What are health professionals’ perceptions of conducting routine growth assessments and lifestyle interventions? A qualitative study involving allied health professionals, nurses and doctors in rural and regional New South Wales
Emma Schwartzkoff A B * , Tracy Burrows B , Andrew Bailey C , Eloise Sneddon A and Kerith Duncanson D EA Health Promotion, Mid North Coast Local Health District, Port Macquarie, NSW 2444, Australia.
B School of Health Sciences (Nutrition and Dietetics), University of Newcastle, Callaghan, NSW 2308, Australia.
C Research and Knowledge Translation, Mid North Coast Local Health District, Port Macquarie, NSW 2444, Australia.
D Heath Education and Training Institute (NSW Health), St Leonards, NSW 2067, Australia.
E School of Medicine and Public Health, University of Newcastle, Callaghan, NSW 2308, Australia.
Australian Journal of Primary Health - https://doi.org/10.1071/PY22251
Submitted: 3 November 2022 Accepted: 10 May 2023 Published online: 29 June 2023
© 2023 The Author(s) (or their employer(s)). Published by CSIRO Publishing on behalf of La Trobe University. This is an open access article distributed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND)
Abstract
Background: Allied health professionals, nurses and doctors within the New South Wales (NSW) public health system provide trusted health information to a large proportion of families across the state. This means they are well positioned to opportunistically assess and discuss child weight status with families. Prior to 2016, weight status was not routinely addressed in most NSW public health settings, however recent policy changes promote quarterly growth assessments for all children aged under 16 years who attend these facilities. The Ministry of Health recommend health professionals use the 5 As framework, a consultation approach to encourage behaviour change, to identify and manage children with overweight or obesity. This study aimed to explore allied health professionals’, nurses’ and doctors’ perceptions of conducting routine growth assessments and providing lifestyle support to families in a local health district in rural and regional NSW, Australia.
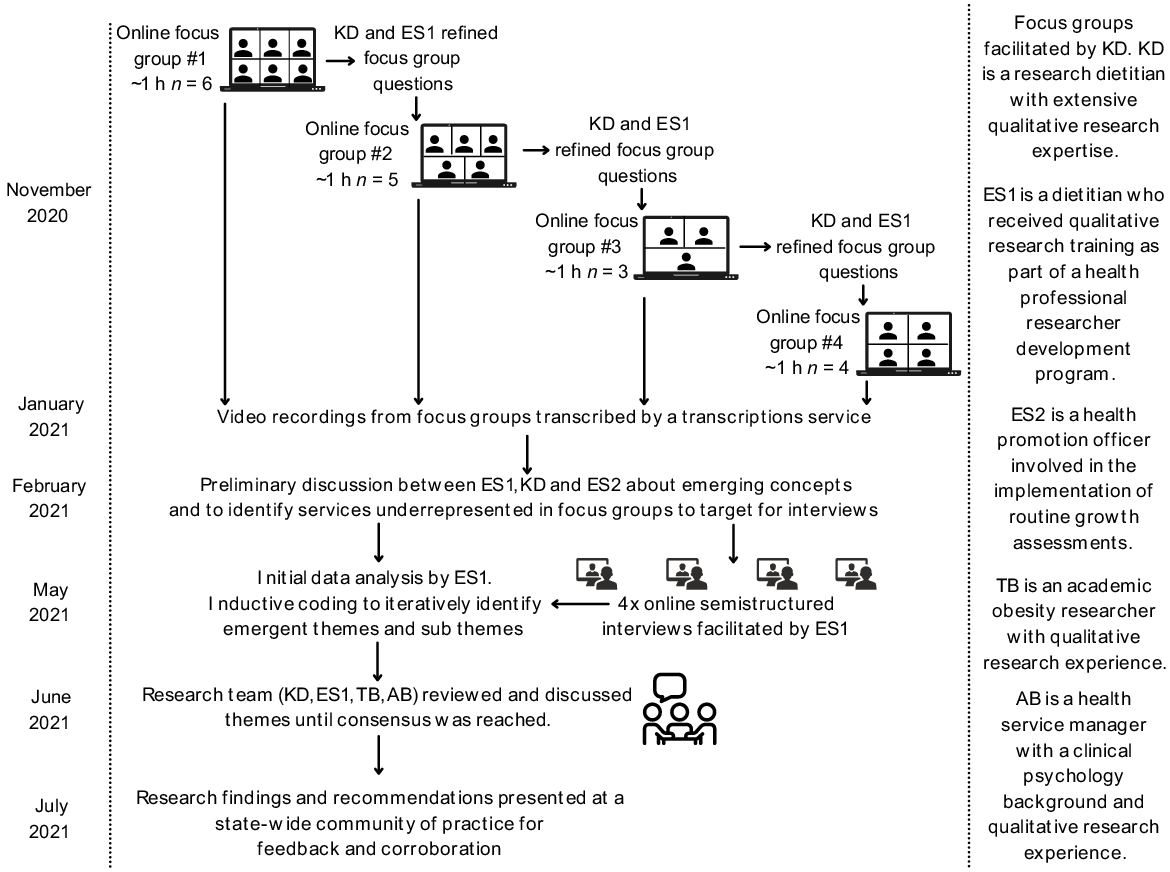
Methods: This descriptive, qualitative study involved online focus groups and semi-structured interviews with health professionals. Audio recordings were transcribed and coded for thematic analysis, with rounds of data consolidation between research team members.
