participants. Continued engagement of participants is supported by content or information sessions that are integrated with activities that develop skills and practice, rather than the two focusing on separate topics or being disconnected. Training content and skills development must facilitate high levels of engagement, be clearly transferable to the practice setting and community context, within the professional scope of practice, and resonate with personal or family health experiences. Program attribute priorities are cultural considerations of including Aboriginal and Torres Strait Islander peoples health professionals as facilitators and creating a learning environment that is culturally safe.
Synthesised finding 2: Modes of learning formed by three categories: (1) use of technology to facilitate training, (2) storytelling for client education, and (3) digital storytelling. It comprises one credible and eight unequivocal findings.
Opportunities to share work experiences with peers through regular networking is valuable and can be delivered online. The regularity of networking opportunities is an important consideration, along with having activities that facilitate interactionm such as reflective practice. Storytelling is a powerful training tool in giving participants a voice in the training about their experiences that may otherwise have gone unspoken. Furthermore, digital storytelling can be done in way that is culturally respectful and effective as a means for participants to provide health messages to their clients.
Synthesised finding 3: Power of support and networking formed by two categories: (1) peer support, and (2) professional networking. It comprises five unequivocal and two credible findings.
A key factor in a successful partnership is developing good relationships and rapport. Important components of the learning experience are getting together through the training program and having the support of Aboriginal and Torres Strait Islander peoples colleagues in the program. Furthermore, contacting the project coordinators at any time for additional support is greatly appreciated, and is an essential part of successful partnerships. However, further training opportunities can be made available; for example, refresher courses or training in specific areas, such as nutrition, computer skills and medications, and discussing recent research findings. Additional networking can be required to share work experiences related to related topics; for example, health promotion projects.
Synthesised finding 4: Adult learning formed by two categories: (1) pros and cons of higher learning, and (2) work–family commitments. It comprises nine unequivocal and two credible findings.
Positive experiences of training programs can include personal satisfaction on completion, additional ability to empower Aboriginal clients to practice selfcare and becoming specialised in particular health condition/s. However, transition to adult learning may be challenging, as some individuals may have previous negative educational experiences that impacted their learning. Adult learning was developed from two categories, including the pros and cons of higher learning and work–family commitments. They comprised nine unequivocal and two credible findings. Using medical terminology within the training program and academic writing can create difficulties for participants. Lack of support from managers to participate in mentoring activities, time constraints and family commitments are also barriers to participation in training programs. Various barriers to adult learning can be mitigated with more orientation and lead in time required to assist with adaptation to undertaking the course. Lack of support from managers to participate in mentoring activities, time constraints and family commitments were also barriers to participation in the training program.
Synthesised finding 1: Improved knowledge, confidence and skills formed by three categories: (1) improved knowledge and understanding of chronic diseases, (2) improved health care provider confidence, and (3) practice (clinical and non-clinical skills). It comprises 11 unequivocal and four credible findings.
Increased knowledge and understanding of the relevant health care condition/s can lead to more responsibility to use expertise to care for clients. Training participants seek understanding about the complexity of chronic conditions and adopting a holistic approach to managing the condition; for example, within the context of living circumstances and other social determinants of health. Gaining more information can shift participant feelings about chronic conditions, as the individuals will be able to discuss the acquired information with their clients. The training program content and format are important to empower changing participants; behaviour and share information with others, such as patients, families and communities. Developing more confidence and competence in clinical practice can be a benefit of training. Increased confidence helps to provide education or brief intervention, and these learning skills could be transferred into the workplace by providing more accurate information to clients. In addition, learning using communication skills, such as reflective listening and motivational interviewing, and demonstrated ability in using management skills in clinical practice.
Synthesised finding 2: Knowledge transfer formed by two categories: (1) sharing knowledge with clients and community, and (2) client capacity building. It comprises six unequivocal and three credible findings.
Receiving training can strengthen patient care practices, such as discussing related risk reduction behaviours and undertaking screening examinations. Sharing and disseminating information with families, friends and community members who had chronic diseases are highly valued aspects of a training program, as well as using strengths-based approaches and shared decision-making strategies. Providing methods of communication between patients, health care providers and other clinicians can be valued and utilised in practice by participants.
