A community proactive health management model for family doctors in Shandong, China
Meng Yang A *A
Abstract
Chronic disease management is an essential part of public health management and a fundamental means of slowing down the progression of major diseases. Unlike traditional medical care, proactive health management focuses on the combination of prevention and treatment. Proactive health management can reduce the re-admission rate of patients with chronic diseases, improve long-term prognosis, and effectively reduce the disability and mortality rates of major health events. This study aimed to establish a proactive health management model based on a grid-based medical service team arrangement, and to explore the effect of this model on managing chronic diseases in community health service institutions.
A grid-based medical service team was established in Binzhou, Shandong, China, consisting of general practitioners, nurses, public health doctors, health promoters and community grid liaison staff. Each team was responsible for several areas to monitor critical populations within the grid and compile statistics on the health management of these key populations in 2022–2023.
A total of 2050 patients with coronary artery disease, 4973 patients with hypertension, and 1621 patients with type 2 diabetes were followed up in 2022. Compared with 155,612 resident health records in 2022, the number of records increased by 140.50% in 2023. The number of patients with hypertension under health management in 2023 increased by 50.92%; patients with type 2 diabetes increased by 74.65%; and the number of coronary artery disease increased by 42.00%. After the implementation of grid management, the hospitalisation rate for patients with type 2 diabetes significantly decreased in 2023 (P < 0.05). However, the hospitalisation rate for patients with coronary artery disease and hypertension was similar in 2023 to that in 2022 (P > 0.05).
The grid-based community proactive health management model makes full use of the advantages of community resources and improves the pertinence and coverage of community health services. Moreover, it reduces hospitalisation for patients with type 2 diabetes.
Keywords: chronic disease management, community joint prevention, evidence-based medicine, family doctor, grid management, long-term prognosis, proactive health management model, public health services.
Introduction
The recent coronavirus disease 2019 (COVID-19) pandemic has challenged global health management over the past 4 years (Brotons et al. 2020; Liu et al. 2021). From the perspective of evidence-based medicine, people with chronic diseases have a higher risk of developing severe COVID-19 infection, and there is evidence that underlying cardiovascular disease leads to more severe COVID-19 progression and a higher risk of death (Aghagoli et al. 2020; Teuwen et al. 2020; Nunez-Gil et al. 2021). People who recover from COVID-19 are more likely to develop chronic diseases, especially coronary artery disease, hypertension and diabetes (Wang et al. 2020a; Zheng et al. 2020). Chronic disease management is, therefore, part of significant public health management and is a fundamental means of mitigating the development of major diseases. Proactive health management is beginning to gain attention. Unlike traditional medical treatment, proactive health management pays more attention to the combination of prevention and treatment. Modern medicine and modern management means proactive health management evaluates and monitors the health status of individuals and groups, and the risk factors affecting their health, effectively intervenes, and continuously tracks prevention and management (Guo et al. 2019; Li and Yu 2020; Ye et al. 2021). Proactive health management can reduce the number of re-hospitalisations of patients with chronic diseases, improve long-term prognosis, and effectively reduce the disability and mortality rates for significant health events (Lucas and Rojas 2014; Pavel et al. 2015).
The community joint prevention and control policy has become a prominent ‘Chinese experience’ in managing public health incidents (Bangura et al. 2020; Cheng et al. 2020). Implementing community health service institutions and family doctor contract services is the focus of national essential public health (Zheng et al. 2018; He et al. 2019). However, due to the limited human resources at the grass-roots level, it is difficult for grass-roots medical staff to go deep into every corner of the community to publicise and implement the national essential public health services and family doctor contracted services, resulting in difficulty in achieving full coverage of community health services. As a result, residents’ satisfaction and awareness of essential public health services and family doctor contracted services are low (Ren et al. 2018; Hu and Huang 2020; Wang et al. 2020b).
This study takes the research on establishing a grid management service model for family doctors to a street in Shandong to promote COVID-19 prevention and control as a case study. The ‘trinity’ working mode of community workstations, police districts and community health centres carried out in this area has played an essential role in preventing and controlling COVID-19 (Yan et al. 2020). This study draws on the epidemic prevention and control work model (Liu et al. 2019) to carry out the grid management by family doctors in communities, aiming to establish the grid management service model of family doctors and explore the benefits to chronic disease patients by providing a reference model for other regions to carry out national essential public health services and contract services by family doctors.
