Lessons from the Netherlands for Australia: cross-country comparison of trends in antidepressant dispensing 2013–2021 and contextual factors influencing prescribing
Katharine A. Wallis A * , Pieter J. S. Dikken A B , Piumika Sooriyaarachchi A , Arthur M. Bohnen B and Maria Donald
A * , Pieter J. S. Dikken A B , Piumika Sooriyaarachchi A , Arthur M. Bohnen B and Maria Donald  A
A
A
B
Abstract
There is concern internationally about increasing antidepressant use. Most antidepressants are prescribed in general practice. The aim of this study was to compare trends in antidepressant dispensing in Australia and the Netherlands over the 9 years from 2013 to 2021, and to explore reasons for differences.
A convergent mixed methods study including analysis of publicly available antidepressant dispensing data obtained from Australia’s Pharmaceutical Benefits Scheme and Repatriation Pharmaceutical Benefits Scheme and the Dutch Foundation for Pharmaceutical Statistics and a search of relevant literature to compare contextual factors influencing prescribing were undertaken.
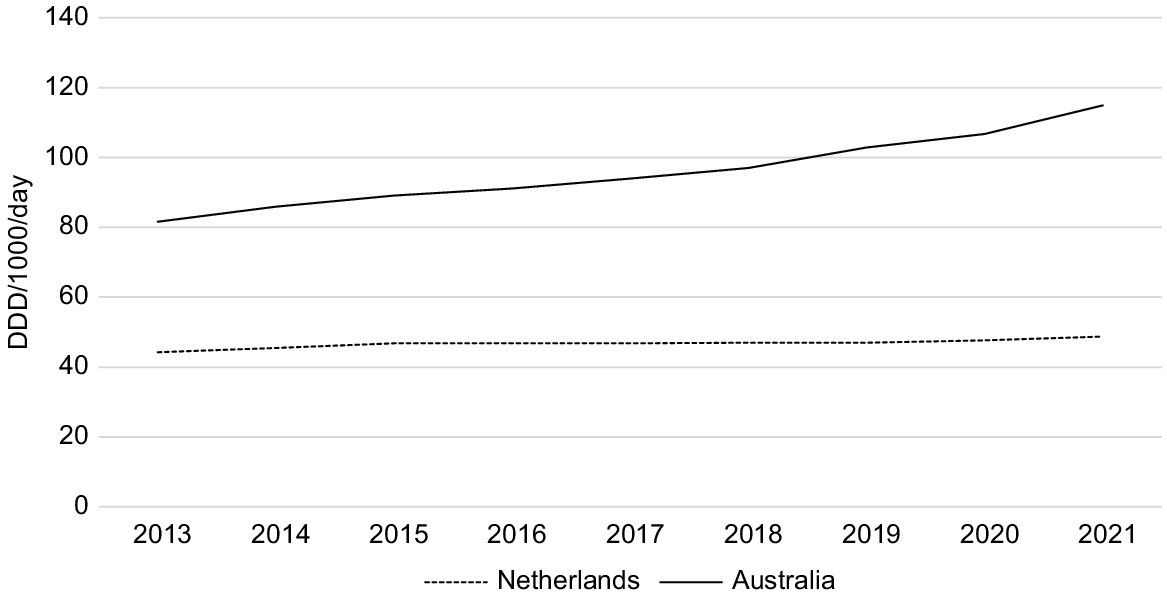
In 2013, antidepressant dispensing rates in Australia were nearly twice as high as those in the Netherlands (82.5 versus 44.3 DDD/1000/day) and increased to be more than twice as high by 2021 (115.6 versus 48.8 DDD/1000/day). Antidepressant dispensing increased by 40% in Australia over the nine study years, but by only 10% in the Netherlands. Our scan of the literature confirms that while population factors, health system structure, and clinical guideline recommendations are largely consistent across the two countries, a multifaceted approach in the Netherlands involving improved access to non-pharmacological alternatives, initiatives targeting safer antidepressant prescribing, and tight regulation of pharmaceutical industry influence on prescribers, has successfully curtailed increasing antidepressant use.
Australia may learn from the Netherlands’ approach to redress increasing antidepressant use.
Keywords: antidepressant, Australia, clinical guidelines, drug utilisation, general practice, Netherlands, pharmacoepidemiology, policy, prescribing behaviour, quality use of medicines, quantitative research.
Introduction
There is international concern about increasing antidepressant use, the increase due largely to increasing long-term use with known adverse effects and risks. In Australia, around one in seven adults is now taking antidepressants (Cochrane Australia 2021). In 2019, Australia had the fourth highest antidepressant consumption (defined by the daily dose per 1000 people per day) among the member countries of the Organisation for Economic Co-operation and Development, while the Netherlands ranked amongst the lowest (OECDiLibrary 2021). In 2020, Australia with a population of 25.7 million spent A$184 million on antidepressant drugs (A$7.16 per person) (Australian Institute of Health and Welfare 2020), while the Netherlands with a population of 17.4 million spent only A$62.4 million (A$3.59 per person) (Dutch National Healthcare Institute 2020).
It is not clear why there is such discrepancy between the two countries in antidepressant use. Australia and the Netherlands, although geographically distant, share common characteristics as high-income countries with aging populations. Both countries have well-established socialised healthcare systems and advanced mental health services. Both countries spend around 10% of their Gross Domestic Product on health care. Both countries have government-subsidised prescription medicine schemes. The healthcare systems in both countries include a primary and secondary care structure that allows patients to select their preferred healthcare providers (Tikkanen et al. 2020). Moreover, in both countries, most antidepressants are prescribed in general practice (Mcmanus et al. 2003; Gardarsdottir et al. 2007). In Australia, a thematic analysis of patient responses highlighted five central themes; depression, medication, healthcare system, psychosocial, and financial, which inform suggestions for addressing antidepressant deprescribing in clinical environments (Coe et al. 2023).