Results: Allied health professionals, nurses and doctors who work in a variety of settings within a local health district of NSW participated in one of four focus groups (n = 18 participants) or semi-structured interviews (n = 4). The predominant themes related to: (1) health professionals’ professional identity and their perceived scope of practice; (2) interpersonal qualities of health professionals; (3) the service delivery ecosystem in which health professionals worked. Diversity in attitudes and beliefs about routine growth assessments were not necessarily specific to discipline or setting.
Conclusions: Allied health professionals, nurses and doctors recognise the complexities involved in conducting routine growth assessments and providing lifestyle support to families. The 5 As framework used in NSW public health facilities to encourage behaviour change may not allow clinicians to address these complexities in a patient centred way. The findings of this research will be used to inform future strategies aimed at embedding preventive health discussions into routine clinical practice, and to support health professionals to identify and manage children with overweight or obesity.
Keywords: BMI-for-age, body weights and measures, health occupations, health professional perceptions, lifestyle intervention, obesity screening, paediatric overweight and obesity, preventive healthcare.
Introduction
One in four Australian children aged 5–14 years live with overweight or obesity (Australian Institute of Health and Welfare 2020). Along with the serious physical and psychosocial implications for the individual (Australian Institute of Health and Welfare 2020), childhood overweight and obesity places a substantial burden on the health system (Brown et al. 2017). While allied health professionals, nurses and doctors (health professionals) have the potential to engage in preventive health discussions and play a key role in early identification and management of children with obesity (Zheng and Cretikos 2019), previous studies indicate that the issue is not routinely addressed in clinical practice (Sivertsen et al. 2008; Davidson et al. 2019a).
Prior to 2016, the NSW Ministry of Health (MoH) recommended that child and family nurses and general practitioners should weigh and measure the height/length of a child as part of routine development checks (NSW Ministry of Health 2015). Missed attendance at these appointments is common; a study conducted in one metropolitan local health district (LHD) showed that 23% of children did not attend their 18 month developmental check, and non-attendance rates were higher in vulnerable populations (Ayer et al. 2020). Missed developmental checks can lead to late detection of health problems including overweight and obesity. To support health professionals to identify and address abnormal growth earlier, in 2016, the MoH introduced several changes: central implementation support; local implementation leadership; education, training and resource development; and performance monitoring. Additionally, a key performance indicator was introduced as part of the annual service level agreement between NSW Health and the 15 LHDs (six metropolitan and nine rural and regional LHDs) across the state; health professionals at public health facilities are now expected to offer growth assessments at least once every 3 months to families with children younger than 16 years who attend their clinical service. This includes inpatient settings, outpatient clinics where patients are not formally admitted to hospital and community-based health services which provide prevention, early intervention, treatment, recovery and health maintenance. Emergency departments and COVID-19 services were excluded. If a child attends multiple services in a quarter, only one health professional is required to complete the growth assessment. Health professionals who subsequently review the patient in the same quarter can see that a growth assessment has already been conducted in the electronic medical records, however, in reality, some patients may receive multiple growth assessments per quarter. The proportion of children with a service encounter who have their growth assessed and recorded in the electronic medical record are monitored and reported each quarter. Routine growth assessment recording rates in one rural and regional LHD have increased from 38% when changes were first implemented in 2017 to 70% in 2022 (data collected for MoH, unpublished).
The 5 As framework: Ask and Assess, Advise, Assist, Arrange is a clinical consultation approach to facilitate behavioural change (Sturgiss and van Weel 2017). It is the approach that the MoH recommend health professionals use to identify and manage childhood obesity (http://pro.healthykids.nsw.gov.au/wp-content/uploads/2021/04/Healthy-Kids-for-Professionals-Snapshot-Report_April-2021.pdf). In line with this approach, health professionals in NSW public health facilities are trained to plot the child’s body mass index (BMI) on a BMI-for-age chart, and provide families with healthy lifestyle education and referrals to community-based lifestyle programs or clinical services as appropriate. The education and referral components of the implementation are not monitored as part of the key performance indicator, so the completion rates and effectiveness are not well understood.
