Impact of the COVID-19 pandemic on primary care delivery in a remote Aboriginal community
Yasuchiyo Hamilton A * , Alice Cairns B * and Rhondda Jones CA School of Medicine and Dentistry, Griffith University, Southport, Qld, Australia.
B Australia Institute of Tropical Health and Medicine, Murtupini Centre for Rural and Remote Health, James Cook University, Townsville, Qld, Australia.
C James Cook University, Tropical Australian Academic Health Centre, Townsville, Qld, Australia.
Australian Journal of Primary Health 29(5) 416-421 https://doi.org/10.1071/PY23026
Submitted: 20 February 2023 Accepted: 24 April 2023 Published: 19 May 2023
Abstract
The coronavirus disease 2019 (COVID-19) pandemic has disrupted the delivery of primary health care internationally, particularly for the most marginalised groups. This project investigated the impact of the initial response to the COVID-19 pandemic on the delivery of primary health care in a remote First Nations community in Far North Queensland with a high chronic disease burden. There were no confirmed cases of COVID-19 circulating in the community at the time of the study. A comparison was conducted of patient numbers presenting to a local primary healthcare centre (PHCC) in the periods before, during and after the initial peak of Australian COVID-19 restrictions in 2020, compared to the same period in 2019. A significant proportional decrease was observed in the number of patients that presented from the target community during the initial restrictions. A sub-analysis of preventative services delivered to a defined high-risk group found that services delivered did not decrease to this particular group during the periods of interest. This study has highlighted that there is a risk of underutilisation of primary healthcare services during a health pandemic in remote settings. Strengthening the primary care system to adequately provide ongoing services during natural disasters requires further consideration to reduce the risk of long-term impacts of service disengagement.
Keywords: chronic disease management, community health, First Nations, Indigenous, pandemic, preventative health, public health services, rural health, telehealth, Torres Strait Islander.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has disrupted the delivery of primary health care internationally, particularly for the most marginalised groups. This project investigated the impact of the initial COVID-19 pandemic response on the delivery of primary health care in a remote First Nations community in Far North Queensland. There were no confirmed cases of COVID-19 circulating in the community at the time of the study. A comparison was conducted of patient numbers presenting to a local primary healthcare centre (PHCC) in the periods before, during and after the initial peak of Australian COVID-19 restrictions in 2020, compared to the same period in 2019. A significant proportional decrease was observed in the number of patients that presented from the target community during the initial restrictions. A sub-analysis of preventative services delivered to a defined high-risk group found that services did not decrease to this group. This study highlighted that although there is a risk of underutilisation of primary healthcare services during health emergencies, a case management model can mitigate this risk for patients with high chronic disease management needs.
Context
The participating PHCC is based in a remote First Nations community in Cape York, Queensland. A small hospital approximately 10 km away provides after-hours and emergency services. The community population is approximately 900 people with 90% identifying as Aboriginal and/or Torres Strait Islander (Australian Bureau of Statistics 2021). Representative of most remote First Nations communities, chronic disease rates are high, with complex socioeconomic and cultural issues that impact wellbeing. The study site was a state-run PHCC that delivers health care through partnerships between nursing staff, Aboriginal and Torres Strait Islander Health Workers, and visiting medical specialists and allied health.
Review of literature
Primary care forms the foundation of the Australian healthcare system. Health security requires healthcare systems that are oriented towards delivering strong primary care, which in turn is associated with lower overall national healthcare costs (World Health Organization 2018). General practitioners (GPs) and other primary care services play a crucial role during health disasters, including pandemics, in the acute and recovery phases of pandemics, as well as continuing to manage chronic illnesses and other health problems, regardless of the presence of emergency situations (RACGP 2017). Disasters have the potential to indirectly impact the health of a population due to the redirection of health care to more acute care, potentially at the expense of primary and secondary prevention (Verhoeven et al. 2020). Worldwide, the consequences of this change in primary care provision have resulted in the largest sustained decline in childhood vaccination rates in over 30 years (World Health Organization 2022), a reduction in cancer pathology notifications in Victoria (te Marvelde et al. 2021), and a sudden halt in progress in key First Nations health outcomes, such as the goal of eliminating trachoma by the end of 2020 (Anjou 2021).