Integration of quantitative and qualitative evidence
Some quantitative and qualitative findings in this review have been largely complementary and support each other, especially participants’ perception of the training program, knowledge, confidence and skills of the Aboriginal and Torres Strait Islander peoples health professionals, and client-related outcomes.
Quantitative findings provided evidence that participants were satisfied with the training program. The training program content was informative, enjoyable, relevant and respectful to their culture. This was also supported by the qualitative findings, which explored in detail the participants’ views and their satisfaction with the training program, and their experiences after receiving the training program.
Quantitative findings showed that participants reported improved knowledge, confidence, and developed clinical and non-clinical skills in their workplace. This was supported by qualitative findings through reported improved knowledge and understanding of chronic diseases, improved participants’ confidence, and participants were able to transfer their knowledge and skills into clinical practice. Participants also claimed to have developed more clinical and non-clinical skills in their workplace. Participants reported developing increased competence because of the training program, and more confidence in using communication and management skills in clinical practice, and sharing knowledge with families, friends and community.
Few quantitative studies reported an impact of the training programs on clients’ outcomes. Health care providers reported improvement in clients’ outcomes and improved behaviours, such as medication compliance and attending follow-up appointments. Similarly, qualitative studies highlighted the importance of sharing and transferring knowledge into clinical practice with their clients. For example, using different approaches to support clients in clinical practice, such as shared decision-making and a strengths-based approach.
In summary, quantitative and qualitative findings highlighted that a multifaceted training program delivered to Indigenous Health Workers and Practitioners (IHW/P) might be associated with improved knowledge, confidence, and clinical and non-clinical skills, as well as sharing knowledge with family, friends and community. These training programs also had a positive impact on improving client-related outcomes, including improved behaviours, such as medication compliance, diet and exercise. In addition, the training programs enabled health workers and practitioners to use a strenghts-based approach with their clients that focuses on clients’ perspectives, experience and knowledge to enable decision making.
Discussion
This scoping review summarised literature on the characteristics of chronic disease training programs and modes of learning for IHW/P. It synthesised enablers and barriers of modes of delivery, and the outcomes of the training programs on participant knowledge, attitude, skill and practice. The included studies varied in type of chronic disease, sample size, length of training, outcomes measures and effectiveness of the training programs. With regard to evaluation, most studies focused on participants’ satisfaction with content and relevance of training programs. Some studies measured improvement in participant knowledge, confidence, attitude, behaviours and skills, including clinical and non-clinical skills translation into practice (Davidson et al. 2008; Colleran et al. 2012; Cueva et al. 2013, 2016). Few studies provided information on client-related outcomes, but did not measure these (Orr 1993; Zeunert et al. 2002; King et al. 2017; Jull et al. 2019).
The importance of adhering to a framework of strategies to guide practice in Aboriginal health is acknowledged. This framework that would apply to workforce training programs includes: using appropriate approaches (e.g. demonstrating a commitment to building relationships, humility and honesty); skills (e.g. communication, persistence); and personal attributes (e.g. relinquishing control, awareness of Aboriginal history) (Wilson et al. 2020). Similarly, the current findings of this review emphasise that training programs need to be multifaceted, have relevance to local contexts, address barriers to participation and promote engagement with health care providers. Such programs are more likely to result in adopting best practice and improved client-related outcomes (Pantoja et al. 2017). A multifaceted knowledge transfer strategy can have positive impacts by considering factors that may influence uptake and implementation of best practice, including, but not limited to, participants’ knowledge, skills, attitudes, personal beliefs and social contexts. Such a strategy may utilise a combination of educational meetings, training programs of health care providers, educational outreach, practice facilitation, local health leader and peer support, and audit and feedback (Pantoja et al. 2017). These elements, individually and collectively, form building blocks of knowledge transfer and evidence implementation strategies, and have been rigorously evaluated. Furthermore, culturally and contextually informed training programs increases knowledge transfer and translation into practice, which improves client-related outcomes (Curtis et al. 2017).