The aim of this study was to explore health professionals’ experiences and perceptions of conducting routine growth assessments and providing healthy lifestyle support to families with children aged under 16 years. The research team envisaged that the findings would inform future implementation strategies to improve the prevention, identification and management of childhood overweight and obesity in a clinical setting.
Methods
This study used a descriptive, qualitative design with focus groups and semi-structured interviews.
Subjects
Participants were nurses, doctors and allied health professionals working in child facing roles in a rural and regional LHD with a population size of approximately 220 000 of which 20% were children aged under 16 years. The LHD provides a range of public health services through seven public hospitals and 12 community health centres (https://www.health.nsw.gov.au/lhd/Pages/mnclhd.aspx). Eligible health professionals were identified from an existing list used to recruit child facing health professionals for online training related to child weight management. There were no exclusion criteria. Three research team members (ES1, ES2 and AB) had previous contact with some participants through their roles within the LHD.
Recruitment
Participants were recruited for focus groups using convenience sampling (Tracy 2019). Recruitment invitations, participant information sheets and consent forms were sent from a generic health service email address to the work email addresses of eligible health professionals (n = 735). A follow-up email was sent 1 week after the initial invitation. Participants who returned a consent form were included in a focus group. Oral health therapists were unable to attend the scheduled focus groups, so an additional group was held with those who had consented during an oral health meeting.
Health professionals from services that were underrepresented in focus groups (refugee health, youth and family mental health, out of home care and emergency department) were purposively recruited to participate in semi-structured interviews. Emergency departments are excluded from the MoH service level agreement changes, but discussions in focus groups indicated that some health professionals thought it should be included, so we felt it was relevant to explore this perspective. Participants who were recruited for interviews were identified from professional networks and recruited via targeted emails or phone calls from a member of the research team. These interviews were used to further explore topics raised during focus groups and to capture diverse clinical perspectives. Participants were not reimbursed for participation, but the focus groups and interviews were conducted within work hours. No consenting participants withdrew from the study.
Data collection
Focus group questions were developed by research team consensus based on an in-depth knowledge of the health service delivery and the research aims. The focus group interview guide is available as Supplementary material 1.
Four online focus groups were conducted in November 2020 via Zoom video conferencing software. Each focus group included three to six participants and was approximately 1 h long. Focus groups were facilitated by a member of the research team (KD), who is an experienced qualitative researcher who does not work within the LHD. Following the focus groups, two researchers (KD and ES1) met to discuss the data, to review the questions and agree which services had been underrepresented. These discussions served a similar purpose to field notes (Tracy 2019).
Semi-structured interviews were conducted in May 2021 via Zoom video conferencing software. Interviews were conducted by a member of the research team who is involved in the implementation of clinical practice changes related to childhood obesity across the LHD (ES1). Interview participants were given the option of an external interviewer, but all declined.
Focus groups and interviews were video recorded and recordings transcribed verbatim by a transcription service. Transcripts were deidentified except for participants’ clinical setting. Transcripts were checked for accuracy before analysis. Participants did not have the opportunity to review focus group transcripts due to the inability to maintain data security.
Data analysis
Three researchers (ES1, ES2, KD) had preliminary discussions about concepts emerging from the focus groups before the semi-structured interviews were conducted. One researcher (ES) analysed the data in Excel using inductive coding and iteratively identified emergent themes (Tracy 2019). Themes were revised as new data emerged from interviews. Themes and subthemes were collated into a table with supporting quotes to provide context and evidence for the theme (Tracy 2019). The research team agreed that theoretical saturation (Tracy 2019) was achieved when no new themes or subthemes were identified in an interview, and the main service delivery settings and health professional role types had been represented. At that point, no further interviews were scheduled. Four researchers (ES1, KD, AB, TB) reviewed and discussed themes until consensus was reached.
The data collection and analysis process is summarised in Fig. 1.
Dissemination of findings
For the purpose of knowledge translation, five meetings with relevant stakeholders within the health service governance structures were conducted. Stakeholder groups were identified through professional networks and included senior and middle management, health professionals and policy makers. All meetings were conducted virtually via video conferencing software and included a 10–30 min presentation followed by questions and discussion time. The purpose of these meetings was to ensure that decision makers at all levels of the health system were aware of the research findings to inform policy, reporting requirements and implementation strategies. Discussions and arising actions were documented in meeting minutes and video recordings.
A document summarising the research findings and the next steps was developed for dissemination to research participants.
Rigour
The research team, which consisted of researchers with preventive health expertise and qualitative research experience, implemented strategies to ensure study quality, reliability, validity and credibility (Tracy 2019). Focus group and interview questions were pilot tested with three health professionals from other LHDs to ensure that questions were worded in a way that would elicit responses relevant to the research aims. Preliminary discussions between three researchers immediately after focus groups were conducted for the purpose of reflexivity. These discussions then informed subsequent data collection and interpretation, contributing to rigour. The research team also reviewed and discussed coded data to ensure inter-coder reliability (Tracy 2019) and to discuss any differing perspectives and interpretations.
