Empowering our First Nations workforce: evaluation of a First Nations COVID-19 vaccination training program
Sean Cowley A * , Karina Baigrie A B , Katie Panaretto A C , Kelly Trudgen A , Vanessa Clements A , Oscar Whitehead D and Rica Lacey CA
B
C
D
Abstract
A COVID-19 vaccination training program was designed for Aboriginal and Torres Strait Islander (First Nations) health workers and practitioners in Queensland to expand their scope of practice to include COVID-19 immunisation. In the setting of a global pandemic, the project aimed to improve vaccination levels and show how First Nations staff are central to community-led responses to effectively address their community’s health needs.
The program, consisting of an online module and face to face workshop, is described and then evaluated with the RE–AIM framework via mixed methods of participant training surveys and qualitative feedback.
The program reached 738 online and 329 workshop participants with the majority identifying as First Nations. The 52 workshops were attended by participants from 12 different hospital and health services in Queensland and 13 Aboriginal Community Controlled Health Organisations (ACCHOs). Feedback was positive, with participants rating the training highly. Of the First Nations Health Workers and Practitioners who responded to the workshop follow up survey, the majority (34/40) implemented their new skills in practice helping minimise the impact of COVID-19 outbreaks in their community. Most respondents (38/40) considered vaccination should be permanently in their scope of practice.
The successful implementation of the vaccination training project was an example of First Nations led health care. Improving scope of practice for First Nations health staff can improve not just career retention and progression but also the delivery of primary care to a community that continues to bear the inequity of poorer health outcomes.
Keywords: Aboriginal and Torres Strait Islander, Aboriginal and Torres Strait Islander health practitioner, COVID-19, empower, evaluation, First Nations health workforce, immunisation, Indigenous health worker, RE–AIM, scope of practice, vaccination training.
Introduction
The COVID-19 pandemic continues to have wide ranging impacts on the community, the health system and those with living with chronic disease and other risk factors. The response of Aboriginal and Torres Strait Islander communities (hereafter referred to as First Nations) to the pandemic has been a world leading example of self-determination (Stanley et al. 2021). This was integral to the successful public health response that mitigated many of the anticipated consequences. However, First Nations people in Australia face ongoing health disparities and a higher burden of chronic disease which predispose to severe outcomes from COVID-19 (Doherty Institute 2021). Overcrowding remains prevalent in First Nations communities with up to 51% of those in remote areas living in houses with too few bedrooms (Australian Institute of Health and Welfare 2021), which exacerbates the risk of COVID-19 transmission. Distance from tertiary health care amplified fears about the predicted impact of COVID-19 within remote communities and demanded a rapid public health response.
The importance of vaccination to reduce severity of disease and lessen the need for more stringent public health measures was emphasised in pandemic modelling in Australia (Doherty Institute 2021). This created an urgency to maximise First Nations COVID-19 vaccination uptake. Whilst there are high childhood and influenza coverage rates for First Nations people (Department of Health and Aged Care 2022) it was anticipated that there would be moderate vaccine hesitancy due to the novel COVID-19 virus and vaccines in an ever-changing knowledge environment. Hence the First Nations health workforce was going to be vital to maximising vaccination coverage.
Many programs have demonstrated how effective First Nations heath workers and health practitioners can be in engaging and delivering care for their communities. This includes improving communication with patients, continuity of care and improving discharge against medical advice rates (Mackean et al. 2020). Recognition of their important role led to regulation of health practitioners under the Australian Health Practitioner Regulation Authority (Ahpra) in 2012. Despite Ahpra recognition, this workforce remained unable to work to a full scope of capacity due to state medicines regulations which rendered them unable to administer immunisations (Naren et al. 2021). This is compounded by poor role descriptions, ambivalent career pathways and lack of recognition from health colleagues (Wright et al. 2019).