An emphasis when working with AHW/P is cultural appropriateness and safety, which incorporates knowledge and respect for self and knowledge, and respect for Aboriginal and Torres Strait Islander peoples (Phillips 2017). However, little evidence supports how cultural safety approaches are incorporated into clinical practice (West et al. 2021). In response to ineffective Aboriginal and Torres Strait Islander peoples cultural training programs in Australia, the study highlighted the importance of using cultural safety tools to measure the effectiveness of cultural safety education for Aboriginal and Torres Strait Islander peoples in university and health service settings (West et al. 2021). Our review found that all studies reported training program content that was informative, relevant, respectful to the participants’ culture and incorporated a cultural safety approach. These programs included Aboriginal and Torres Strait Islander peoples history and Aboriginal and Torres Strait Islander peoples culture, and showed respectful interaction with participants, similar findings were reported by Wilson et al. (2020). Culturally appropriate training programs provide a safe space for participants to learn, and ideally adopt care practices that better meet client needs and impact client-related outcomes (Curtis et al. 2017).
Most of the included studies reported that communication skills and respectful interpersonal skills are crucial when working with Aboriginal and Torres Strait Islander peoples communities and individuals (Wilson et al. 2020). Interpersonal skills include being truthful and responsive, having a genuine interest in people and in establishing relationships, honesty and trustworthiness (Dudgeon and Ugle 2014). Communication protocols and guidelines are available on ethical and effective communication for researchers when working with Aboriginal and Torres Strait Islander peoples (Jones and Barnett 2006).
Studies that have evaluated the effectiveness of conducting research through incorporating Aboriginal and Torres Strait Islander peoples research knowledge and methodologies when working with Aboriginal and Torres Strait Islander peoples (Ryder et al. 2020) also highlighted the importance of using storytelling as a recommended data collection method (Ryder et al. 2020; Smith et al. 2020). Storytelling has been recognised as a method for data collection, and a pedagogical tool for learning about life, witnessing and remembering, and sharing stories as a source of strength, and a way of sharing knowledge and validating experiences (Iseke 2013). Storytelling and digital storytelling are used to enforce shared intergenerational and cultural bonding processes among youth, adults, elders and the community, and developing trust, empathy and self-understanding (Bainbridge et al. 2021). It also creates a space for respectful conversations supporting the voices of participants (Bernardes et al. 2020). This review highlighted the importance of storytelling in clinical practice as a powerful tool to involve clients, share knowledge and validate experiences.
As Aboriginal and Torres Strait Islander peoples evaluation framework for IHW/P training in chronic disease management was not found (has not yet been developed), evaluating effectiveness of training programs in this review was based on the New World Kirkpatrick Model (Kirkpatrick and Kirkpatrick 2016). Most included studies focused on level 1 (reaction) and 2 (learning) outcomes measured by participant satisfaction with training program content, delivery and relevance. Following all training programs, participants reported improved knowledge, confidence, attitude, and behaviour related to both clinical and non-clinical skills. This included confidence and skills to deliver education, and provide support and guidance to their clients Few studies were focused on level 3 (behaviour) and 4 (client results) outcomes. Similarly, another study reported increased client engagement with health services by attending follow-up appointments regularly and increased access to chronic disease care due to adequate training programs for IHW/P. To generate robust evidence training, programs need to focus on level 3- and 4-related outcomes. Importantly, Aboriginal and Torres Strait Islander peoples-developed, formal ways of evaluating the impact of programs are needed, so that effectiveness on knowledge, behaviour, confidence in clinical and non-clinical practice, and client-related outcomes may be accurately measured.