Results
Participant characteristics
Twenty two participants were recruited to the study. Three nurses and 15 allied health professionals from inpatient, outpatient and community health settings participated in the focus groups. Two allied health professionals, one nurse and one doctor participated in semi-structured interviews. The diversity of the participant sample is shown in Table 1.
| Focus group | Participants’ clinical settings | Context of clinical settingsA |
|---|---|---|
| Focus group 1 (n = 6) | Community audiometry (n = 1) | Hearing testing for children aged 3–18 years |
| Community occupational therapy (n = 1) | Functional skill development for children of all ages. | |
| Community child and family nursing (n = 1) | Support for families with children aged 0–5 years. | |
| Outpatient early start physiotherapy (n = 1) | Assessment of babies’ development in the first 24 months of life. | |
| Community paediatric speech pathology (n = 1) | Assistance with communication or feeding problems for children aged 0–6 years and assessment for children aged up to 10 years. | |
| Outpatient diabetes dietetics (n = 1) | Nutrition assessment, care planning and education to adults and children with diabetes. | |
| Focus group 2 (n = 5) | Community oral health (n = 5) | Dental care for adults and children |
| Focus group 3 (n = 3) | Outpatient early start occupational therapy (n = 2) | Assessment of babies’ development in the first 24 months of life. |
| Community child and family nursing (n = 1) | Support for families with children aged 0–5 years. | |
| Focus group 4 (n = 4) | Community dietetics (n = 1) | Predominantly adult service who occasionally see children for nutrition assessment, planning and education. |
| Inpatient paediatric ward (n = 1) | Admitted hospital care for children aged 0–18 years | |
| Outpatient fracture clinic (n = 1) | Orthopaedic and physiotherapy service for adults and children with bone fractures. | |
| Community continence clinic (n = 1) | Treatment and management of incontinence for adults and children. | |
| Semi-structured interview (n = 4) | Emergency department (n = 1) | Care for adults and children who require urgent medical attention. |
| Community child and adolescent mental health services (CAMHS) (n = 1) | Mental health assessment and support for children and adolescents aged 0–17 years. | |
| Outpatient refugee health (n = 1) | Assessment and primary care to newly arrived refugees to health services in New South Wales (NSW). | |
| Community out of home care (OOHC) (n = 1) | Coordinated assessment and intervention for children and adolescents aged 0–17 years entering statutory OOHC |
AThis data was not collected as part of the research but is provided as context from information that is freely available online from https://mnclhd.health.nsw.gov.au/your-services/.
Main themes
Health professionals’ experiences of implementing routine growth assessments and providing healthy lifestyle support were diverse. Health professionals in similar roles did not necessarily share similar experiences. Health professionals felt that patient centred care was key to identify and manage childhood overweight and obesity safely and effectively. They discussed this through the lens of the 5 As framework. Three predominant themes were evident from the data and related to health professionals’ professional identities and their perceived scope of practice, interpersonal qualities of health professionals and the service delivery ecosystem in which they worked.
Professional identity and perceived scope of practice
Health professionals perceived the clinical practice changes related to childhood obesity differently, depending on how closely the changes aligned with the clinical service they traditionally provided and their perceived scope of practice:
Well, it is my core business being a dietitian, so I’m very comfortable with doing height and weight assessments on whoever walks through my door. (Outpatient diabetes dietetics)
Most health professionals who participated in the focus groups had a firm view about the scope of their clinical role. Some found it difficult to understand how identification and basic management of children with obesity could fit into that role:
I find it hard to then turn that into my role because I am really trying to grasp these kids for quite a specific assessment, and it is quite left field. (Community audiometry)
I just find it hard to then have that conversation. It’s not my area, it’s not what I do. (Outpatient early start physiotherapy)
Interpersonal qualities of health professionals
Health professionals identified that a positive relationship between families and health professionals is important when discussing weight status and lifestyle with families. Health professionals who had strong, ongoing relationships with families found it easier to initiate conversations about weight status and lifestyle than health professionals working in one-off, high-volume services where they had less time to develop rapport:
There’s a lot of trust between parents and nurses… we can give more person-to-person advice. (Inpatient paediatric ward)
But I don’t know if it is the most receptive environment. Like [x] was saying about having the parents on the ward and seeing the patient, you probably have a bit more time to build up a rapport. (Outpatient fracture clinic)
The health professionals who participated in this study generally believed that they discussed overweight and obesity in a sensitive way, but many had encountered families who felt they had been treated insensitively in other settings:
I have had people go ‘oh, had to be weighed and measured at someplace and they just told me I was fat’. (Community dietetics)
Parents can come in crying saying ‘you know, they’re saying this about my child’. (Outpatient early start occupational therapy)
Service delivery ecosystem
The MoH has introduced health professional education and resources for families, along with a new service measure and performance monitoring to support health professionals to discuss children’s weight status and lifestyle in clinical settings. Despite these changes there are still aspects of the service delivery ecosystem that make it difficult for health professionals to address the issue in a meaningful way.