Cognisant of these factors, the Office of First Nations Health partnered with the Cunningham Centre (Darling Downs Health) to develop the First Nations COVID-19 Vaccination Program (FNCVP). The aims of the program were first, to train health workers and practitioners to vaccinate against COVID-19; and second to increase knowledge of the COVID-19 vaccines so that all First Nations health staff could provide consistent advice to their communities. This paper reports on the development and evaluation of FNCVP in Queensland.
Setting
In Queensland, 237 000 people identify as Aboriginal and/or Torres Strait Islander which is 4.6% of the population (Australian Bureau of Statistics 2022). Within the state, 33.8% of First Nations people live in urban areas, 48.7% regional and 17% remote (Australian Bureau of Statistics 2016). Although most First Nations people live in urban and regional areas, in discreet remote communities the populations are predominantly First Nations – for example Cherbourg (96.4%) and Yarrabah (95.9%) (Australian Bureau of Statistics 2016).
To facilitate the rollout, Queensland Health issued a Public Health Emergency Order for COVID-19 vaccination which permitted First Nations health workers and practitioners in clinical positions to vaccinate on completion of mandated training (Queensland Government 2023). In April 2022 this order was extended to include administration of the influenza vaccine.
It was difficult to determine the exact number of the professions working clinically in Queensland – at the time of the training, there were 155 First Nations health practitioners registered in Queensland (Australian Health Practitioner Regulation Agency 2021). National data further estimate the numbers actually working in clinical roles – this is approximated at 70% in 2020 with the remainder 30% in non-clinical roles (Department of Health and Aged Care 2020). The clinical health practitioners are thought to be predominantly in the ACCHO sector with approximately three working in Queensland Health; anecdotally there are many more health workers in Queensland.
The FNCVP was rolled out whilst Queensland maintained an elimination public health strategy to COVID-19, with border restrictions in place in part to drive up vaccination coverage throughout much of 2021. The border restrictions were removed on 13 December 2021 once the state achieved a target of 80% fully vaccinated (Queensland Government 2021).
First Nations COVID-19 vaccination program
An expert steering committee, comprising public health physicians, nurses and First Nations health staff supported the design, rollout and review of the program. It was intended to complement the mandatory Commonwealth COVID-19 training modules health professionals were required to complete to administer COVID-19 vaccines.
The program was designed to enable this workforce to vaccinate safely and deliver health promotion regarding COVID-19 and its vaccines. Whilst the primary focus was to upskill health workers and practitioners, any interested health staff could complete the training. The online modules comprised an overview of First Nations health in Australia in relation to vaccine preventable diseases, with a focus on clinical features, disease management, vaccine development and the risks and benefits of vaccination for COVID-19 disease. An additional influenza module covered the clinical features and vaccines for influenza. The 1 day workshop covered how to receive, handle, administer and prepare COVID-19 vaccines. In Queensland, health workers and practitioners were required to complete the online modules prior to the workshop in order to vaccinate. Additionally, support to complete the Commonwealth COVID-19 training was facilitated. Final certification to vaccinate required the completion of both FNCVP and the Commonwealth training. After the workshops, onsite support and mentoring was provided where services requested this help, to integrate participants into their vaccination teams and clinics.