This review highlighted the need for IHW/P to receive annual continuous professional development to ensure relevancy related to best practice care, technology and medications, for example, and importantly, a space to share cultural and contextual knowledge and experiences with one another. This ongoing professional development effectively builds health professionals’ confidence, helps translate knowledge into clinical practice and supports the provision of respectful care to Aboriginal and Torres Strait Islander peoples clients (Durey et al. 2017). These findings were consistent with previous literature, which suggests that enhancing continuous education opportunities for IHW/P may positively impact the health of regional Aboriginal and Torres Strait Islander people communities (Martyn and Woolcock 2020). This review also identified the importance of networking through sharing knowledge and supporting each other during training programs. Overall, this review included diverse training programs with various characteristics, which makes it difficult to ascertain their effectiveness.
Strengths and limitations
A strength of this review is that it has informed the design, implementation and evaluation of a diabetes training program for Aboriginal health workers and practitioners. However, due to methodological variability and lack of rigour in study design, evaluation and reporting strong recommendations were not able to be elicited. Generalisability of the findings was limited due to the inclusion of studies from multiple countries, in addition to some studies having small non-representative samples. The inclusion of different chronic diseases could have had a direct effect on the measured outcomes, and included studies varied in follow-up duration. Although few studies reported on client-related outcomes, none of these used formal measurement tools. Identifying these limitations are important for future studies to consider, so that the body of evidence on training programs can become more rigorous.
Conclusion
Multifaceted training programs for IHW/P were well received, and may strengthen and improve the effectiveness of the workforce in managing diabetes. Incorporating Aboriginal and Torres Strait Islander peoples pedagogies in training programs, and having the workforce inform the design, delivery and evaluation of training programs are key to better workforce and client outcomes. Conclusive robust evidence on the effectiveness of training programs is limited due to heterogeneity in the literature, as well as methodological quality. Therefore, future research must be rigorous, and include appropriate and validated tools that measure effectiveness across all outcomes.
Data availability
Data sharing is not applicable as no new data were generated or analysed during this study.
Declaration of funding
This research was funded by Medical Research Future Fund (MRFF) Primary Health Care Research Grant (APP1200314).
References
Aboriginal and Torres Strait Islander Health Practice Board (2020) Professional capabilities for registered Aboriginal and Torres Strait Islander Health Practitioners. Available at https://www.atsihealthpracticeboard.gov.au/Codes-Guidelines/Professional-capabilities.aspx
Amos B, Bailes B, Baxter S, Burgoyne T, Johnson G, King M, Pollard M, Stewart M, Giaretto A, Graham A (2002) Report: an eye health program for Aboriginal health workers in South Australia. Aboriginal and Islander Health Worker Journal 26, 22-24.
| Google Scholar |
Australian Government (2022) HLT40221 – Certificate IV in Aboriginal and/or Torres Strait Islander Primary Health Care Practice (Release 1). Available at https://training.gov.au/Training/Details/HLT40221#tableUnits
Bernardes CM, Valery PC, Arley B, Pratt G, Medlin L, Meiklejohn JA (2020) Empowering voice through the creation of a safe space: an experience of Aboriginal women in regional Queensland. International Journal of Environmental Research and Public Health 17, 1476.
| Crossref | Google Scholar |
Colleran K, Harding E, Kipp BJ, Zurawski A, MacMillan B, Jelinkova L, Kalishman S, Dion D, Som D, Arora S (2012) Building capacity to reduce disparities in diabetes: training community health workers using an integrated distance learning model. The Diabetes Educator 38, 386-396.
| Crossref | Google Scholar | PubMed |
Colmer K, Kumar S, Jesudason D, Mejia G, Wittert G, Wischer N, Zoungas S, Zimmet P, Brown A, Morey M, Giles J, Jones S, Pearson O (2020) Supporting best practice in the management of chronic diseases in primary health care: a scoping review protocol of training programs for Indigenous health workers/practitioners. Available at https://osf.io/9dh67
Croager EJ, Eades T, Pratt IS, Slevin T (2010) Impact of a short, culturally relevant training course on cancer knowledge and confidence in Western Australia’s Aboriginal Health Professionals. Australian and New Zealand Journal of Public Health 34, S76-S79.
| Crossref | Google Scholar | PubMed |
Cueva M, Kuhnley R, Revels LJ, Cueva K, Dignan M, Lanier AP (2013) Bridging storytelling traditions with digital technology. International Journal of Circumpolar Health 72, 20717.