Health professionals identified time limitations as a major barrier to addressing a child’s weight status and lifestyle in clinical practice:
It was already taking me a full hour to do my assessment in my role, so it’s definitely a time thing for me. (Community audiometry)
We have such limited time and so many messages that we want to get across. (Community oral health)
Time limitations sometimes meant that aspects of the patient’s care related to the presenting complaint were compromised in order to fit in the growth assessment:
It takes a considerable amount of time to do it and to the point where sometimes we have to defer other things that we would normally do in that appointment for the next appointment in order to fit that in. (Community oral health)
Some health professionals would make time to conduct the growth assessment but reported that they did not have the time to provide healthy lifestyle support to families:
… and even if I get to do the clinical height and weight, you’re at the end of your session anyway, so you don’t really have time to carry on that education …. (Community audiometry)
Health professionals reported that they prioritised growth assessments over the provision of lifestyle support because of the reporting requirements. Some health professionals expressed concern about the focus on data collection rather than meaningful activity to support children with obesity:
Just identifying the percentage of children who are overweight or obese is not going to change the incidence of overweight and obesity, because we need more people to drive the conversations and to work with these children and families. (Outpatient diabetes dietetics)
Currently in NSW, community based healthy lifestyle programs are available for some age groups, and health professionals who utilised these services had confidence in them:
… anyone who’s done it [Go4Fun] has gotten a lot out of it, from the feedback that I’ve had. (Outpatient early start occupational therapy)
However, health professionals also felt that it was sometimes difficult to meaningfully support children with obesity because there were insufficient programs or services available:
There’s not programs for all age groups. (Community oral health)
… there is nobody exclusively working in paed[iatric]s, so there’s very limited capacity to accept referrals which ultimately means that people don’t refer because they know there’s no capacity and they know that unless it’s really extreme, there’s not going to be a person to see. (Outpatient diabetes dietetics)
Health professionals in our study also felt it was ineffective to refer to GPs since they face the same service limitations:
Even referring to a GP, like really, what are you expecting them to do? (Community child and family nursing)
Some health professionals believed that GPs contradicted the advice they provided. This had negative ramifications for the rapport health professionals had built with families:
We’ve referred on to GPs and we’ve been really dismissed, and then it’s kind of I think tainted our relationship with the family because it’s then like ‘oh, she overreacted, that nurse overreacted’. That can be really debilitating in your job; it’s a really crappy part where you’re trying to do the best. (Community child and family nursing)
Communication of findings to influence implementation strategies
Findings were presented to relevant end users (see Table 2) to communicate recommendations and attempt to influence changes related to policy, reporting requirements and implementation strategies.
| Target audience | Impact |
|---|---|
| NSW state-wide Community of Practice with representatives from the MoH and other LHDs who are responsible for the implementation of routine growth assessments across NSW. | Prompted and informed discussions about included and excluded services. Highlighted that the findings were relevant to other jurisdictions |
| LHD working group comprising of clinical and health promotion managers who meet regularly to ensure the optimal implementation of routine growth assessments and brief lifestyle interventions. | Informed implementation strategies including resource development and review of referral pathways |
| LHD governing board subcommittee who provide leadership and strategic advice to the LHD Governing Board and Senior Executive Team (SET) in relation to research and innovation activity | Increased awareness of senior executives about routine growth assessments and the current state in the LHD |
| LHD Advisory Committee who provide strategic direction and advice and receive feedback and reports on matters relating to Allied Health. | Prompted further consideration of future clinical referral pathways within LHD for children with overweight and obesity |
| Delegates attending the Australian and New Zealand Obesity Society Annual Meeting 2021 | Highlighted that the findings were relevant to other jurisdictions |
Discussion
This study identified that the professional identity and perceived scope of practice, interpersonal skills and health service delivery ecosystem of health professionals influenced the experiences and perceptions about conducting routine growth assessments using the 5 As framework. The 5 As framework has previously been described as an ‘initial descriptor’ to ‘direct patient care’ but it has been criticised as too simplistic for a complex condition like obesity (Sturgiss and van Weel 2017). Our findings expand on these assertions by providing context and examples. Our research also extends the existing literature about the potential roles of health professionals in the prevention, early identification and management of childhood obesity, as most studies have focussed on the role of GPs (Sivertsen et al. 2008; Jones et al. 2014). This research extends our knowledge and understanding of growth assessments and obesity interventions beyond general practice settings and focusses on a broader range of clinical settings and range of health professionals in the NSW public health system.