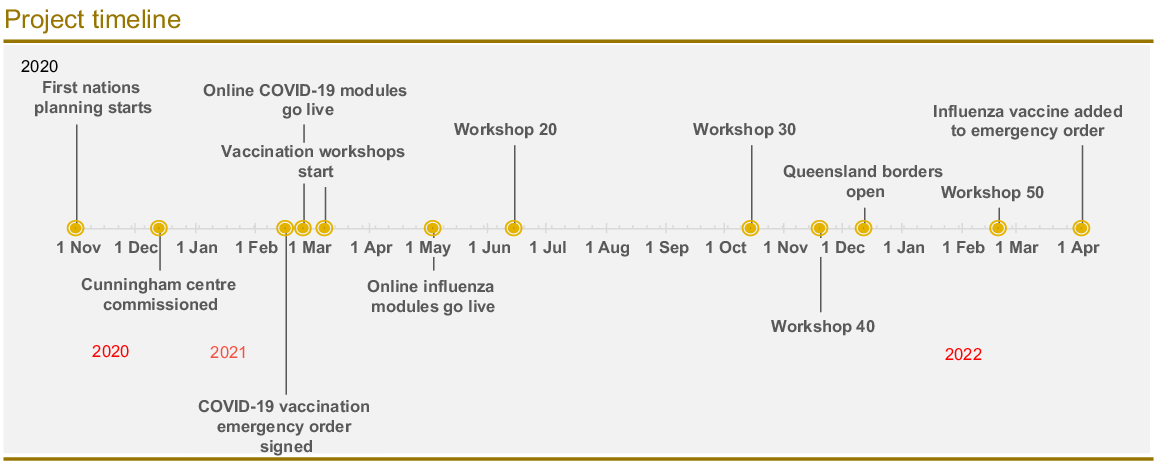
Workshops were held at the request of employing organisations, so many participants trained with their clinic teams. The workshops aimed to be a transformative learning environment, enabling reflection on the learning and discussion topics, with a strong focus on addressing vaccine hesitancy. Feedback from participants led to continuous improvement of the content and format. Frequent revision of Australian Technical Advisory Group on Immunisation (ATAGI) recommendations led to regular updates in the content. The training was promoted through Primary Health Networks, Public Health Units and ACCHOs. Fig. 1 shows the timeline of the project milestones.
Methods
This is a mixed methods paper which utilised evaluation data from participants of the online modules, workshops and qualitative feedback from workshop attendees. Participants were offered anonymous evaluation after the online modules (survey 1) and workshop (survey 2). Survey 1 had a 69.9% (516/738) response rate and survey 2 had a 77.8% (256/329) response rate. A final survey (survey 3) was offered via email to health workers and practitioners 4 months post the final workshop, which had a more limited response rate of 15.2 % (40/264). The surveys were a mix of Likert scale questions, binary questions and free text comments. The responses were aggregated and analysed in summary form, and free text responses collated and individually reviewed. See Supplementary material detailing the questions asked for each survey.
The program was evaluated using the RE–AIM framework, which is used to measure the public health impact of an intervention on five dimensions – Reach, Efficacy, Adoption, Implementation and Maintenance (Glasgow et al. 1999). Program reach and adoption was assessed by analysis of survey 1 and 2 in which data were collected on occupation, sector of employment and identification as First Nations. Efficacy was evaluated from feedback of the quality and utility of the training in survey 1 and 2. Implementation of the training was assessed by the proportion who reported administering COVID-19 vaccines in survey 3. Maintenance was assessed by survey 3 data regarding ongoing use of vaccination skills, and interest in other vaccinations was used to assess the longer-term potential of the project. Qualitative feedback of the views of workshop participants was collated during training. A formal qualitative tool was not used, so this was obtained via direct discussions and collation of ad hoc feedback during workshops that was summarised by the authors for this report. Personal communication received from ACCHOs to the authors was used to give examples of health workers and practitioners vaccinating in practice.
Results
It was a deadly experience and I was so glad I was afforded the opportunity. (First Nations Health Worker, Cherbourg Community)
The training was great; it gave me the skills I required to be able to go into my community and vaccinate my people against COVID-19. (Workshop attendee)
The FNCVP online modules had a high uptake with 738 people completing them, the majority identifying as First Nations (60.3%; 445/738). The breakdown of participants by occupation and sector of employment are shown in Tables 1 and 2. Feedback on the content of the modules was consistently high with participants acknowledging the content was easy to understand. The negatives were generally related to log-in and access issues. Subsequent to this feedback, more detailed instructions were provided to assist with registration. The workshops trained 329 people with the majority being health workers and practitioners (75.6%; 254/329).