| Crossref | Google Scholar |
Cueva M, Kuhnley R, Lanier A, Dignan M, Revels L, Schoenberg NE, Cueva K (2016) Promoting culturally respectful cancer education through digital storytelling. International Journal of Indigenous Health 11, 34-49.
| Crossref | Google Scholar | PubMed |
Cueva K, Cueva M, Revels L, Dignan M (2018a) Culturally-relevant online education improves health workers’ capacity and intent to address cancer. Journal of Community Health 43, 660-666.
| Crossref | Google Scholar | PubMed |
Cueva K, Revels L, Cueva M, Lanier AP, Dignan M, Viswanath K, Fung TT, Geller AC (2018b) Culturally-relevant online cancer education modules empower Alaska’s community health aides/practitioners to disseminate cancer information and reduce cancer risk. Journal of Cancer Education 33, 1102-1109.
| Crossref | Google Scholar | PubMed |
Cueva K, Cueva M, Revels L, Hensel M, Dignan M (2019) An evaluation of cancer education webinars in Alaska. Journal of Cancer Education 36, 484-490.
| Crossref | Google Scholar |
Curtis K, Fry M, Shaban RZ, Considine J (2017) Translating research findings to clinical nursing practice. Journal of Clinical Nursing 26, 862-872.
| Crossref | Google Scholar | PubMed |
Davidson PM, Digiacomo M, Abbott P, Zecchin R, Heal PE, Mieni L, Sheerin N, Smith J, Mark A, Bradbery B, Davison J (2008) A partnership model in the development and implementation of a collaborative, cardiovascular education program for Aboriginal Health Workers. Australian Health Review 32, 139-146.
| Crossref | Google Scholar | PubMed |
Doorenbos AZ, Kundu A, Eaton LH, Demiris G, Haozous EA, Towle C, Buchwald D (2011) Enhancing access to cancer education for rural healthcare providers via telehealth. Journal of Cancer Education 26, 682-686.
| Crossref | Google Scholar | PubMed |
Dudgeon P, Ugle K (2014) Communicating and engaging with diverse communities. In ‘Working together: Aboriginal and Torres Strait Islander mental health and wellbeing principles and practice’. (Eds PM Dudgeon, H Milroy, R Walker) pp. 257–267. (Australian Government Department of the Prime Minister and Cabinet)
Durey A, Halkett G, Berg M, Lester L, Kickett M (2017) Does one workshop on respecting cultural differences increase health professionals’ confidence to improve the care of Australian Aboriginal patients with cancer? An evaluation. BMC Health Services Research 17, 660.
| Crossref | Google Scholar |
Glazier RH, Bajcar J, Kennie NR, Willson K (2006) A systematic review of interventions to improve diabetes care in socially disadvantaged populations. Diabetes Care 29, 1675-1688.
| Crossref | Google Scholar | PubMed |
Gomersall JS, Gibson O, Dwyer J, O’Donnell K, Stephenson M, Carter D, Canuto K, Munn Z, Aromataris E, Brown A (2017) What Indigenous Australian clients value about primary health care: a systematic review of qualitative evidence. Australian and New Zealand Journal of Public Health 41, 417-423.
| Crossref | Google Scholar | PubMed |
Grant MJ, Booth A (2009) A typology of reviews: an analysis of 14 review types and associated methodologies. Health Information & Libraries Journal 26, 91-108.
| Crossref | Google Scholar | PubMed |
Hare MJL, Zhao Y, Guthridge S, Burgess P, Barr ELM, Ellis E, Butler D, Rosser A, Falhammar H, Maple-Brown LJ (2022) Prevalence and incidence of diabetes among Aboriginal people in remote communities of the Northern Territory, Australia: a retrospective, longitudinal data-linkage study. BMJ Open 12(5), e059716.
| Crossref | Google Scholar |
Harfield SG, Davy C, McArthur A, Munn Z, Brown A, Brown N (2018) Characteristics of Indigenous primary health care service delivery models: a systematic scoping review. Globalization and Health 14, 12.