Professional identity and perceived scope of practice
Findings related to professional identity and perceived scope of practice contrasted with previous related research (Sivertsen et al. 2008; Jones et al. 2014), which reported that health professionals did see childhood obesity as a significant issue and felt that it was important that they managed it. The difference in our study is likely due to the inclusion of a wide range of health professionals across different disciplines compared to previous studies which have focussed on general practice only. GPs’ scope of practice is broad by definition and specifically encompasses ‘prevention, health promotion (and) early intervention’ (Royal Australian College of General Practitioners 2022). In contrast, there is inconsistency between clinical practice guidelines for the management of overweight and obesity (National Health and Medical Research Council 2013) and the expectations of some professional associations whose scope of practice is quite directive and specific to a single body function rather than acknowledging scope for wholistic, preventive health care (Audiology Australia the Australasian College of Audiology the Hearing Aid Audiometrist Society of Australia 2016; Davidson et al. 2019a). Similarly, tertiary education institutions’ medical, nursing and allied health curriculums reportedly do not equip future health professionals with the skills and knowledge to address childhood obesity (Jacobson and Gance-Cleveland 2011). As population health needs for chronic disease management increase, health professionals employed in the public health sector will increasingly be expected to provide routine basic preventive health care. Engaging professional associations and tertiary education institutions to embed education about managing children with obesity into professional development opportunities and educational curricula may build competency and confidence in these areas.
This research did not collect data about health professional’s age and years of experience working in the NSW health system. Future research should explore differences in the perceptions of health professionals who entered the system after the service changes were introduced in 2016 and those who have been expected to implement a practice change. A difference in attitude between these two groups may indicate that a sustainable, cultural shift is occurring as a result of the service changes.
Interpersonal qualities of health professionals
Previous research has suggested that health professionals’ discomfort in discussing children’s weight status is often the main barrier preventing them from addressing it in practice (Jones et al. 2014). Similar to Edvardsson et al. (2009), our findings suggest that health professionals are more likely to discuss this uncomfortable topic if they already have an established relationship (Edvardsson et al. 2009).
There is a paucity of information about families’ perceptions of growth assessments and lifestyle conversations in Australian healthcare settings. The existing literature suggests that while parents see the value of routine growth assessments (Davidson et al. 2019b) they often feel that the information they are provided in clinical settings is unhelpful or dismissive (Edmunds 2005), and parents are often left unsure how to manage their child’s weight despite the child being identified as overweight or obese by a health professional (Hardy et al. 2019). Most health professionals in the LHD we studied had participated in online training and face-to-face in-services to educate them how to discuss childhood obesity with families to motivate lifestyle changes and to avoid stigmatising language. Previous research has found that parents dislike weight related terminology such as ‘overweight’ and ‘obese’ (Farnesi et al. 2012) so health professionals have been trained to use phrases such as ‘above the healthy weight range’. The provision of healthy lifestyle support is not monitored so the extent to which health professionals are using the language and resources provided is not known. Further research is required to better understand how health professionals are approaching these conversations and how children and families perceive them.
Service delivery ecosystem
Time limitations have often been identified as a major barrier preventing health professionals from conducting growth assessments (Johnston et al. 2011; Findholt et al. 2013). In most settings, consultation times have not been extended since routine growth assessments were introduced, and no additional funding has been provided. The reporting and monitoring requirements for the new service measure have helped to embed growth assessments in routine practice, but time limitations are still identified as a barrier to the provision of lifestyle education. Previous research has addressed the need for appropriate education to complement growth assessments (Findholt et al. 2013). It may be useful to review current reporting requirements to ensure there is a focus on preventive health discussions and management of children with overweight or obesity as well as identification. Strategies to optimise workflow, such as improving access to equipment and digitising referral processes, may also help to address time limitations and make it easier for health professionals to address child weight status and lifestyle concerns.
Previous research has also suggested that obesity screening should be conducted in conjunction with referrals to weight management services (Findholt et al. 2013). As health professionals in our study identified, there are currently service gaps in our LHD for children with overweight or obesity aged 3–6 and 14–16 years, and no secondary weight management clinic for children with more complex needs. None of the four multidisciplinary weight management services in NSW are in rural or regional areas. Locally, the health promotion team is working to extend the age range of existing preventive health programs to address some service gaps, but this requires additional funding. Service gaps related to clinical services require an LHD response as part of paediatric clinical service planning. The increasing availability of telehealth may help to improve equity of access to services in the future, enabling children with obesity to be managed more effectively in rural and regional areas (Moorman et al. 2021).