This study sought to compare trends in antidepressant dispensing in Australia and the Netherlands over the 9-year period from 2013 to 2021, and to explore contextual factors that may explain any observed differences.
Methods
Study design and data sources
This research used a convergent mixed methods approach including retrospective analysis of dispensing data obtained from public domain sources and a search of literature and websites to compare factors influencing general practitioner (GP) prescribing including clinical guideline recommendations and regulation of pharmaceutical industry promotion to prescribers.
Data collection
Prescribing data were obtained from the Australian Pharmaceutical Benefits Scheme (PBS) and Repatriation Pharmaceutical Benefits Scheme (RPBS) (Australian Government Department of Health and Aged Care 2022) and the Dutch Foundation for Pharmaceutical Statistics (SFK) datasets (Foundation for Pharmaceutical Statistics 2023). Population data for both Australia and the Netherlands were sourced from the Australian Bureau of Statistics (Australian Bureau of Statistics 2023) and the Dutch Central Bureau for Statistics (Centraal Bureau voor de Statistiek 2023a). These population data sets were used to calculate rates of antidepressant dispensing per 1000 inhabitants.
We conducted a search of websites containing information about antidepressant prescribing guidelines and factors influencing antidepressant prescribing in both countries. We consulted organisational websites including, in Australia, the therapeutic guidelines by the Psychotropic Expert group (Therapeutic Guidelines 2023a), the Royal Australian and New Zealand College of Psychiatrist clinical practice guidelines (Andrews et al. 2018), the Therapeutic Goods Administration (Therapeutic Goods Administration 2020), and the Royal Australian College of General Practitioners (Royal Australian College of General Practitioners 2019); and, in the Netherlands, the Dutch Association of General Practitioners (NHG) (NHG-werkgroep Depressie 2019), the Royal Dutch Society for the Promotion of Pharmacy (KNMP), and the Dutch Psychiatric Association (NVvP) (Nederlandse Vereniging voor Psychiatrie 2023). We also manually searched for relevant literature in PubMed, Google, and Google Scholar databases (until August 2023). Published peer reviewed studies as well as grey literature, including blog posts and unpublished reports, were identified through the electronic search process.
Data analysis
The dispensing datasets were compared for 2013–2021, focusing on specific Anatomical Therapeutic Chemical (ATC) codes for antidepressants. The following categories were examined: all antidepressants (N06A), tricyclic antidepressants (TCAs) and non-selective monoamine reuptake inhibitors (N06AA), selective serotonin reuptake inhibitors (SSRIs) (N06AB), monoamine oxidase inhibitors (MAOI) (N06AF), and ‘Other antidepressants’ including mirtazapine, venlafaxine, desvenlafaxine, and duloxetine (N06AX).
To ensure comparability, the quantity of each dispensed drug was standardised using the defined daily dose (DDD) per 1000 inhabitants per day (DDD/1000/day) (World Health Organization 2023). The DDD corresponds to the average maintenance dose per day of the drug when used for its main indication in adults. For the Australian dataset, the DDD/1000/day was calculated using Date of Supply (DoS) reports between 2013 and 2021 (Australian Government Department of Health and Aged Care 2022). The calculation involved multiplying the number of prescriptions, drug mass, and average dispensed quantity by 1000. This value was then divided by the product of the DDD, population, and days in the year. In the Dutch dataset, the total DDDs per year per antidepressant were provided, and the Dutch DDD/1000/day was calculated by multiplying the DDD by 1000 and dividing it by the population and the number of days in the year. All statistical analyses were conducted using Microsoft Excel. Findings from the literature and website search were synthesised using a narrative summary.
To compare antidepressant dispensing data by age and sex, we used Australian Institute of Health and Welfare reported PBS/RPBS data (Australian Institute of Health and Welfare) and Dutch National Healthcare Institute data (Dutch National Healthcare Institute) for the most recently available year, 2020. The number of antidepressant users was divided by the total population for each demographic group. The 10 most dispensed antidepressants were identified by ranking all dispensed antidepressants in 2021 for both countries.
Results
Antidepressant dispensing
Antidepressant dispensing (DDD per 1000 population per day) was higher in Australia compared to the Netherlands for each study year as shown in Table 1. In 2013, antidepressant dispensing in Australia was 1.9 times higher than that in the Netherlands, and by 2021 had increased to be 2.4 times higher. Over the nine study years, antidepressant dispensing rates increased in both countries as shown in Fig. 1. In Australia, dispensing increased by 40.1% (from 82.5 to 115.6 DDD/1000/day), compared to only 10.2% in the Netherlands (from 44.3 to 48.8 DDD/1000/day). Antidepressant dispensing in Australia exhibited an average annual increase of 4.5% per year compared to only 1.1% per year in the Netherlands.