First Nations people living in remote communities were identified early as being at greater risk from the consequences of COVID-19 infection (Crooks et al. 2020). The diversion of staff to acute/COVID-19 response services and a reduced fly-in/fly-out workforce potentially impacted the delivery of primary healthcare services for remote First Nations communities. There are many complex inter-related factors that result in greater vulnerability for Australian’s First Nations people, including socioeconomic disadvantage, an increased chronic disease burden, and cultural practices that make public health measures difficult to fully enact (Crooks et al. 2020).
There has been research looking at the impact of the COVID-19 pandemic on healthcare staff, including in primary care (Gibbs 2020). However, research on the impact of the COVID-19 pandemic on primary care delivery in First Nations populations is lacking. Broadly, primary healthcare clinics have seen a decrease in patient numbers and chronic care delivery (Verhoeven et al. 2020). However, the impact of the COVID-19 pandemic on primary care delivery in First Nations communities in remote locations has not been explicitly explored, despite potential increased vulnerabilities to these changes. Therefore, the aim of this study was to explore if the delivery of primary healthcare services changed at a single remote primary healthcare clinic during the COVID-19 pandemic.
Case study
This post observational investigation included all patients presenting to the participating PHCC during three 6-week blocks during the initial public health COVID-19 pandemic response:
Block 1: 6 February 2020 – 20 March 2020, before widespread awareness of COVID-19 in Australia, during which case numbers in Australia began to escalate, but general community awareness was poor.
Block 2: 21 March 2020 – 01 May 2020, during the first national lockdown when Australia closed its international borders to all non-residents and social distancing rules were imposed.
Block 3: 2 May 2020 – 12 June 2020, after the initial lockdown period, which coincided with the easing of a number of public health restrictions in Queensland, Australia.
Data were also collected for each block from the corresponding dates in 2019 for comparison.
De-identifiable data were collected from consecutive clinical charts by a research team member. The electronic patient billing information record system records item numbers claimed under the Medicare Benefits Schedule (MBS). It was used to identify all patients who presented to the PHCC and were reviewed by a GP or nurse practitioner (NP), as well as the age and gender of each patient. Services delivered by other health professionals in this clinic are not recorded using the MBS and therefore were not captured in this study.
A subsection of the community was identified by the health service as being medically and/or socially vulnerable to COVID-19. Vulnerability was defined by: being treated for a chronic condition or immunocompromised; aged >50 years and of Aboriginal and/or Torres Strait Islander origin; being an active smoker; or having a mental health condition. These patients were included in a sub-analysis of chronic disease health activities if they had concomitant diagnoses of hypertension, type two diabetes mellitus and chronic kidney disease (any stage). The paper-based medical record for each patient from the identified subgroup was reviewed and all patient–PHCC interactions manually recorded. Preventable health activities were recorded as (Yes/No). A preventable activity was defined as a blood pressure check, weight measurement, pathology review, alcohol and smoking status review, and a dental check within 12 months.
Data analyses used the base package of R ver. 4.2.1 (R Foundation for Statistical Computing, Vienna, Austria). The R package, ggplot2, was used to generate plots (Wickham 2016) and the car package (Fox and Weisberg 2019) to apply analyses of deviance to quasi-Poisson and logistic regression models.
Total cohort data analysis
Distribution of consultations and service days among years, periods, demographic groups, and service providers was tabulated.
Differences between years in the proportion of consultations occurring in each period were evaluated using a χ2 test. Preliminary models of consultations per service day using Poisson regression proved to be overdispersed, so more detailed examination of the factors affecting numbers of consultations per service day used quasi-Poisson regression, with an analysis of deviance to evaluate the impact of each explanatory variable. Explanatory variables initially examined YEAR, PERIOD, and a YEAR:PERIOD interaction. Because availability of different service providers differed between days of the week, WEEKDAY was also included in the model.
To examine whether different demographic groups were affected differently by PERIOD and YEAR, the number of consultations for each service day were subdivided according to demographic attribute (GENDER and AGE GROUP) and re-analysed, including the relevant demographic attribute as a potential explanatory variable. To examine whether the effects of PERIOD and YEAR varied according to provider type (GP or NP), the number of consultations for each service day were subdivided according to provider type and re-analysed.