Our research suggests that there is sometimes a disconnect between the health care provided by LHD health professionals and GPs in relation to childhood obesity. This finding is supported by previous studies demonstrating that GPs’ adherence to published obesity management guidelines is poor (Holt et al. 2011; Gage et al. 2012). Policy and reporting changes within the public health system are unlikely to generate practice change in the GP setting so further research may be required to identify policies, incentives or training that may influence practice in this setting.
Contributing factors for success of project
This body of research was designed to directly translate into changes to health service delivery. Understanding health professionals’ experience of providing care is an essential aspect of value-based health care. Communicating findings and recommendations within health service governance structures can inform change. Recommendations related to policy, reporting requirements and implementation strategies will impact all end users including MoH, staff who are responsible for implementing growth assessments in different districts, health professionals and families.
Factors additional to the body of research that will contribute to translational success include the service agreement key performance indicator which creates visibility, interest and accountability around this topic and the chief investigator’s embedded role within the health service, established networks and relationships with teams across the health service and within the MoH.
Strengths and limitations
The participation of a wide range of health professionals from different clinical settings allowed for in-depth, multidisciplinary exploration of the research question. The health professionals who participated in this research were open about their experiences, and their insights provided useful direction for the future. This study followed the COREQ guidelines for implementing and reporting qualitative research, demonstrating rigour in data collection and analysis.
The response rate to recruitment emails and final sample size (n = 22) were small, and it is possible that those who participated in the study felt strongly about the topic or were invested in the outcomes of the research, creating potential response bias. However, the aim of recruitment was to capture representation across a wide range of professions for an exploratory research design rather than a large sample size and this was achieved. This research was conducted during the COVID-19 pandemic when health resources were diverted and health professionals were extremely time poor. This may have contributed to the low response rate. Due to time limitations, it was difficult to conduct focus groups at a suitable time for all participants, so we conducted an additional focus group with oral health therapists alone. Differences have been noted in the group dynamics, depth of interaction and diversity of natural groups (oral health group) compared to constructed groups (other focus groups with a heterogenous mix of health professionals) (Leask et al. 2001). This may have impacted our findings, however, the data collected in this focus group reflected the data collected in other focus groups and semi-structured interviews.
This study was conducted in one rural and regional LHD. Other areas will have different population demographics, clinical practices and available services, therefore the results are not intended to be generalisable to other areas within Australia or internationally. However, incidental findings reported at a state-wide community of practice and responses from a national conference (Australian and New Zealand Obesity Society Annual Meeting 2021) indicated that the issues raised were applicable across other jurisdictions, and this is currently being explored in other studies being conducted across the state. While representation was achieved from a range of professions, this research does not represent all views, for example we were unable to recruit a paediatrician. A stronger representation of medical professionals would have been valuable, given their influence in terms of health policy and practice (Lewis 2006).
Conclusion
Health professionals recognise the complexities involved in conducting routine growth assessments and providing lifestyle support to families. The 5 As framework used in NSW public health facilities to encourage behaviour change may not allow clinicians to address these complexities in a patient centred way. The experiences and perceptions of health professionals in this study indicate that consistency in health professionals’ approach to preventive health care, improved continuum of care for children with obesity and increased access to appropriate support for families of children with overweight or obesity are priority areas for practice change. Further translational research may see these strategies influence implementation and policy towards improved identification, prevention and management of childhood overweight and obesity in clinical settings.
Data availability
The data that support this study cannot be publicly shared due to ethical or privacy reasons and may be shared upon reasonable request to the corresponding author if appropriate.
Declaration of funding
This work was supported by the NSW Health Education and Training Institute (HETI) (2019) who provided funding to MNCLHD to support 60 days of time release from the chief investigator’s substantive role to conduct the research as part of the Rural Research Capacity Building Program. HETI also provided access to research supervisors and mentors who are listed as co-investigators on this paper.
References
Audiology Australia the Australasian College of Audiology the Hearing Aid Audiometrist Society of Australia (2016) Scope of practice for audiologists and audiometrists. Available at https://audiology.asn.au/Tenant/C0000013/Position%20Papers/Other%20documents/Scope%20of%20Practice%20All-in-one%2020170119.pdf [Accessed 29 September 2022]
Australian and New Zealand Obesity Society Annual Meeting (2021) ANZOS 2021. Virtual, July 2021. Available at https://www.anzos.com/anzos-annual-meeting
Ayer C, Eapen V, Overs B, Descallar J, Jalaludin B, Eastwood JG, Dissanayake C, Williams K, Murphy E, Woolfenden S, for the Watch Me Grow Study Group (2020) Risk factors for non-participation in a universal developmental surveillance program in a population in Australia. Australian Health Review 44, 512-520.
| Crossref | Google Scholar |
Brown V, Moodie M, Baur L, Wen LM, Hayes A (2017) The high cost of obesity in Australian pre-schoolers. Australian and New Zealand Journal of Public Health 41, 323-324.