| DDD/1000/day | Total increase (%) | Average annual increase (%) | Proportion of all ADs (%) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2013 | 2021 | |||||
| All ADs | Australia | 82.5 | 86.7 | 89.9 | 91.8 | 94.8 | 97.6 | 103.6 | 107.2 | 115.6 | 40.1 | 4.5 | – | – | |
| Netherlands | 44.3 | 45.4 | 46.9 | 46.8 | 46.8 | 46.9 | 47.0 | 47.8 | 48.8 | 10.2 | 1.1 | – | – | ||
| SSRI | Australia | 48.1 | 50.1 | 52.0 | 53.3 | 55.4 | 57.6 | 61.7 | 64.7 | 70.4 | 46.4 | 5.2 | 58.0 | 61.0 | |
| Netherlands | 27.8 | 28.5 | 29.5 | 29.5 | 29.5 | 29.8 | 30.0 | 30.8 | 31.7 | 14.0 | 1.6 | 63.0 | 66.0 | ||
| NSMRI and TCA | Australia | 5.6 | 5.6 | 5.6 | 5.5 | 5.5 | 5.5 | 5.8 | 5.8 | 6.1 | 8.9 | 1.0 | 6.8 | 5.3 | |
| Netherlands | 5.4 | 5.5 | 5.7 | 5.7 | 5.7 | 5.6 | 5.6 | 5.6 | 5.7 | 5.6 | 0.6 | 12.0 | 12.0 | ||
| MAOI | Australia | 0.9 | 0.8 | 0.8 | 0.8 | 0.7 | 0.7 | 0.7 | 0.6 | 0.6 | −33.3 | −3.7 | 1.1 | 0.5 | |
| Netherlands | 0.5 | 0.6 | 0.6 | 0.6 | 0.6 | 0.6 | 0.6 | 0.6 | 0.6 | 20.0 | 2.2 | 1.2 | 1.1 | ||
| Other ADs including SNRIs | Australia | 27.9 | 30.2 | 31.5 | 32.2 | 33.2 | 33.8 | 35.4 | 36.1 | 38.5 | 38.0 | 4.2 | 34.0 | 33.0 | |
| Netherlands | 10.6 | 10.8 | 11.1 | 11.0 | 11.0 | 10.9 | 10.8 | 10.8 | 10.9 | 2.8 | 0.3 | 24.0 | 23.0 | ||
AD, antidepressant; DDD, defined daily dose; SSRI, selective serotonin reuptake inhibitor; SNRI, serotonin and norepinephrine reuptake inhibitor; NSMRI, non-selective monoamine reuptake inhibitor; TCA, tricyclic antidepressant; MAOI, monoamine oxidase inhibitor.
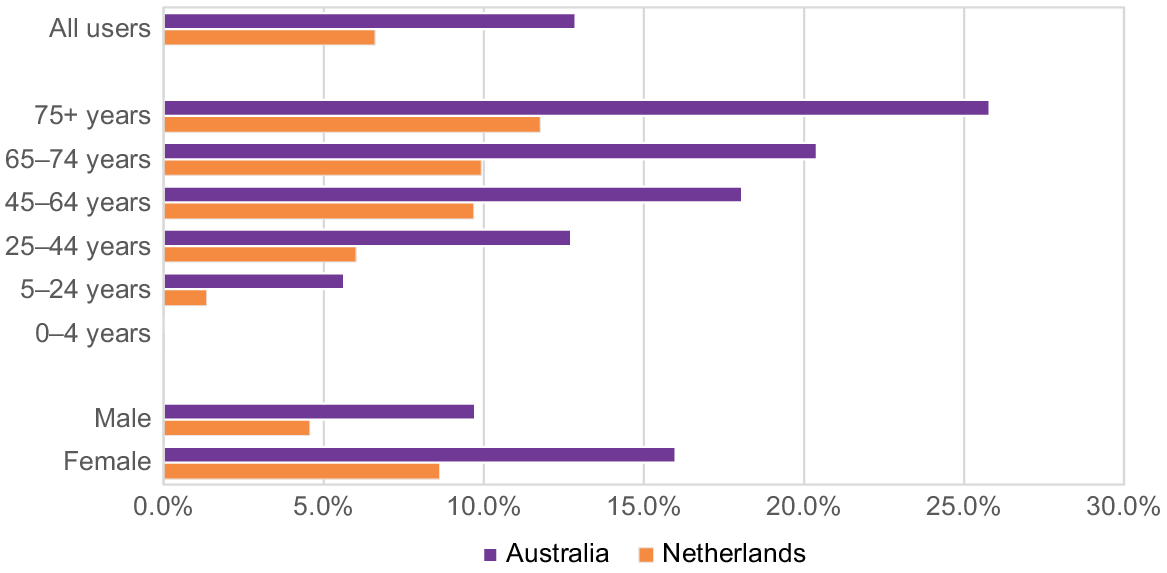
In both countries, antidepressant dispensing was about 50% higher for women than men (16.0% for women versus 9.7% for men in Australia, and 8.6% versus 4.6% in the Netherlands) (Fig. 2). As shown in Fig. 2, antidepressant dispensing increased with age in both countries. In Australia, antidepressant dispensing reached a peak of 25.8% for people aged 75 years or older from 2020 to 2021, compared to 11.8% in the same age group in the Netherlands.