Treatment frequencies for each different patient demographics and total number of consultations per year per period of interest, as well as distribution of GP and NP reviews, are summarised in Table 1, and a summary of service days is presented in Table 2. Although the total number of consultations in each year was similar, the distribution of consultations among the three periods differed between years (χ2 = 31.56, d.f. = 2, P = 0.00000014).
| Variables | Total | 2019 | 2020 | |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| Sex | ||||
| Male | 705 (44) | 377 (46) | 328 (41) | |
| Female | 914 (56) | 435 (54) | 479 (59) | |
| Age (years) | ||||
| <6 | 114 (7) | 70 (9) | 44 (5) | |
| 6–18 | 166 (10) | 90 (11) | 76 (9) | |
| 19–35 | 342 (21) | 173 (21) | 169 (21) | |
| 36–50 | 427 (26) | 226 (28) | 201 (25) | |
| >50 | 570 (35) | 253 (31) | 317 (39) | |
| Provider | ||||
| Nurse practitioner | 397 (25) | 157 (19) | 240 (30) | |
| General practitioner | 1221 (75) | 655 (81) | 566 (70) | |
| Period | ||||
| Block 1 | 615 (38) | 270 (33) | 345 (43) | |
| Block 2 | 484 (30) | 293 (36) | 191 (24) | |
| Block 3 | 520 (32) | 249 (31) | 271 (33) | |
| Total | 1619 | 812 | 807 | |
| WeekdayA | ||||
| Monday | 419 (26) | 218 (27) | 201 (25) | |
| Tuesday | 427 (26) | 213 (26) | 214 (27) | |
| Wednesday | 386 (24) | 211 (26) | 175 (22) | |
| Thursday | 326 (20) | 143 (18) | 183 (23) | |
| Friday | 55 (4) | 24 (3) | 31 (4) | |
AThere were six episodes of care documented in data pulled from the Patient Information Recall System used by the health service as having occurred on Saturday or Sunday, during which the PHCC does not open. The weekday for these six episodes were treated as missing values in analyses, which included day of the week as a variable.
| Variable and period | N | 2019 | 2020 | |
|---|---|---|---|---|
| Nurse practitioner | ||||
| Block 1 | 43 | 23 | 20 | |
| Block 2 | 39 | 16 | 23 | |
| Block 3 | 30 | 8 | 22 | |
| Total | 112 | 47 | 65 | |
| General practitioner | ||||
| Block 1 | 49 | 23 | 26 | |
| Block 2 | 44 | 22 | 22 | |
| Block 3 | 48 | 25 | 23 | |
| Total | 141 | 70 | 71 | |
Further analyses of deviance included GENDER and AGE GROUP as possible explanatory variables. The only significant interaction involving gender is a relatively weak association with provider, with an overall greater number of consultations with females than with males for NPs and a higher proportion of consultations with male patients for GPs, Likelihood Ratio (LR) χ2 (5.991, N = 757, d.f. = 1, P < 0.05). GP consultations involved more patients aged <18 years and >50 years, LR χ2 (26.106, N = 757, d.f. = 4, P < 0.001). There were no interactions of either GENDER or AGE GROUP with YEAR or PERIOD, meaning differential presentation to the clinic was similar for both genders and for all age groups.
Subgroup data analysis
For the group of 33 patients followed through the study period, the numbers of missed appointments or ‘did not attend’ (DNA) were tabulated, and the proportion of appointments missed were calculated for each combination of PERIOD and YEAR.
Effects on the number of preventative activities undertaken at each consultation were modelled with a quasi-Poisson regression, using PERIOD, YEAR, the PERIOD:YEAR interaction, appointment type (acute vs preventative) and attendance (DNA or not) as potential explanatory variables. For both logistic and quasi-Poisson regressions, the overall impact of each explanatory variable was examined via an analysis of deviance using the car package in R.
