Unprecedented increase in syphilis cases among heterosexual men and women in Japan, 2021–2022
Ayu Kasamatsu A , Takuri Takahashi A , Yuzo Arima
A , Takuri Takahashi A , Yuzo Arima  A * , Miyako Otsuka A , Takeshi Arashiro A , Hanae Ito B , Sakiko Tabata B , Takuya Yamagishi
A * , Miyako Otsuka A , Takeshi Arashiro A , Hanae Ito B , Sakiko Tabata B , Takuya Yamagishi  C and Motoi Suzuki A
C and Motoi Suzuki A
A Center for Surveillance, Immunization and Epidemiologic Research, National Institute of Infectious Diseases, Tokyo, Japan.
B Field Epidemiology Training Program, National Institute of Infectious Diseases, Tokyo, Japan.
C Center for Field Epidemic Intelligence, Research and Professional Development, National Institute of Infectious Diseases, Tokyo, Japan.
Sexual Health 20(4) 370-372 https://doi.org/10.1071/SH23031
Submitted: 14 February 2023 Accepted: 19 May 2023 Published: 7 June 2023
© 2023 The Author(s) (or their employer(s)). Published by CSIRO Publishing
Abstract
Based on national surveillance data, we describe an unprecedented increase in syphilis case reports in Japan, with a surge in 2021–2022 reaching 10 141 cases in Week 42, 2022, a 1.7-fold increase over the same period in 2021. This already represented the highest annual case count in nearly half a century; by Week 52, 2022, the number reached 12 966, far surpassing the 7978 cases in 2021. Predominantly affecting heterosexual men and young women, the proportionate increase in primary and secondary syphilis cases suggests a true increase in incidence. The syphilis surge during the pandemic poses a serious public health concern and underscores the importance of adequate testing and preventive measures.
Keywords: age distribution, Asia, congenital, epidemiology, Japan, sexually transmitted diseases, surveillance, syphilis.
Amid the coronavirus disease 2019 (COVID-19) pandemic, Japan has been facing another public health challenge – syphilis has dramatically increased, despite reduced social contacts at the population level.
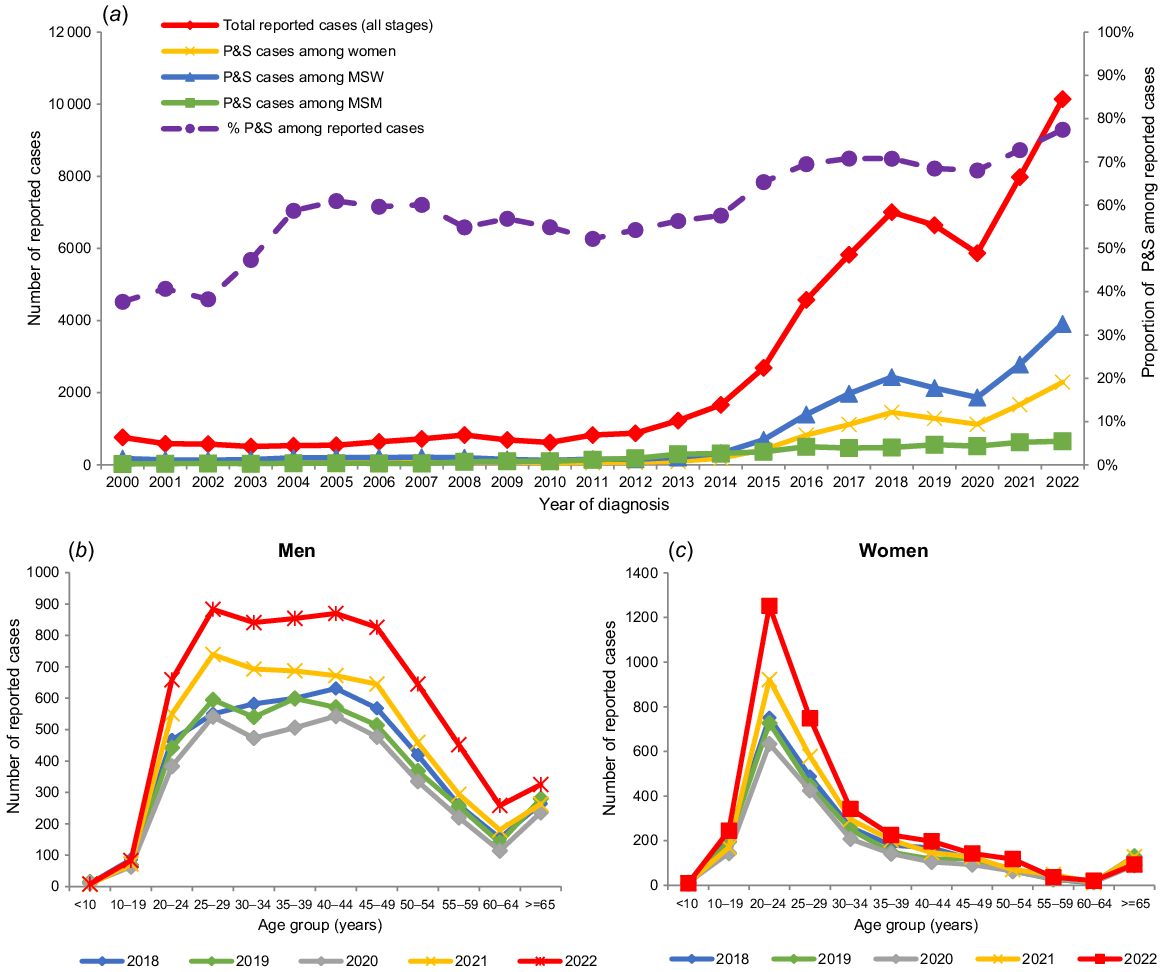
Syphilis is legally notifiable in Japan, requiring reporting of all laboratory-confirmed cases.1 Notifications of syphilis (all stages), including primary and secondary syphilis (P&S), had continued to rise since 2011 but showed a decline in 2019–2020 (Fig. 1a). Since 2021, however, notifications increased again, reaching a record high; cases diagnosed in Weeks 1–42 of 2022 (as at 26 October 2022) reached 10 141 (8.0 per 100 000), marking the highest annual count in nearly half a century.2 This was 1.7 times higher than the same period in 2021 (n = 6031), with P&S accounting for 77.4% (7853) in 2022.