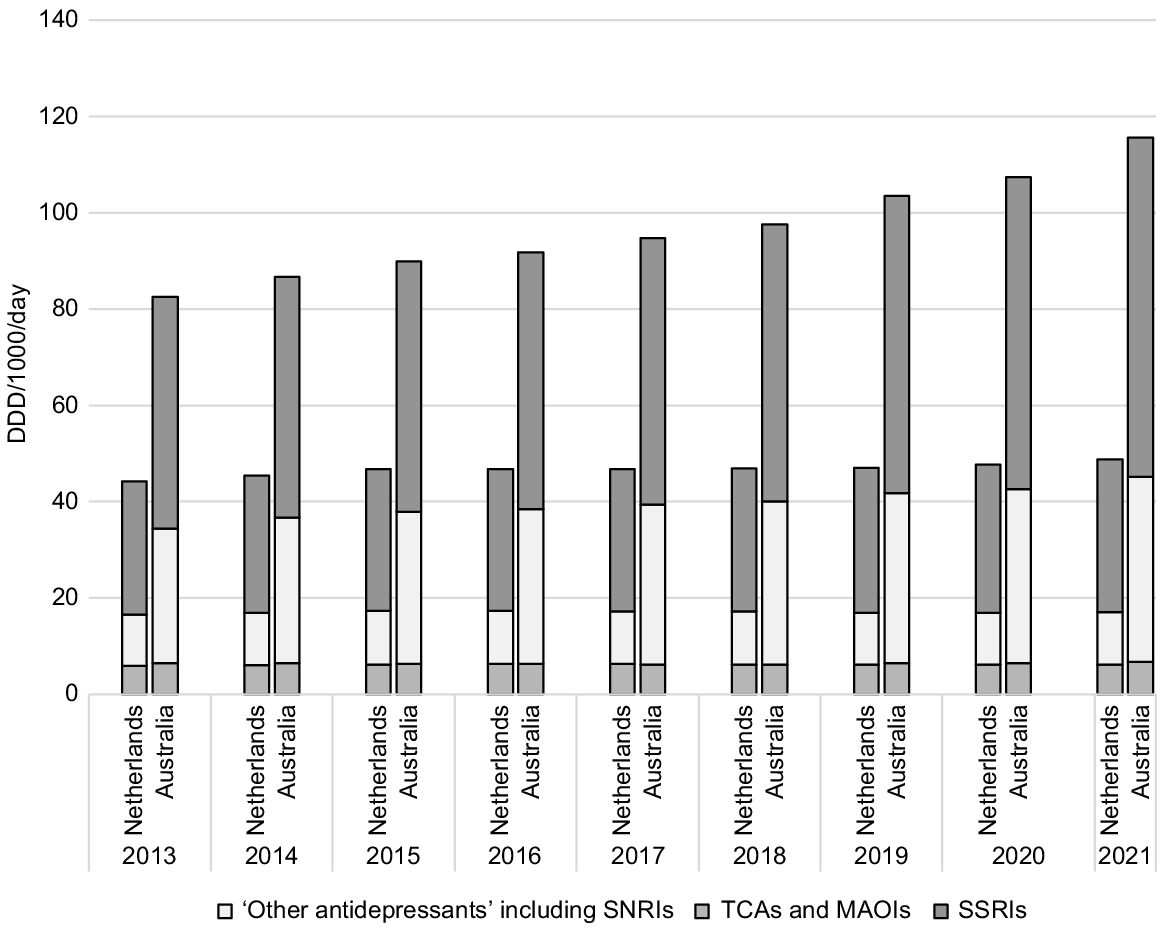
In both countries, SSRIs were the most dispensed antidepressants (Table 1, Fig. 3). For 2021, SSRIs accounted for 61.0% and 66.0% of all dispensed antidepressants in Australia and the Netherlands respectively. The 10 most dispensed antidepressants for both countries from 2013 to 2021 (DDD per 1000 people per day) are shown in Fig. 4. In 2021, these 10 antidepressants accounted for 97% of all dispensed antidepressants in Australia and 92% in the Netherlands. Nine of the 10 antidepressants were the same for both countries. Desvenlafaxine was not available in the Netherlands during the study period accounting for the only difference.
Dispensed antidepressant (DDD/1000 population/day) by type in Australia and the Netherlands, 2013–2021.
Top 10 most dispensed antidepressants (DDD/1000 population/day) in Australia and the Netherlands, 2013–2021.
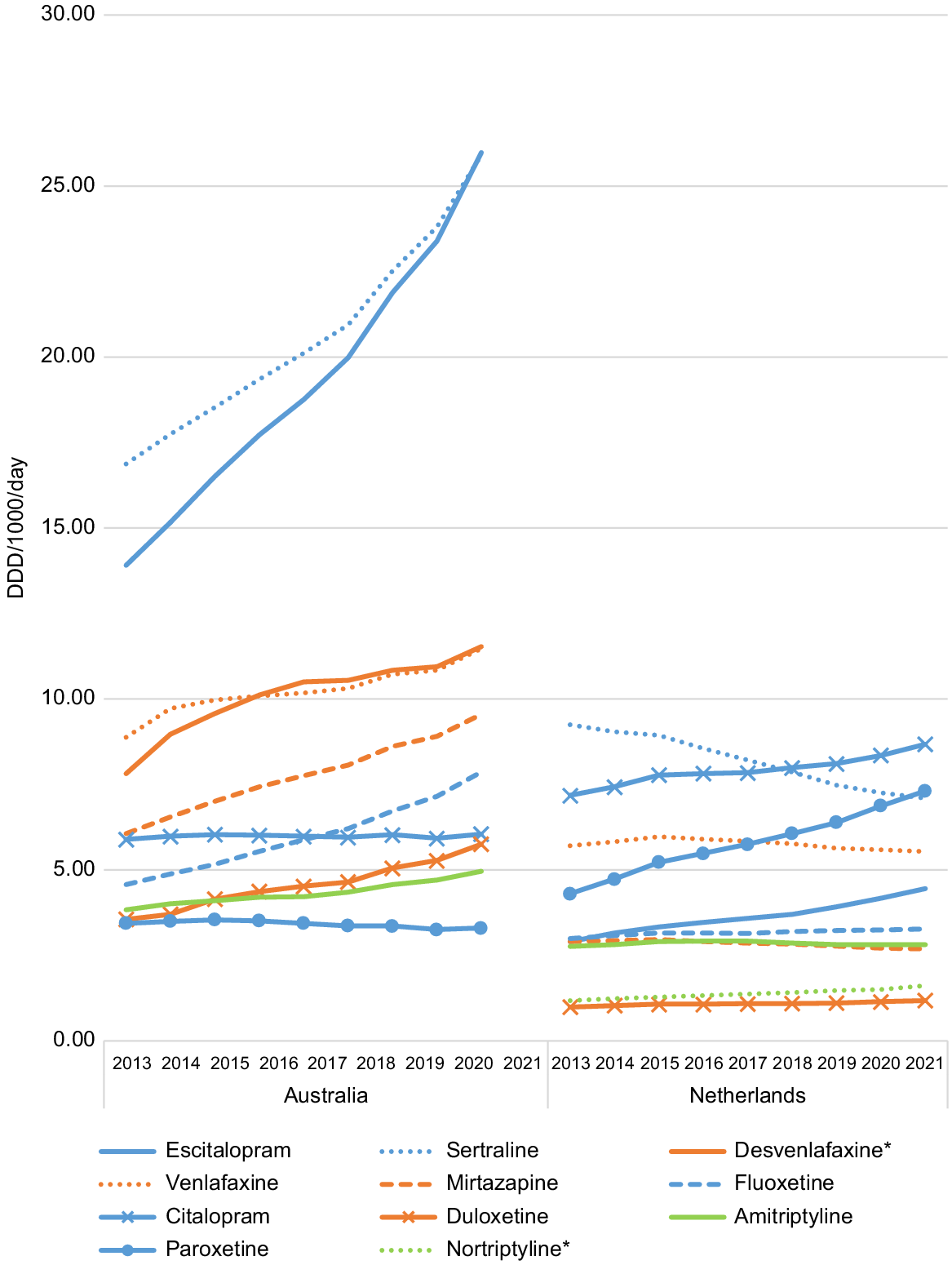
In Australia, escitalopram and sertraline dispensing increased dramatically over the nine study years; escitalopram dispensing increased by 78% (from 14.6 DDD/1000/day to 26.0 DDD/1000/day) and sertraline dispensing by 46.3% (from 17.7 DDD/1000/day to 25.9 DDD/1000/day).