Why now when we have not previously been supported for this type of training before? (Workshop participant)
| Occupation | Online modules | Workshops | |
|---|---|---|---|
| Aboriginal and Torres Strait Islander health practitioner | 11.5% (85) | 15.8% (52) | |
| Aboriginal and Torres Strait Islander health workers | 24.1% (178) | 64.4% (212) | |
| Others (e.g. nurse, doctor, allied health, managerial, administrative, operational and support staff) | 64.4% (475) | 19.8% (65) | |
| Total | 100% (738) | 100% (329) |
| Sector Employment | Online modules | Workshops | |
|---|---|---|---|
| Aboriginal Community Controlled Health Organisations (ACCHO) | 75.3% (556) | 46.8% (154) | |
| Queensland Health | 22.4% (165) | 52.9% (174) | |
| Others (e.g. private clinics) | 2.3% (17) | 0.3% (1) | |
| Total | 100% (738) | 100% (329) |
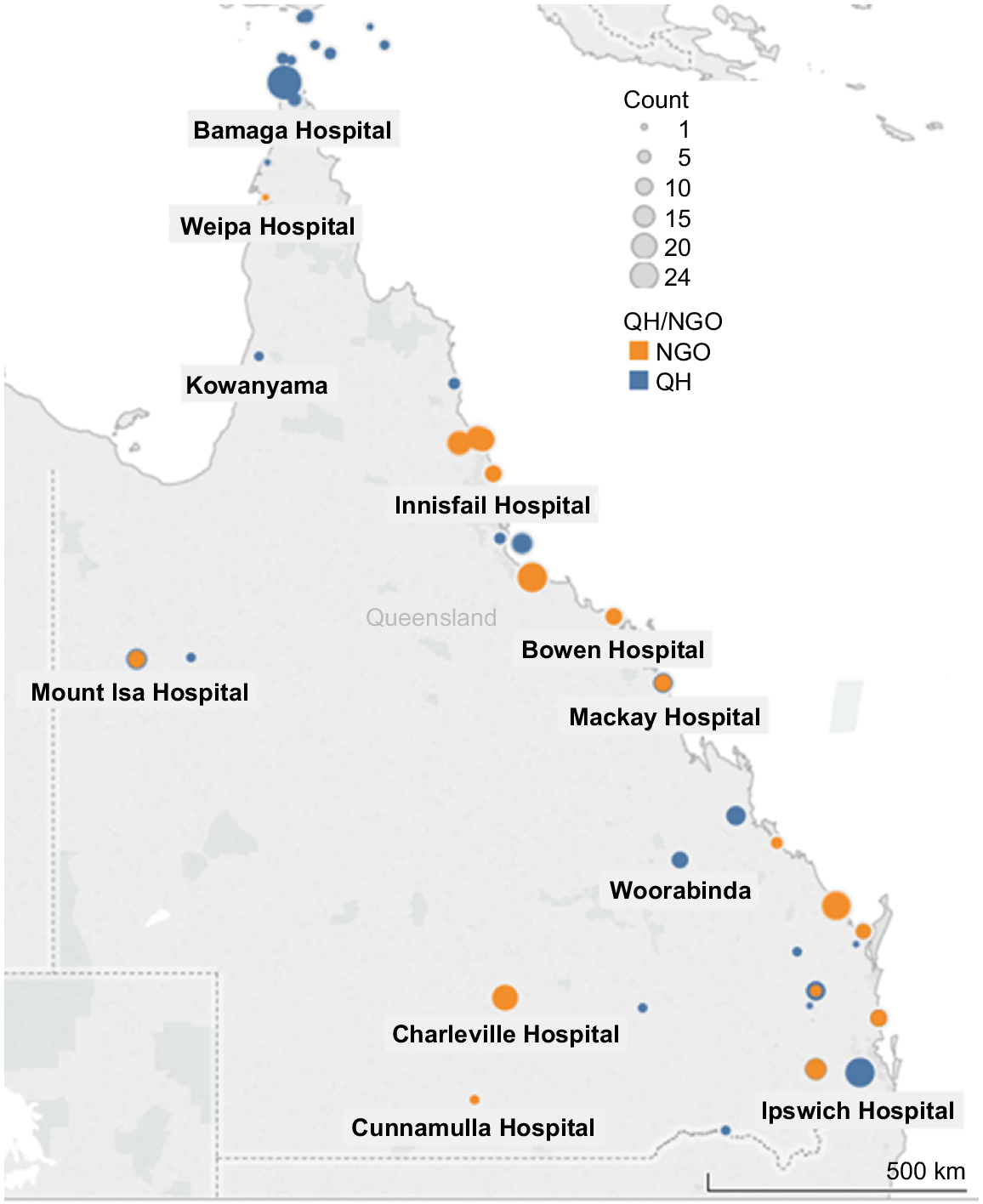
Initially there was some disbelief that the law had been changed to allow this workforce to vaccinate and strongly articulated hesitancy from participants reluctant to take on a clinical skill they could not continue beyond the cessation of the emergency order. This was expressed directly to authors at workshops and in discussions with services about participating in the FNCVP. It required some negotiation to moderate and a commitment to drive permanent change within the Office of First Nations Health. As the program rolled out, uptake was more than anticipated. Initially five workshops were commissioned; this expanded to 20 workshops completed by June 2022 and with extension of the project and an additional First Nations nurse, 52 workshops were held in less than 10 months to the end of January 2022. Fig. 2 shows the workshop locations and participant numbers.
Map of vaccine training workshops by participant number and employment sector. QH: Queensland Health; NGO: non-government organisation.
Health staff vaccine hesitancy noticeably lessened over the program. Over the year, a shift was seen in the thinking about the vaccine, with growing acceptance and uptake of vaccination by the workshop participants themselves. At the end of one workshop, an unvaccinated participant stated ‘I’m going to go home and talk to the family tonight. We need to have this vaccine’.