Methods
This study takes the practice of a grid-based community proactive health management model carried out by a community health service centre in a particular street in Binzhou as a research case study. The community health service centre in the street area is located in the central north of Shandong. The regional social health centre has nine community health service centres (stations) with 256 staff members, including 70 doctors (general practitioners and specialist doctors). The street has nine community workstations and 315 grid areas, with a permanent population of approximately 297,200. The following steps introduced the grid management model to the area in 2023.
Build a framework for the grid management of family doctors
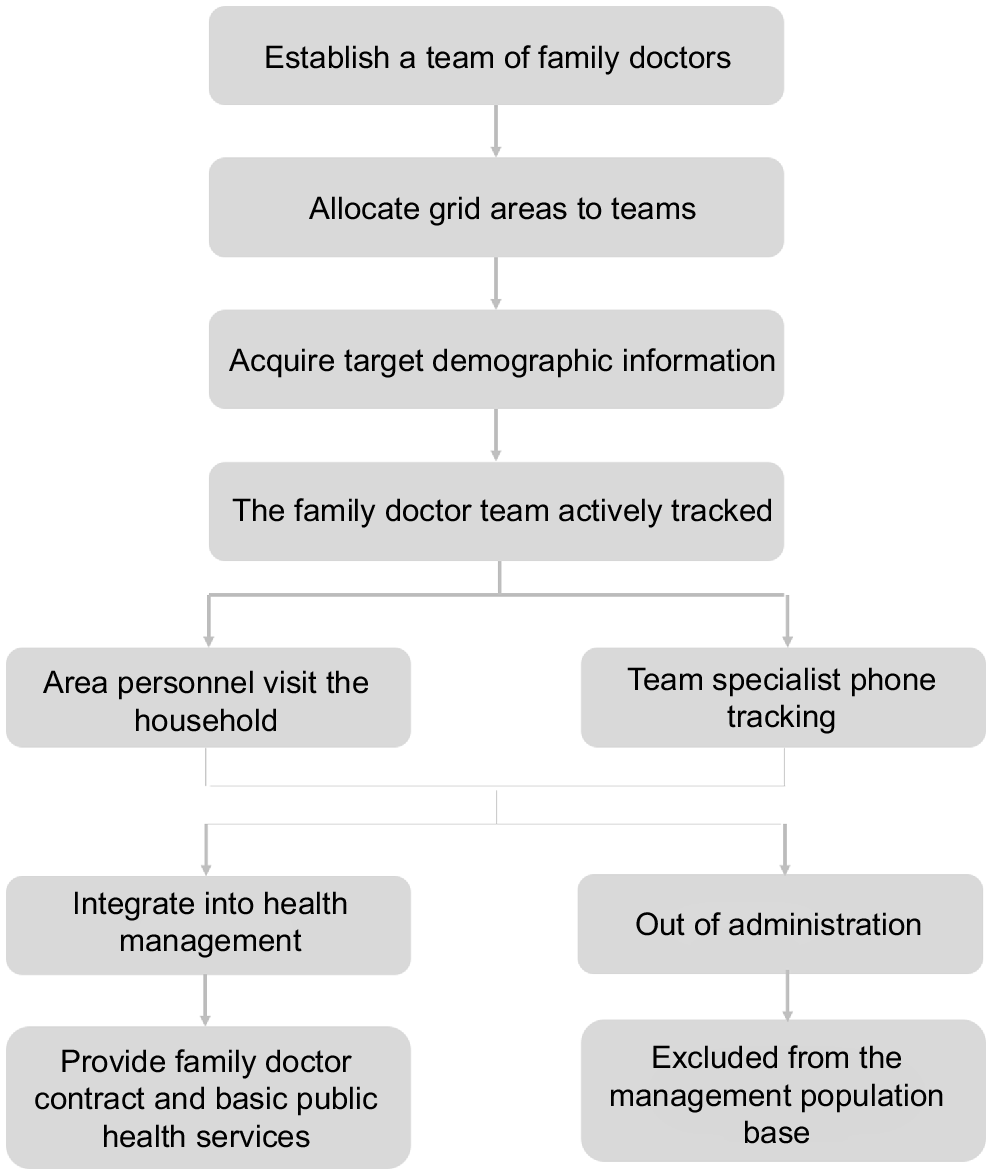
The family doctor grid management framework divides the community served by the social health centre into several areas according to a grid, with one family doctor team looking after one area on the grid. Concurrently, other community grid members are added to the family doctor team to implement national essential public health services and family doctor contract services to fully provide for the grid area. The grid management framework process is shown in Fig. 1.