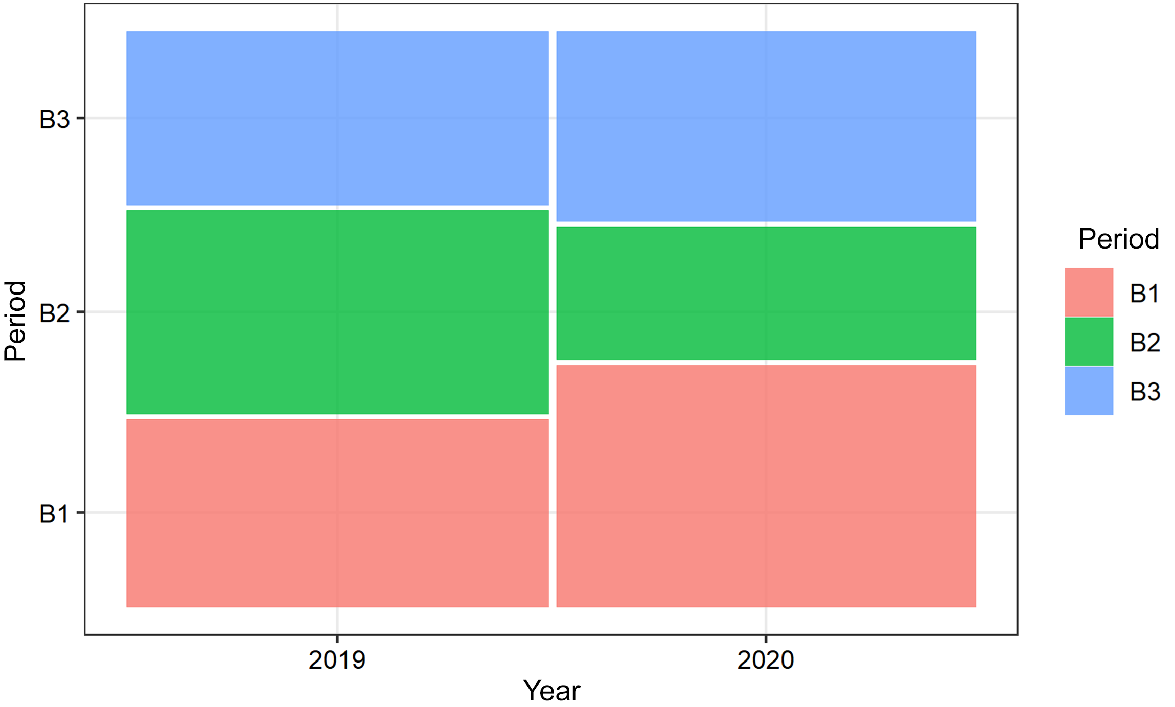
Effects on the proportion of preventative appointments and DNA proportion were modelled using a logistic regression with proportion preventative and proportion DNA, respectively, as the response variables (weighted by number of appointments from which proportions were calculated), and using PERIOD, YEAR, and the interaction between them as potential explanatory variables (Fig. 1).
The total number of appointments did not differ significantly between period-year combinations. The average number of preventative activities per appointment was 4.44 (CI 4.10–4.79), with values ranging from 0 to 13. The proportion of appointments classified as preventative versus acute did differ between PERIOD–YEAR combinations (LR χ2 = 9.98, d.f. = 2, P = 0.0068), with the highest proportion of preventative activities occurring during the 2020 COVID-19 period B2. The proportion of DNA did not vary significantly between PERIOD–YEAR combinations in this subgroup.
Ethics approval
The study was approved by the Human Research Ethics Committee of the Torres and Cape Hospital and Health Service (QCH/73493 (6 March 2021 and 1 May 2021), the Public Health Act (26 October 2020) and research governance (29 November 2021).
Patient consent was waived under section 282 and 284 of the Public Health Act 2005 by the Director-General’s delegate on 26 October 2021.