Workshops were rated good or better by 99.6% (255/256) of survey 2 respondents and 100% (256/256) valued the training as a useful skill in their employment. The majority of survey 3 respondents vaccinated in practice (34/40). There was strong interest in maintenance of vaccination skills and permanent scope of practice changes. In Queensland, the emergency orders for COVID-19 vaccination added influenza vaccine for the 2022 season; 42% (138/329) of FNCVP participants completed the extra module to enable them to deliver influenza vaccine. The trained staff joined many vaccine teams across the state. Box 1 provides examples of the translation of the training into practice in three First Nations vaccination clinics.
| Box 1.First Nations health practitioners and workers in action vaccinating their communities (personal communication from each service). |
| From August 2021 to May 2022: |
The main findings of the RE-AIM review are summarised in Box 2.
| Box 2.FNCVP RE-AIM evaluation summary. |
| Reach (the proportion of the target population that participates in the program) |
| Effectiveness (the success of the program) |
| Adoption (the proportion of settings that implemented the program) |
| Implementation (the extent to which the program was implemented as planned) |
| Maintenance (the extent which the program is sustained over time) |
Discussion
We are very important; we are the link between health services and our community. (Indigenous Health Worker, Cherbourg Community)
Program reach and adoption showed that the FNCVP tapped into a workforce ready to step up their clinical skills. The FNCVP provides evidence that vaccination (after appropriate training) is considered valuable knowledge by health workers and practitioners. Program implementation is demonstrated by the majority of respondents vaccinating in practice in survey 3 (34/40). There was a decrease in those who continued to vaccinate at the time of survey (18/40). Whilst this may represent a winding down of the COVID-19 vaccination rollout, other reasons for the participants not vaccinating cannot be excluded. Factors such as strong support from respondents for permanent scope of practice changes in Queensland and interest in further vaccination training support the longer-term maintenance of the program. There was a gap between those who felt they needed ongoing mentoring to maintain their skills (30/40) and those who received mentoring (21/40). This may have implications for future vaccination training programs to ensure staff are supported in the workplace.