Contextual factors that may influence GP prescribing of antidepressants
The mean age of the population is slightly higher in the Netherlands compared to Australia (42.3 versus 37 years), and the proportion of women in the population is slightly lower (50.2% versus 51.2%) (Australian Bureau of Statistics 2020; Centraal Bureau voor de Statistiek 2023b).
Rates of anxiety and depression are comparable (Australian Bureau of Statistics 2020-21; Centraal Bureau voor de Statistiek 2023a). Both countries enjoy relatively high levels of happiness. The Netherlands ranked 5th and Australia 12th out of 149 countries in the 2023 global happiness rankings (Rowan 2023). Unadjusted unemployment rates were comparable in 2023, at 3.5% in the Netherlands and 3.6% in Australia (Unemployment Rate 2023). Divorce rates were also comparable, at 1.7 and 1.9 per 1000 people in the Netherlands and Australia, respectively (World Population Review 2023).
The health systems of Australia and the Netherlands are comparable. Both countries have well-established primary care systems with GPs generating most antidepressant prescriptions and acting as gatekeepers to psychological therapy or specialist care.
In the Netherlands, there are no out of pocket costs for people to consult a GP (Hansen et al. 2022). In the Netherlands, in 2008 financial support was introduced for GPs to hire mental health nurses (Magnée et al. 2018). Subsequently, mental health nurses have been progressively integrated into Dutch general practice (Abidi et al. 2019). Today, more than 80% of GP practices have an affiliated mental health nurse (Magnée et al. 2016). The mental health nurses offer psychological therapy and conduct diagnostic assessments including psychological and social assessments at no cost to the patient (Magnée et al. 2018; Hansen et al. 2022).
In Australia, GPs are the first point of contact. Some GPs are bulk billing such that there is no out of pocket cost for patients, but for most patients there is a cost to consult a GP. The GPs can refer patients for psychological therapy on a mental health treatment plan (Jorm et al. 2005). This plan enables therapists to claim MBS, but there is still often out of pocket costs for the patient which can be up to A$90. Regardless of cost, access to therapists can be challenging, in particular for patients in rural Australia.
In both countries, there is a cost to patients for medication. In the Netherlands, the maximum personal contribution for medication is €385 euros per year (Wammes et al. 2020). In Australia, the patient contributes a co-payment for prescription medicines indexed annually up to A$42.50 per prescription, reduced to A$6.80 for concession card holders (NPS MedicineWise 2022).
In both countries, clinical guidelines recommend lifestyle interventions and psychological therapy as first-line treatment for mild and moderate depression and, for major depressive disorder, antidepressants with SSRIs as first choice antidepressant (NHG-werkgroep Depressie 2019; Therapeutic Guidelines 2023a). Guidelines in both countries recommend psychosocial interventions as first-line for generalised anxiety disorder (NHG-werkgroep Depressie 2019; Therapeutic Guidelines 2023a) .
In the Netherlands, guidelines recommend continuing treatment for 6 months beyond remission of symptoms and for at least 1 year in case of recurrent depression (NHG-werkgroep Depressie 2019). In Australia, guidelines recommend medication for 6–12 months for a single episode of major depression (Malhi et al. 2021; Therapeutic Guidelines 2023a).
In the Netherlands, guidelines recommend that long-term antidepressant therapy could be useful after three episodes of major depression or one severe major depression, and that mindfulness-based cognitive therapy is equally effective for relapse prevention (NHG-werkgroep Depressie 2019). Australian guidelines recommend that if a patient experiences two or more depressive episodes within a 5-year period, has a total of three or more depressive episodes overall, suffers from psychotic depression, or has made a serious suicide attempt, the continuation of antidepressant therapy should be for a period of 3 to 5 years. In some instances, lifelong therapy may even be suggested (Therapeutic Guidelines 2023a).
In the Netherlands, there are antidepressant drug-specific protocols to guide the tapering process (Horix et al. 2019). In 2018, a joint effort between the Dutch College of General Practitioners, the Royal Dutch Pharmacists Association, the Dutch Association for Psychiatry, and the patient organisation MIND led to the development of multidisciplinary guidelines for discontinuing SSRIs and SNRIs. These guidelines advocate for a hyperbolic dose reduction strategy (Horix et al. 2019). There is also the non-profit organisation Cinderella Therapeutics for personalised tapering strips (Kendrick 2021). In Australia, clinical guidelines recommend stopping antidepressants by decreasing the dosage by 25–50% every 1–4 weeks until reaching half of the smallest unit dose, which is then sustained for 2 weeks before stopping (Therapeutic Guidelines 2023b). There are no antidepressant drug-specific tapering protocols, and the requisite drug mini-doses are not readily available (Wallis et al. 2021). Drug mini-doses are available via compounding pharmacies but the expense can be prohibitive (Wallis et al. 2023).