What can be learnt from the case
This study explored the impact of the initial COVID-19 response on the delivery of primary care in a remote First Nations community, and it highlights the importance of a case management-based model in this setting. The significant reduction in primary care presentations observed during and immediately after the initial COVID-19 restrictions was expected and has been observed in other studies in non-Indigenous settings (Sumner et al. 2022). The findings from this study suggest the reduction in the number was not a result of reduced service availability compared with the same period in 2019. The reduction in patient numbers occurred at a time when Australia was experiencing its first wave of the COVID-19 pandemic, although no cases were recorded in the participating community. Despite the PHCC of interest remaining open, public health and community messaging were urging people to ‘stay at home’ and this likely influenced people to delay non-urgent appointments regardless of baseline health status. As identified by Sumner et al (2022), it is likely that fear of contracting COVID-19 and uncertainty of treatment and prognosis was a factor in reduced healthcare-seeking behaviour. Additional public health screening procedures and misinformation about COVID-19 may also have been an influencing factor in people limiting their engagement with primary care services (Pickles et al. 2021). In the community of interest, Aboriginal and Torres Strait Islander Health Workers play an essential role in maintaining community engagement with the health service and supporting access for those patients who are most disadvantaged. Public health restrictions limited the movement of health staff around the community, which likely further reduced patient engagement.
COVID-19 precautions challenged the way care was delivered at the participating PHCC, with patients encouraged to postpone ‘non-essential’ care. However, chronic disease patients who had regular scheduled visits with NPs (e.g. people diagnosed with diabetes with one of the diabetes educator NPs) continued to be reviewed. Given the subgroup analysis, these results suggest that reductions in overall appointments during the initial COVID-19 lockdown may have been primarily in acute rather than preventative consultations. Both NPs and GPs had fewer consultations per service day in period B2 than in the other two periods, with a greater drop for GP consultations. The B2 drop is not apparent in 2019. This demonstrates that the case management model adopted by NPs for a specific subset of patients is likely to be effective in maintaining regular reviews for these patients. The subgroup analysis demonstrated that in the subgroup of interest, there was no significant difference in the number of appointments between 2019 and 2020 across the different periods. This result indicates that the high-risk group in particular were engaged more deliberately and that this relationship had been built over some time and therefore was more likely to be maintained during the first lockdown period. This supports existing literature that describes NPs caring for patients with complex needs at rates that match their medical colleagues, as well as improved access to essential health care for vulnerable and at-risk populations (Fraze et al. 2020).
The COVID-19 pandemic has demonstrated the need to consider a more culturally nuanced approach to public health restrictions in a health emergency. The lower infection rates in First Nation’s people in Australia compared to Australia’s non-Indigenous population (0.19 vs 1.12 per 1000) (Lowitja Institute 2021) is evidence of effective community leadership and initiatives, supported by the Australian Government’s Indigenous Advancement Strategy (IAS) (Australian Government 2020b). Processes to facilitate community-driven responses to pandemics and other emergencies is urgently needed considering the vulnerability of rural Australians in the context of climate change and subsequent public health consequences, particularly those with pre-existing cardiovascular and respiratory disease (Parise 2018). Telehealth has been shown to be effective in some First Nations settings (St Clair et al. 2018); however, simply replacing face-to-face reviews with telehealth consultations can reduce trust and decrease continuity of care in remote Australian settings (Sutarsa et al. 2022). The use of telehealth rapidly expanded during the COVID-19 pandemic for GP consultations in Australia nationwide; however, in this community, telehealth was often not feasible without support from a healthcare professional physically with the patient, reducing the potential effectiveness of telehealth being an infection control strategy.
This was a retrospective analysis of health service and medical chart information. It is possible relevant data were not correctly recorded and therefore missed during the auditing process. Every effort was taken to reduce this risk, including the manual checking of clinical charts. Data were not collected on unattended appointments, although this could have potentially provided context as to whether it was patients or services driving the reduction in service delivery. This has been addressed somewhat by analysing services on each day of the 6-week blocks and removing days where no services were provided, allowing analysis of whether services were reduced during any one period. This study only collected data from one primary healthcare provider. It is unknown how the services at the Aboriginal Community Controlled Health Service (ACCHO) provider within the community were affected during the periods of interest.
Conclusions
The COVID-19 pandemic has raised ethical and practical dilemmas surrounding the distribution of scarce health resources. This study shows that maintaining primary care services in the remote community of interest was challenging, despite the push nationally for the implementation of telehealth to combat lockdown restrictions. It also demonstrated that a case management model, particularly for vulnerable subsets of the population, is potentially useful for maintaining and optimising care for this cohort during periods of emergency. It reinforces that health systems cannot be complacent and must have strategies in place to enable vulnerable members of the population to continue accessing necessary health care.