(a) Number of reported syphilis cases by stage of infection, sex, and sex of sex partner (sexual transmission route),* Japan, 2000–2022; age distribution of reported syphilis cases by sex, Japan, 2016–2022: (b) men, (c) women. *Sexual transmission route was based on self-reporting. Male cases with a recent history of sexual contact with men were classified as MSM. MSW, men who have sex with women; MSM, men who have sex with men; P&S, primary and secondary syphilis.
While Tokyo (20.6 per 100 000) and Osaka prefectures (15.5 per 100 000) had the highest case counts and those per capita,2 the current surge has been nationwide; case counts increased in 45/47 prefectures during 2021–2022.
The unprecedented rise has been associated with an increase in reported heterosexual syphilis. While men who have sex with men (MSM) had hitherto been disproportionately affected, both P&S cases among men who have sex with women (MSW) and women have been increasing (Fig. 1a). The P&S case counts among MSW was similar to that among MSM in 2011, but increased to six times that among MSM in 2022. This trend may reflect the limited overlap of sexual networks between heterosexual and MSM communities, as indicated by clearly different Treponema pallidum molecular profiles.3 Notably, age distribution differed considerably by sex, with male cases ranging mostly aged 20−50 years, while female cases were predominantly aged in their early 20s (Fig. 1b, c).2 This peak among female cases has not shifted for a decade,4 indicating a sustained disproportionate risk in this particular age group,5 rather than a specific birth cohort. Also, approximately 30–40% of male and female cases reported having a recent history of utilising or providing commercial sex, respectively.6
With increase in syphilis among young women, there is concern regarding congenital syphilis. Indeed, approximately 200 cases among pregnant women have been reported annually in recent years,7 and annual congenital syphilis case reports have been increasing, from 1–12 during 2000–2013 (median 6) to 9–23 (median 16) during 2014–2021.
Surveillance data can be influenced by changes in healthcare-seeking behaviour, awareness among patients/physicians, or testing practices. Nonetheless, the following suggest a true rise in incidence. First, the P&S proportion has risen in recent years (including 2021 and 2022) along with the total case counts (Fig. 1a), which cannot be explained by more incidental diagnoses through increased testing among asymptomatic persons. Second, congenital syphilis has increased concomitantly with P&S among MSW and women, suggesting an actual heterosexual epidemic. Third, with very little change in the number of days from visit to diagnosis or from diagnosis to report during 2017–2021, there is no clear indication of enhanced surveillance sensitivity. Lastly, a survey on domestic postal syphilis testing practices found that the number of positive tests in 2021 was higher than in 2020, despite a lower number of tests.8 This pattern raises the concern that testing may not be keeping up with the actual increase in syphilis.