With their mix of community knowledge and health skills, health workers and practitioners were integral to the vaccine rollout and management of COVID-19 disease in their communities. Not only did they vaccinate, but many were also involved in COVID-19 testing, contact tracing and risk assessment. This helped reduce the anticipated devastating impact of COVID-19 on the community in Queensland through 2022. Their hard work contributed to a first dose vaccine coverage of 73% in First Nations people by 15 December 2021 just after the border restrictions were removed and Omicron swept in (Department of Health and Aged Care 2021).
First Nations health professionals remain underrepresented in the health workforce and there are issues with both recruitment and retention, a situation that appears to be worsening (Taylor et al. 2020). Empowering and developing the First Nations workforce has been called for by many experts and the community to improve First Nations peoples’ health and self-determination for many years (Moodie et al. 2021). A sustainable workforce of First Nations health practitioners, with their ‘unique cultural, social and language skills’ (Taylor and Thompson 2019), will improve trust to access health care and will be more cost effective to the health system instead of relying on external staff (Zhao et al. 2019).
Initially there was workforce hesitancy from participants reluctant to take on a clinical skill they could not continue beyond the cessation of the emergency order. This led to a commitment from the Office of First Nations Health to seek permanent change in regulations to enable the professions to work to a full scope of practice in Queensland. Subsequent to this program, this has now occurred, with First Nations health workers and practitioners now permitted to administer a range of vaccines in Queensland following completion of relevant training (Queensland Government 2023).
Limitations
This review has several limitations. The unknown numbers of health workers and practitioners in Queensland impacted the planning and evaluation of the project. Our data suggest we trained 50% of known health practitioners in clinical roles in Queensland; the number of health workers is unknown. The feedback gained was subjective and qualitative which may introduce bias in the data and evaluation. Response rate to post-training survey 3 was low. This loss to follow up impacts on the ability to assess the implementation and longer-term maintenance of the training. We are unable to directly measure the numbers of participants who vaccinated or the quantity of vaccines given as the data are not available. The data does not enable quantification of the number of people that were provided education from participants, who later chose to be vaccinated for COVID-19. Consequently, the evaluation cannot directly measure the contribution to the overall COVID-19 vaccination coverage.
Conclusion
Having vaccination skills was very useful for me in my community; having vaccination permanently in the scope of practice for health practitioners would be beneficial for their community. (Workshop attendee)
The FNCVP was rolled out in a dynamic situation with expected vaccine hesitancy, community anxiety about biosecurity restrictions and pre-existing mistrust of government. It was strongly supported by First Nations health workers and practitioners. This program was not just a technical training exercise, but an example of First Nations centred and led health care which acknowledged them as integral clinical team members who possess broad skills in primary health. Supporting them with training, mentoring and career development is essential to empower the profession to work to its full scope of practice. Placing First Nations people central to their own communities’ health care will create a culturally safe health service and improve the continuity and effectiveness of the primary care we deliver.
Data availability
The data that support this study will be shared upon reasonable request to the corresponding author.
Acknowledgements
The authors acknowledge the contributions of Abdulla Suleman and Di Maurer (Office of First Nations Health, Queensland Health) for their support during the project and in the evaluation stage. Rachael Ham (Wuchopperen Health Service) and north Queensland ACCHOs are acknowledged for their support of the project.