| Crossref | Google Scholar | PubMed |
Higgins R, Murphy B, Worcester M, Daffey A (2012) Supporting chronic disease self-management: translating policies and principles into clinical practice. Australian Journal of Primary Health 18, 80-87.
| Crossref | Google Scholar | PubMed |
Iseke J (2013) Indigenous storytelling as research. International Review of Qualitative Research 6, 559-577.
| Crossref | Google Scholar |
Jull J, Hizaka A, Sheppard AJ, Kewayosh A, Doering P, MacLeod L, Joudain G, Plourde J, Dorschner D, Habash M, Graham ID (2019) An integrated knowledge translation approach to develop a shared decision-making strategy for use by Inuit in cancer care: a qualitative study. Current Oncology 26, 192-204.
| Crossref | Google Scholar | PubMed |
King M, Sinn A (1999) An account from five Aboriginal health workers who undertook the Diabetes Educators Course conducted by Flinders University. Aboriginal and Islander Health Worker Journal 23, 19-23.
| Google Scholar |
King M, Munt R, Eastwood A (2007) The impact of a postgraduate diabetes course on the perceptions Aboriginal health workers and supervisors in South Australia. Contemporary Nurse 25, 82-93.
| Crossref | Google Scholar | PubMed |
King C, Goldman A, Gampa V, Smith C, Muskett O, Brown C, Malone J, Sehn H, Curley C, Begay M-G, Nelson AK, Shin SS (2017) Strengthening the role of community health representatives in the Navajo Nation. BMC Public Health 17, 348.
| Crossref | Google Scholar | PubMed |
Look MA, Baumhofer NK, Ng-Osorio J, Furubayashi JK, Kimata C (2008) Diabetes training of community health workers serving native Hawaiians and Pacific People. The Diabetes Educator 34, 834-840.
| Crossref | Google Scholar | PubMed |
Martyn J-A, Woolcock A (2020) An appreciative inquiry to identify the continuing education needs of Aboriginal and Torres Strait Islander health practitioners in regional Queensland. The Australian Journal of Indigenous Education 50, 320-330.
| Crossref | Google Scholar |
McDermott RA, Schmidt B, Preece C, Owens V, Taylor S, Li M, Esterman A (2015) Community health workers improve diabetes care in remote Australian Indigenous communities: results of a pragmatic cluster randomized controlled trial. BMC Health Services Research 15, 68.
| Crossref | Google Scholar | PubMed |
McRae M, Taylor S, Swain L, Sheldrake C (2008) Evaluation of a pharmacist-led, medicines education program for Aboriginal health workers. Rural and Remote Health 8, 946.
| Crossref | Google Scholar |
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine 6, e1000097.
| Crossref | Google Scholar | PubMed |
Moleta CD, Look MA, Trask-Batti MK, Mabellos T, Mau ML (2017) 2016 writing contest graduate winner: cardiovascular disease training for community health workers serving native Hawaiians and other Pacific Peoples. Hawai’i Journal of Medicine & Public Health 76, 190-198.
| Google Scholar | PubMed |
Munn Z, Porritt K, Lockwood C, Aromataris E, Pearson A (2014a) Establishing confidence in the output of qualitative research synthesis: the ConQual approach. BMC Medical Research Methodology 14, 108.
| Crossref | Google Scholar | PubMed |
National Aboriginal and Torres Strait Islander Health Worker Association (2012) The Aboriginal and Torres Strait Islander Health Worker Professional Practice Framework. ACT. Available at https://www.natsihwa.org.au/aboriginal-and-torres-strait-islander-health-worker-professional-practice-framework
National Aboriginal Community Controlled Health Organisation (NACCHO) (2019) The importance of Aboriginal and/or Torres Strait Islander Health Workers and Health Practitioners in Australia’s health system: position statement. Available at https://www.natsihwa.org.au/sites/default/files/position_statmente_importance_aboriginal_torres_strait_islander_hw_hp_in_aust_health_system_aug_2019.pdf
NSW Ministry of Health (2018) Aboriginal health worker guidelines for NSW Health. NSW Health, NSW. Available at https://www.health.nsw.gov.au/workforce/aboriginal/Pages/aboriginal-health-worker-guidelines.aspx
Orr AL (1993) Training outreach workers to serve American Indian elders with visual impairment and diabetes. Journal of Visual Impairment & Blindness 87, 336-340.