Data availability
The data that support this study will be shared upon reasonable request to the corresponding author.
Conflicts of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflicts of interest.
Author contributions
Conceptualisation, Y.H. and A.C.; Methodology, Y.H.; Validation, Y.H.; Formal Analysis, Y.H. and R.J.; Investigation, Y.H.; Resources, Y.H.; Data Curation, Y.H. and R.J.; Writing—Original Draft Preparation, Y.H.; Writing—Review and Editing, Y.H. and A.C.; Supervision, A.C; Project Administration, Y.H.; Funding Acquisition, Y.H. All authors have read and agreed to the published version of the manuscript.
Acknowledgements
The authors would like to acknowledge the Aboriginal community council and the hospital and health service that supported this project.
References
Anjou MD (2021) Keeping the momentum on eye health equity. Partyline. Available at https://www.ruralhealth.org.au/partyline/article/keeping-momentum-eye-health-equity [Accessed March 18]
Australian Government (2020b) Practising and sharing culture while social distancing. Australian Government. Available at indigenous.gov.au
Crooks K, Casey D, Ward JS (2020) First Nations peoples leading the way in COVID-19 pandemic planning, response and management. Medical Journal of Australia 213, 151-152.e1.
| Crossref | Google Scholar |
Fraze TK, Briggs ADM, Whitcomb EK, Peck KA, Meara E (2020) Role of nurse practitioners in caring for patients with complex health needs. Medical Care 58, 853-860.
| Crossref | Google Scholar |
Gibbs B (2020) Exploring the impact of COVID-19 on Australian Primary Health Care. The University of Notre Dame Australia. Available at https://www.notredame.edu.au/news-items/exploring-the-impact-of-covid-19-on-australian-primary-health-care [Accessed 17 April 2021]
Lowitja Institute (2021) Close the gap campaign report 2021: leadership and legacy through crises: keeping our mob safe. (Lowitja Institute) Available at https://humanrights.gov.au/our-work/aboriginal-and-torres-strait-islander-social-justice/publications/close-gap-2021 [Accessed 7 February 2022]
Parise I (2018) A brief review of global climate change and the public health consequences. Australian Journal of General Practice 47(7), 451-456.
| Crossref | Google Scholar |
Pickles K, Cvejic E, Nickel B, Copp T, Bonner C, Leask J, Ayre J, Batcup C, Cornell S, Dakin T, Dodd RH, Isautier JMJ, McCaffery KJ (2021) COVID-19 misinformation trends in Australia: prospective longitudinal national survey. Journal of Medical Internet Research 23(1), e23805.
| Crossref | Google Scholar |
St Clair M, Murtagh D, Kelly J, Ford PL, Wallace R (2018) Telehealth: a game changer – closing the gap in remote indigenous health in three remote homeland communities in the Laynhapuy Homelands, East Arnhem, Northern Australia. Studies in Health Technology and Informatics 252, 132-138.
| Google Scholar |
Sumner J, Bundele A, Chong LS, et al. (2022) Continuing chronic care services during a pandemic: results of a mixed-method study. BMC Health Services Research 22, 1009.
| Crossref | Google Scholar |
Sutarsa IN, Kasim R, Steward B, Bain-Donohue S, Slimings C, Hall Dykgraaf S, Barnard A (2022) Implications of telehealth services for healthcare delivery and access in rural and remote communities: perceptions of patients and general practitioners. Australian Journal of Primary Health 28 522-528.
| Crossref | Google Scholar |
te Marvelde L, Wolfe R, McArthur G, Blake LA, Evans SM (2021) Decline in cancer pathology notifications during the 2020 COVID-19-related restrictions in Victoria. Medical Journal of Australia 214, 281-283.
| Crossref | Google Scholar |
Verhoeven V, Tsakitzidis G, Philips H, Van Royen P (2020) Impact of the COVID-19 pandemic on the core functions of primary care: will the cure be worse than the disease? A qualitative interview study in Flemish GPs. BMJ Open 10, e039674.
| Crossref | Google Scholar |