The annual case counts for 2022 (Weeks 1–52) reached 12 966 (vs 7978 notifications in 2021), with their trends and distributions remaining similar to those diagnosed through Week 42 (as at 5 January 2023).6 With a true and unprecedented epidemic, early treatment and preventive measures to minimise serious health consequences are urgent issues for the medical and public health sectors. Information-sharing on the epidemiological characteristics of syphilis cases, providing adequate testing opportunities for the disproportionately affected, and risk communication for prevention are crucial.
Data availability
Data for this analysis are publicly available from National Institute of Infectious Diseases; Ministry of Health, Labour and Welfare, Japan. Infectious Diseases Weekly Report Japan (Japanese). Available at https://www.niid.go.jp/niid/ja/idwr.html.
Declaration of funding
This work was supported by grants from the Ministry of Health, Labour and Welfare, Japan (grant no. 21HA1003).
Ethical statement
Information on reported cases was collected under the Infectious Diseases Control Law. The use of national surveillance data for public health purposes does not require informed consent from the patient or ethical approval from the relevant authorities.
Author contributions
AK, TT, and YA designed the study. All authors verified the data. AK, TT, YA and MO analysed and interpreted the data. AK wrote the first draft of the manuscript. TT, YA, MO, TA, HI, ST, TY, and MS reviewed and provided important comments on the draft manuscript. TY obtained the funding. YA, and MS provided administrative or material support. All authors read and approved the manuscript.
Acknowledgements
This work was based on data reported by physicians, public health centers (PHCs), and prefectural and municipal public health institutes (PHIs) to the NESID system, managed by the National Institute of Infectious Diseases and the Ministry of Health, Labour and Welfare of Japan. We gratefully appreciate staff members from the PHCs and PHIs, along with the reporting physicians, for providing surveillance information. The authors greatly appreciate Dr. Shu-ichi Nakayama and Dr. Yukihiro Akeda for providing valuable comments about the manuscript.
References
1 National Institute of Infectious Diseases. Reporting criteria for syphilis. Infectious Agents Surveillance Report; 2015. Available at https://www.niid.go.jp/niid/images/iasr/36/420/de4201.pdf [cited 11 October 2022].
2 National Institute of Infectious Diseases. Infectious disease weekly report week 42; 2022. Available at https://www.niid.go.jp/niid/ja/syphilis-m-3/syphilis-idwrc/11612-idwrc-2242.html [cited 7 November 2022].
3 Kanai M, Arima Y, Nishiki S, Shimuta K, Itoda I, Matsui T, et al. Molecular typing and macrolide resistance analyses of Treponema pallidum in heterosexuals and men who have sex with men in Japan, 2017. J Clin Microbiol 2019; 57(1): e01167-18.
| Crossref | Google Scholar |
4 Takahashi T, Arima Y, Yamagishi T, Nishiki S, Kanai M, Ishikane M, et al. Rapid increase in reports of syphilis associated with men who have sex with women and women who have sex with men, Japan, 2012 to 2016. Sex Transm Dis 2018; 45(3): 139-43.
| Crossref | Google Scholar |
5 Ministry of Health Labour and Welfare. Vital statistics. Available at https://www.mhlw.go.jp/toukei/list/81-1a.html [cited 7 April 2023].
6 National Institute of Infectious Diseases. Notification trends among syphilis cases in Japan; 2022. Available at https://www.niid.go.jp/niid/ja/syphilis-m/syphilis-trend.html [cited 17 April 2023].
7 National Institute of Infectious Diseases. Pregnant cases and female commercial sex worker cases among reported syphilis cases based on the national epidemiological surveillance of infectious diseases system, 2019–2021; 2022. Available at https://www.niid.go.jp/niid/ja/syphilis-m-3/syphilis-idwrs/11654-syphilis-20221130.html [cited 3 December 2022].
8 Sudo K, Sano T, Kondo M, Imai M, Kato S, Imamura A. Health labour sciences research grant. Research report for improvement of HIV testing system and effective recommendation of HIV testing, survey on testing situation and accuracy of HIV mailed testing; 2021. Available at https://mhlw-grants.niph.go.jp/system/files/report_pdf/202120002A-buntan6.pdf [cited 21 November 2022].