The Netherlands has made concerted efforts over the past 15 years to curtail increasing antidepressant use (Ruhe et al. 2020). These efforts have involved targeted education on antidepressant prescribing, enhanced accessibility to non-pharmaceutical alternatives, regulation of pharmaceutical marketing to prescribers, development of multidisciplinary clinical guidelines, and integration of specialised mental health practitioners into general practice (Magnée et al. 2022). There has been no comparable approach in Australia. However, Australia is conducting research to address the escalating use of antidepressants (Coe et al. 2022; McDonald et al. 2023; Wallis et al. 2023).
In the Netherlands, promoting prescription medicines to the public is not allowed and promotion to doctors is strictly controlled. Gifts to GPs in the form of money, services, and goods are strictly forbidden (Stichting CGR 2023).
In Australia direct-to-consumer advertising for prescription drugs to the public is also not allowed, although promotion to GPs is permitted (Australian Medical Association 2018). While direct to consumer advertising is banned, the Code of Conduct of Medicines Australia (previously the Australian Pharmaceutical Manufacturers Association) that regulates direct to consumer advertising has several loopholes allowing companies to subvert the ban by, for example, funding disease awareness campaigns (Medicines Australia 2020). Awareness campaigns help to grow public awareness of conditions and increase acceptance of pharmaceutical solutions even when non-pharmacological alternatives, such as counselling or lifestyle adjustments, are recommended as first line and are equally or more effective (Greenslit and Kaptchuk 2012).
In Australia, pharmaceutical companies incentivise GP prescribing behaviour through gifts, travel offers, and other inducements (McNeill et al. 2006). There are an average of 608 industry-sponsored clinician events per week (Fabbri et al. 2017). During a 4-year period from 2011 to 2015, there were nearly 3.5 million participations at more than 116 000 pharmaceutical company sponsored medical education events (Fabbri et al. 2017). The pharmaceutical industry also pays for practitioners to serve as ‘key opinion leaders’ (Mintzes 2021). These strategies combined are proven to be effective for influencing prescribing (Donovan 1999).
Discussion
To our knowledge, this is the first study to examine and compare trends in antidepressant dispensing in Australia and the Netherlands and explore reasons for differences. Findings confirm that antidepressant dispensing is higher in Australia and increasing at a greater rate. In both countries, antidepressant dispensing was higher in women than men, and increased with age; and SSRIs were the most dispensed antidepressants consistent with earlier research (Huijbregts et al. 2017; de Oliveira Costa et al. 2023).
Higher antidepressant use in Australia cannot be explained by sociodemographic or health system factors. Identified differences between the countries that may help to explain the difference in antidepressant use include that in the Netherlands there is funding for mental health nurses in general practice, free psychological therapy, and detailed clinical guidance on tapering and stopping antidepressant use, complemented by resources such as tapering protocols and strips. Other notable between country differences include initiatives targeting safer antidepressant prescribing in the Netherlands and tight regulation of pharmaceutical industry influence on the public and on prescribers. This is important since it is well known that pharmaceutical industry marketing and promotion drive GP prescribing decisions and patient treatment expectations (Moynihan 1998; Davari et al. 2018).
In the Netherlands, mental health nursing education is thorough and emphasises holistic patient care. After their general nursing program, individuals pursuing a mental health specialisation in the Netherlands undergo extended post-graduate training, in contrast to many countries where psychiatric nursing specialisation is typically a year-long program (Stegge 2004). This training merges theoretical knowledge with practical experience, preparing nurses for varied clinical scenarios. Adopting aspects of Dutch mental health training could help Australian nurses develop better patient-centred training approaches. Additionally, exchange programs between the two nations could promote shared knowledge and a broader understanding of global mental health practices.
Limitations of this study include that the analysis relied on aggregated data from national databases, which may not capture individual patient characteristics or provide detailed clinical information. These data represent dispensed medication which may differ from prescribed medication and medication taken by the patient, although there is no reason to suspect that these factors would be different between the two countries. Also, we encountered limitation in accessing data on the duration of antidepressant usage for both countries, which may affect the insights into the observed disparities. Additionally, our scan of the literature and websites is susceptible to bias.
Conclusion
Findings from this cross-country comparison could be used to inform policy decisions in Australia targeted at redressing increasing antidepressant use to improve primary mental health care and outcomes for patients. The Netherlands provides a template for success. Factors contributing to this success include improved access to non-pharmacological therapy, clinical guidance and resources to support antidepressant cessation, funding for initiatives targeting safer antidepressant prescribing, and tight regulation of pharmaceutical industry influence on the public and prescribers.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Acknowledgements
The authors thank the Australian Government Department of Health and the Dutch Foundation for Pharmaceutical Statistics for providing freely accessible data on medicine dispensing.
References
Abidi L, Oenema A, Verhaak P, Tan FES, van de Mheen D (2019) The introduction of the practice nurse mental health in general practices in the Netherlands: effects on number of diagnoses of chronic and acute alcohol abuse. BMC Family Practice 20, 48.
| Crossref | Google Scholar |
Andrews G, Bell C, Boyce P, Gale C, Lampe L, Marwat O, Rapee R, Wilkins G (2018) Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for the treatment of panic disorder, social anxiety disorder and generalised anxiety disorder. Australian & New Zealand Journal of Psychiatry 52, 1109-1172.