References
Australian Bureau of Statistics (2016) Census of population and housing – counts of Aboriginal and Torres Strait Islander Australians. Available at https://www.abs.gov.au/statistics/people/aboriginal-and-torres-strait-islander-peoples/census-population-and-housing-counts-aboriginal-and-torres-strait-islander-australians/2016#counts-by-remoteness-area [Accessed 4 December 2022]
Australian Bureau of Statistics (2022) Queensland: Aboriginal and Torres Strait Islander population summary. Available at https://www.abs.gov.au/articles/queensland-aboriginal-and-torres-strait-islander-population-summary [Accessed 4 October 2022]
Australian Health Practitioner Regulation Agency (2021) Registration data table – 30 June 2021. Available at https://www.atsihealthpracticeboard.gov.au/About/Statistics.aspx
Australian Institute of Health and Welfare (2021) Aboriginal and Torres Strait Islander Health performance framework: measure 2.01 housing. Available at https://www.indigenoushpf.gov.au/measures/2-01-housing [Accessed 4 October 2022]
Department of Health and Aged Care (2020) Dashboard, allied health factsheets. Available at https://hwd.health.gov.au/resources/dashboards/nhwds-alld-factsheets.html [Accessed 19 December 2022]
Department of Health and Aged Care (2021) COVID-19 vaccination – geographic vaccination rates – SA4 indigenous population – 15 December 2021. Available at https://www.health.gov.au/resources/publications/covid-19-vaccination-geographic-vaccination-rates-sa4-indigenous-population-15-december-2021?language=en [Accessed 19 December 2022]
Department of Health and Aged Care (2022) Immunisation coverage rates for Aboriginal and Torres Strait Islander children. Available at https://www.health.gov.au/topics/immunisation/immunisation-data/childhood-immunisation-coverage/immunisation-coverage-rates-for-aboriginal-and-torres-strait-islander-children#:~:text=The%20national%20coverage%20rate%20for,2%20year%20olds%20is%2089.53%25 [Accessed 19 December 2022]
Doherty Institute (2021) Doherty modeling – final report to national cabinet. Melbourne, Victoria. Available at https://www.doherty.edu.au/uploads/content_doc/Synthesis_DohertyModelling_FinalReport__NatCab05Nov.pdf [Accessed 19 July 2022]
Glasgow RE, Vogt TM, Boles SM (1999) Evaluating the public health impact of health promotion interventions: the RE-AIM framework. American Journal of Public Health 89, 1322-1327.
| Crossref | Google Scholar | PubMed |
Mackean T, Withall E, Dwyer J, Wilson A (2020) Role of Aboriginal Health Workers and Liaison Officers in quality care in the Australian acute care setting: a systematic review. Australian Health Review 44, 427-433.
| Crossref | Google Scholar | PubMed |
Moodie N, Ward J, Dudgeon P, Adams K, Altman J, Casey D, Cripps K, Davis M, Derry K, Eades S, Faulkner S, Hunt J, Klein E, McDonnell S, Ring I, Sutherland S, Yap M (2021) Roadmap to recovery: reporting on a research taskforce supporting Indigenous responses to COVID-19 in Australia. Australian Journal of Social Issues 56, 4-16.
| Crossref | Google Scholar | PubMed |
Naren T, Burzacott J, West C, Widdicombe D (2021) Role of Aboriginal Health Practitioners in administering and increasing COVID-19 vaccination rates in a Victorian Aboriginal Community Controlled Health Organisation. Rural Remote Health 21, 7043.
| Crossref | Google Scholar | PubMed |
Stanley F, Langton M, Ward J, McAullay D, Eades S (2021) Australian First Nations response to the pandemic: a dramatic reversal of the ‘gap’. Journal of Paediatrics and Child Health 57, 1853-1856.
| Crossref | Google Scholar | PubMed |
Taylor EV, Lyford M, Parsons L, Mason T, Sabesan S, Thompson SC (2020) “We’re very much part of the team here”: a culture of respect for Indigenous health workforce transforms indigenous health care. PLoS ONE 15, e0239207.
| Crossref | Google Scholar | PubMed |
Wright A, Briscoe K, Lovett R (2019) A national profile of Aboriginal and Torres Strait Islander Health Workers, 2006–2016. Australian and New Zealand Journal of Public Health 43, 24-26.
| Crossref | Google Scholar | PubMed |
Zhao Y, Russell DJ, Guthridge S, Ramjan M, Jones MP, Humphreys JS, Wakerman J (2019) Costs and effects of higher turnover of nurses and Aboriginal health practitioners and higher use of short-term nurses in remote Australian primary care services: an observational cohort study. BMJ Open 9, e023906.
| Crossref | Google Scholar | PubMed |