| Crossref | Google Scholar |
Davidson K, Vidgen H, Denney-Wilson E, Daniels L (2019a) Who is responsible for assessing children’s weight status? – a qualitative study of health professionals in regional Australia. BMC Public Health 19, 1196.
| Crossref | Google Scholar |
Davidson K, Vidgen H, Denney-Wilson E (2019b) Parental opinions about the responsibility for assessing children’s weight status – a survey of Rockhampton parents. Australian and New Zealand Journal of Public Health 43, 436-442.
| Crossref | Google Scholar |
Edmunds LD (2005) Parents’ perceptions of health professionals’ responses when seeking help for their overweight children. Family Practice 22, 287-292.
| Crossref | Google Scholar |
Edvardsson K, Edvardsson D, Hörnsten Å (2009) Raising issues about children’s overweight – maternal and child health nurses’ experiences. Journal of Advanced Nursing 65, 2542-2551.
| Crossref | Google Scholar |
Farnesi B-C, Ball GDC, Newton AS (2012) Family–health professional relations in pediatric weight management: an integrative review. Pediatric Obesity 7, 175-186.
| Crossref | Google Scholar |
Findholt NE, Davis MM, Michael YL (2013) Perceived barriers, resources, and training needs of rural primary care providers relevant to the management of childhood obesity. The Journal of Rural Health 29, s17-s24.
| Crossref | Google Scholar |
Gage H, Erdal E, Saigal P, Qiao Y, Williams P, Raats MM (2012) Recognition and management of overweight and obese children: a questionnaire survey of general practitioners and parents in England. Journal of Paediatrics and Child Health 48, 146-152.
| Crossref | Google Scholar |
Hardy K, Hooker L, Ridgway L, Edvardsson K (2019) Australian parents’ experiences when discussing their child’s overweight and obesity with the Maternal and Child Health nurse: a qualitative study. Journal of Clinical Nursing 28, 3610-3617.
| Crossref | Google Scholar |
Holt N, Schetzina KE, Dalton WT, III, Tudiver F, Fulton-Robinson H, Wu T (2011) Primary care practice addressing child overweight and obesity: a survey of primary care physicians at four clinics in southern Appalachia. Southern Medical Journal 104, 14-19.
| Crossref | Google Scholar |
Jacobson D, Gance-Cleveland B (2011) A systematic review of primary healthcare provider education and training using the Chronic Care Model for Childhood Obesity. Obesity Reviews 12, e244-e256.
| Crossref | Google Scholar |
Johnston JCT, McNeil DA, Best M, MacLeod C (2011) A growth status measurement pilot in four Calgary area schools: perceptions of grade 5 students and their parents. The Journal of School Nursing 27, 61-69.
| Crossref | Google Scholar |
Jones KM, Dixon ME, Dixon JB (2014) GPs, families and children’s perceptions of childhood obesity. Obesity Research & Clinical Practice 8, e140-e148.
| Crossref | Google Scholar |
Leask J, Hawe P, Chapman S (2001) Focus group composition: a comparison between natural and constructed groups. Australian and New Zealand Journal of Public Health 25, 152-154.
| Crossref | Google Scholar |
Lewis JM (2006) Being around and knowing the players: networks of influence in health policy. Social Science & Medicine 62, 2125-2136.
| Crossref | Google Scholar |
Moorman EL, Koskela-Staples NC, Mathai BB, Fedele DA, Janicke DM (2021) Pediatric obesity treatment via telehealth: current evidence and future directions. Current Obesity Reports 10, 371-384.
| Crossref | Google Scholar |
National Health and Medical Research Council (2013) Clinical practice guidelines for the management of overweight and obesity in adults, adolescents and children in Australia. Available at www.nhmrc.gov.au/about-us/publications/clinical-practice-guidelines-management-overweight-and-obesity#block-views-block-file-attachments-content-block-1 [Accessed 29 September 2022]
Royal Australian College of General Practitioners (2022) What is general practice? Available at https://www.racgp.org.au/education/students/a-career-in-general-practice/what-is-general-practice [Accessed 29 September 2022]
Sivertsen LM, Woolfenden SR, Woodhead HJ, Lewis D (2008) Diagnosis and management of childhood obesity: a survey of general practitioners in South West Sydney. Journal of Paediatrics and Child Health 44, 622-629.
| Crossref | Google Scholar |
Sturgiss E, van Weel C (2017) The 5 As framework for obesity management: do we need a more intricate model? Canadian Family Physician 63, 506-508.
| Google Scholar |
Zheng A, Cretikos M (2019) How can health services strengthen support for children affected by overweight and obesity, and their families? Public Health Research & Practice 29, e2911903.
| Crossref | Google Scholar |