| Crossref | Google Scholar |
Australian Bureau of Statistics (2020) Twenty years of population change. Available at https://www.abs.gov.au/articles/twenty-years-population-change
Australian Bureau of Statistics (2020-21) National study of mental health and wellbeing. Available at https://www.abs.gov.au/statistics/health/mental-health/national-study-mental-health-and-wellbeing/latest-release [Accessed 17 July 2023]
Australian Bureau of Statistics (2023) Population. Available at https://www.abs.gov.au/statistics/people/population [Accessed 23 April 2023]
Australian Government Department of Health and Aged Care (2022) PBS and RPBS Section 85 Date of Supply Data. Available at https://www.pbs.gov.au/info/statistics/dos-and-dop/dos-and-dop
Australian Institute of Health and Welfare (2020) Expenditure on mental health services. Available at https://www.aihw.gov.au/reports/mental-health-services/mental-health-services-in-australia/report-contents/expenditure-on-mental-health-related-services
Australian Medical Association (2018) Doctors’ relationships with industry. Available at https://www.ama.com.au/position-statement/doctors-relationships-industry-2018 [Accessed 30 August 2023]
Centraal Bureau voor de Statistiek (2023a) Population, households and population dynamics; from 1899. Available at https://www.cbs.nl/en-gb/figures/detail/37556eng [Accessed 23 April 2023]
Centraal Bureau voor de Statistiek (2023b) Age distribution. Available at https://www.cbs.nl/en-gb/visualisations/dashboard-population/age/age-distribution
Cochrane Australia (2021) New Cochrane review explores the latest evidence on approaches to stopping long term antidepressants. Available at https://australia.cochrane.org/news/new-cochrane-review-explores-latest-evidence-approaches-stopping-long-term-antidepressants
Coe A, Gunn J, Kaylor-Hughes C (2022) General practice patients’ experiences and perceptions of the WiserAD structured web-based support tool for antidepressant deprescribing: protocol for a mixed methods case study with realist evaluation. JMIR Research Protocols 11, e42526.
| Crossref | Google Scholar | PubMed |
Coe A, Gunn J, Fletcher S, Murray E, Kaylor-Hughes C (2023) Self-reported reasons for reducing or stopping antidepressant medications in primary care: thematic analysis of the diamond longitudinal study. Primary Health Care Research & Development 24, e16.
| Crossref | Google Scholar | PubMed |
Davari M, Khorasani E, Tigabu BM (2018) Factors influencing prescribing decisions of physicians: a review. Ethiopian Journal of Health Sciences 28, 795-804.
| Crossref | Google Scholar |
de Oliveira Costa J, Gillies MB, Schaffer AL, Peiris D, Zoega H, Pearson S-A (2023) Changes in antidepressant use in Australia: a nationwide analysis (2015–2021). Australian & New Zealand Journal of Psychiatry 57, 49-57.
| Crossref | Google Scholar | PubMed |
Donovan J (1999) Advertising pharmaceuticals to Australians. Australian Prescriber 22, 74-75.
| Crossref | Google Scholar |
Dutch National Healthcare Institute (2020) Reimbursment for ATC-subgroup N06A 2016-2020: Antidepressiva | GIPdatabank.nl. Available at https://www.gipdatabank.nl/databank?infotype=g&label=00-totaal&tabel_g_00-totaal=B_01-basis&tabel_h_00-totaal=B_01-basis&geg=vg&spec=&item=N06A
Fabbri A, Grundy Q, Mintzes B, Swandari S, Moynihan R, Walkom E, Bero LA (2017) A cross-sectional analysis of pharmaceutical industry-funded events for health professionals in Australia. BMJ Open 7, e016701.
| Crossref | Google Scholar | PubMed |
Foundation for Pharmaceutical Statistics (2023) Foundation for pharmaceutical statistics – SFK website. Available at https://www.sfk.nl/english/foundation-for-pharmaceutical-statistics [Accessed 23 April 2023]
Gardarsdottir H, Heerdink ER, van Dijk L, Egberts ACG (2007) Indications for antidepressant drug prescribing in general practice in the Netherlands. Journal of Affective Disorders 98, 109-115.
| Crossref | Google Scholar | PubMed |
Greenslit NP, Kaptchuk TJ (2012) Antidepressants and advertising: psychopharmaceuticals in crisis. The Yale Journal of Biology and Medicine 85, 153-158.
| Google Scholar | PubMed |
Hansen AB, Baste V, Hetlevik Ø, Smith-Sivertsen T, Haukenes I, de Beurs D, Nielen M, Ruths S (2022) Comparison of depression care provided in general practice in Norway and the Netherlands: registry-based cohort study (The Norwegian GP-DEP study). BMC Health Services Research 22, 1494.
| Crossref | Google Scholar | PubMed |
Huijbregts KM, Hoogendoorn AW, Slottje P, van Balkom AJLM, Batelaan NM (2017) Long-term and short-term antidepressant use in general practice: data from a large cohort in the Netherlands. Psychotherapy and Psychosomatics 86, 362-369.
| Crossref | Google Scholar | PubMed |
Jorm AF, Nakane Y, Christensen H, Yoshioka K, Griffiths KM, Wata Y (2005) Public beliefs about treatment and outcome of mental disorders: a comparison of Australia and Japan. BMC Medicine 3, 12.
| Crossref | Google Scholar | PubMed |
Kendrick T (2021) Strategies to reduce use of antidepressants. British Journal of Clinical Pharmacology 87, 23-33.
| Crossref | Google Scholar | PubMed |
Magnée T, de Beurs DP, De Bakker DH, Verhaak PF (2016) Consultations in general practices with and without mental health nurses: an observational study from 2010 to 2014. BMJ Open 6, e011579.
| Crossref | Google Scholar | PubMed |
Magnée T, de Beurs DP, Schellevis FG, Verhaak PF (2018) Antidepressant prescriptions and mental health nurses: an observational study in Dutch general practice from 2011 to 2015. Scandinavian Journal of Primary Health Care 36, 47-55.
| Crossref | Google Scholar | PubMed |
Magnée T, Stroo M, Kager C, Hek K (2022) Zet de POH-ggz in bij chronisch medicatiegebruik. Huisarts en wetenschap 65, 29-37.