| Crossref | Google Scholar |
Pantoja T, Opiyo N, Lewin S, Paulsen E, Ciapponi A, Wiysonge CS, Herrera CA, Rada G, Penaloza B, Dudley L, Gagnon M-P, Garcia Marti S, Oxman AD (2017) Implementation strategies for health systems in low-income countries: an overview of systematic reviews (Review). Cochrane Database of Systematic Reviews 9, CD011086.
| Crossref | Google Scholar |
Peters M, Godfrey C, McInerney P, Munn Z, Tricco A, Khalil H (2020) Chapter 11: Scoping reviews. In ‘JBI manual for evidence synthesis’. (Eds E Aromataris, Z Munn) pp. 407–450. (JBI: Adelaide, SA, Australia) doi:10.46658/JBIMES-20-12
Phillips GL (2017) Dancing with power: Aboriginal health, cultural safety and medical education. PhD Thesis, Monash University. Available at https://doi.org/10.4225/03/58b774b372862
Policicchio JM, Dontje K (2018) Diabetes training for community health workers on an American Indian reservation. Public Health Nursing 35, 40-47.
| Crossref | Google Scholar | PubMed |
Pálsdóttir B, Barry J, Bruno A, Barr H, Clithero A, Cobb N, De Maeseneer J, Kiguli-Malwadde E, Neusy A-J, Reeves S, Strasser R, Worley P (2016) Training for impact: the socio-economic impact of a fit for purpose health workforce on communities. Human Resources for Health 14, 49.
| Crossref | Google Scholar | PubMed |
Ryder C, Mackean T, Coombs J, Williams H, Hunter K, Holland AJA, Ivers RQ (2020) Indigenous research methodology – weaving a research interface. International Journal of Social Research Methodology 23, 255-267.
| Crossref | Google Scholar |
Sebastian S, Thomas DP, Brimblecombe J, Arley B, Cunningham FC (2021) Perceived impact of the characteristics of the Indigenous Queensland B.strong brief intervention training program on uptake and implementation. Health Promotion Journal of Australia 33, 245-256.
| Crossref | Google Scholar |
Smith RL, Devine S, Preston R (2020) Recommended methodologies to determine Australian Indigenous community members’ perceptions of their health needs: a literature review. Australian Journal of Primary Health 26, 95-103.
| Crossref | Google Scholar | PubMed |
Thorpe S, Browne J (2009) Heart health action in Aboriginal communities: translating training into practice: final evaluation report. (Heart FoundationVictorian Aboriginal Community Controlled Health Organisation Inc.: Victoria) Available at https://www.vaccho.org.au/assets/01-RESOURCES/TOPIC-AREA/NUTRITION/Health-Action-in-Aboriginal-Communities-eval-Report-Final-2009-09-18.pdf
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. (2018) PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Annals of Internal Medicine 169, 467-473.
| Crossref | Google Scholar | PubMed |
West R, Armao JE, Creedy DK, Saunders V, Rowe Minnis F (2021) Measuring effectiveness of cultural safety education in First Peoples health in university and health service settings. Contemporary Nurse 57, 356-369.
| Crossref | Google Scholar | PubMed |
Wilson AM, Kelly J, Jones M, O’Donnell K, Wilson S, Tonkin E, Magarey A (2020) Working together in Aboriginal health: a framework to guide health professional practice. BMC Health Services Research 20, 601.
| Crossref | Google Scholar | PubMed |
Zeunert S, Cerro N, Boesch L, Duff M, Shephard MD, Jureidini KF, Braun J (2002) Nutrition project in a remote Australian aboriginal community. Journal of Renal Nutrition 12, 102-106.
| Crossref | Google Scholar | PubMed |