| Crossref | Google Scholar |
Malhi GS, Bell E, Bassett D, Boyce P, Bryant R, Hazell P, Hopwood M, Lyndon B, Mulder R, Porter R, Singh AB, Murray G (2021) The 2020 Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for mood disorders. Australian & New Zealand Journal of Psychiatry 55, 7-117.
| Crossref | Google Scholar | PubMed |
McDonald S, Wallis KA, Horowitz M, Mann E, Le V, Donald M (2023) Acceptability and optimisation of resources to support antidepressant cessation: a qualitative think-aloud study with patients. British Journal of General Practice
| Crossref | Google Scholar |
Mcmanus P, Mant A, Mitchell P, Britt H, Dudley J (2003) Use of antidepressants by general practitioners and psychiatrists in Australia. Australian & New Zealand Journal of Psychiatry 37, 184-189.
| Crossref | Google Scholar | PubMed |
McNeill PM, Kerridge IH, Henry DA, Stokes B, Hill SR, Newby D, Macdonald GJ, Day RO, Maguire J, Henderson KM (2006) Giving and receiving of gifts between pharmaceutical companies and medical specialists in Australia. Internal Medicine Journal 36, 571-578.
| Crossref | Google Scholar | PubMed |
Medicines Australia (2020) Code of Conduct. 19th edn. Adopted 26 November 2019. Effective 30 March 2020. Available at https://www.medicinesaustralia.com.au/wp-content/uploads/sites/65/2022/11/20221103-PUB-Edition-19-FINAL-VERSION-2.pdf [Accessed 30 August 2023]
Mintzes B (2021) Policing the promotion of prescription medicines–the new Medicines Australia Code of Conduct. Australian Prescriber 44, 4-5.
| Crossref | Google Scholar | PubMed |
Nederlandse Vereniging voor Psychiatrie (2023) Available at https://www.nvvp.net/home [Accessed 2023]
NHG-werkgroep Depressie (2019) Depressie | NHG-Richtlijnen. Available at https://richtlijnen.nhg.org/standaarden/depressie [Accessed 23 April 2023]
NPS MedicineWise (2022) Medicine costs: how to reduce them. Available at https://www.nps.org.au/consumers/keeping-your-medicines-costs-down
OECDiLibrary (2021) OECD health statistics 2021. Available at https://www.oecd-ilibrary.org/sites/5689c05c-en/index.html?itemId=%2Fcontent%2Fcomponent%2F5689c05c-en
Rowan AN (2023) World happiness report 2023. WellBeing News 5, 1.
| Google Scholar |
Royal Australian College of General Practitioners (2019) Clinical guideline for the diagnosis and management of work-related mental health conditions in general practice. Available at https://www.racgp.org.au/FSDEDEV/media/documents/Clinical%20Resources/Guidelines/Mental%20health/Work-related-mental-health-conditions-in-general-practice.pdf
Ruhe HG, Horikx A, van Avendonk MJP, Groeneweg BF, Mulder H, Woutersen-Koch H (2020) [Discontinuation of SSRIs and SNRIs]. Nederlands tijdschrift voor geneeskunde 164, D4004 Available at http://europepmc.org/abstract/MED/32186829 [Accessed 10 February 2020].
| Google Scholar | PubMed |
Stegge GJ (2004) [Psychiatric training of nurses in the Netherlands since 1883]. Gewina 27, 78-99.
| Google Scholar | PubMed |
Stichting CGR (2023) Code of conduct – Dutch Medicines Act. Available at https://www.cgr.nl/en-GB/Gedragscode-Geneesmiddelenreclame
Therapeutic Goods Administration (2020) Product and consumer medicine information. Available at https://www.tga.gov.au/products/australian-register-therapeutic-goods-artg/consumer-medicines-information-cmi [Accessed 13 May 2023]
Therapeutic Guidelines (2023a) Psychotropic. Available at https://tgldcdp.tg.org.au/guideLine?guidelinePage=Psychotropic&frompage= [Accessed 13 May 2023]
Therapeutic Guidelines (2023b) Stopping an antidepressant. Available at https://tgldcdp.tg.org.au/viewTopic?etgAccess=true&guidelinePage=Psychotropic&topicfile=stopping-antidepressants [Accessed 24 July 2023]
Unemployment Rate (2023) Trading Economic, G20, Unemployment Rate. Available at https://tradingeconomics.com/country-list/unemployment-rate [Accessed 17 August 2023]
Wallis KA, Donald M, Moncrieff J (2021) Antidepressant prescribing in general practice: a call to action. Australian Journal of General Practice 50, 954-956.
| Crossref | Google Scholar | PubMed |
Wallis KA, Donald M, Horowitz M, Moncrieff J, Ware RS, Byrnes J, Thrift K, Cleetus MA, Panahi I, Zwar N, Morgan M, Freeman C, Scott I (2023) RELEASE (REdressing Long-tErm Antidepressant uSE): protocol for a 3-arm pragmatic cluster randomised controlled trial effectiveness-implementation hybrid type-1 in general practice. Trials 24, 615.
| Crossref | Google Scholar | PubMed |
Wammes J, Jeurissen P, Westert G, Tanke M (2020) The Dutch health care system. In ‘International profiles of health care systems’. (Eds R Tikkanen, R Osborn, The Commonwealth Fund, E Mossialos, A Djordjevic, G Wharton, London School of Economics and Political Science) p. 137. (The Commonwealth Fund)
World Health Organization (2023) Defined Daily Dose (DDD). Available at https://www.who.int/tools/atc-ddd-toolkit/about-ddd [Accessed 20 April 2023]
World Population Review (2023) Divorce rates by country 2023. Available at https://worldpopulationreview.com/country-rankings/divorce-rates-by-country [Accessed 17 August 2023]