Health grid management method
According to the community grid division and population distribution, combined with the number of family doctor teams in the social health centre, each family doctor team is responsible for several grid areas. The team provides for the health needs of residents in the area. The family doctor team’s services focus on managing patients in the area who have chronic diseases. At present, the key population services are for coronary artery disease patients, patients with hypertension, and patients with type 2 diabetes.
Implementation process and grid management steps
A grid-based family doctor team was established to connect with community workstations, grid stations, and mass service centres. District grid members and mass service centre volunteers were incorporated into the family doctor team to fully leverage community resources’ benefits and jointly carry out national essential public health services.
A reasonable division of the management areas was allocated to each team. According to the staffing characteristics of each family doctor team, the population structure of each region, especially the number of key groups (hypertension, type 2 diabetes, coronary artery disease), and the community characteristics (such as enterprise-based communities and residential communities), the areas under the jurisdiction of each team are divided. Each team was responsible for the family doctor contract services for key groups and national basic public health services in its jurisdiction. The contract services include health education, family follow-up assessment (every month for chronic disease groups, half a year for sub-healthy residents, and once a year for healthy groups), physique identification in traditional Chinese medicine, rehabilitation and training plans (for patients with rehabilitation needs), and ‘homeward’ services (urinary catheterisation, on-site blood glucose testing).
By exchanging population data with the district health bureau and then conducting visits by grid personnel and phone tracking by health promotion personnel, an understanding of the health needs of key populations in the area was developed. Each team can understand the health needs of key populations in the management area, laying the foundation for the next step of key population tracking management.
Unmanaged key groups were followed up in the grid area, including patients with coronary artery disease, hypertension, and type 2 diabetes. The family doctor team targeted the key groups, informed the social health centre of the national basic public health service content, and included those patients with health needs in the health management of the social health centre to provide them with national basic public health services.
Annual hospitalisation rates in key populations
Annual hospitalisation rates are calculated to assess the benefits to chronic disease patients. Non-disease-related complications will be excluded from the hospitalisation rate calculation. The complications of diabetes include ketoacidosis, hyperosmolar coma, and various secondary infections (common in the foot, lung, and urinary tract). Stroke, myocardial infarction, renal failure, retinopathy, and heart failure are complications of hypertension. Arrhythmias, acute myocardial infarction, heart failure, coronary assessment, and cardiomyopathy will be included in the hospitalisation rate for chronic heart disease.
Statistical analysis
SPSS 22.0 was used for data analysis, the Kolmogorov–Smirnov test was used to assess the normality of measurement data, and the Levene method was used to test the homogeneity of variance of measurement data. The Mann–Whitney U rank sum test was performed for data that fitted a non-normal distribution or uneven variance. P < 0.05 indicated that the difference was statistically significant.
Results
Grid division status of family doctors in the case area
Consistent with the grid management requirements for family doctors and the formation of family doctor teams in other regions of China, in this case study street, nine social health centres (stations) formed a total of 63 family doctor teams, each consisting of general practitioners, nurses, public health physicians, health promoters, and community grid members. As shown in Table 1, the street had a total of 315 grids and a population of 297,200. The grid was evenly distributed and managed based on the population and key patients of the area, with an average of five grids managed by each team. The street was divided into 63 family doctor grid areas.
| Community healthy centre | Doctor team (n) | Grid count (n) | Family Physicians (n) | Nurses (n) | Public health physicians (n) | Liaison staff (n) | |
|---|---|---|---|---|---|---|---|
| Xin Pu Cheng | 2 | 16 | 3 | 6 | 1 | 16 | |
| Zhao Si Wu | 5 | 10 | 5 | 4 | 1 | 8 | |
| Niu Wang | 7 | 21 | 7 | 6 | 2 | 19 | |
| Liu Kou | 4 | 18 | 5 | 6 | 1 | 18 | |
| Wu Li | 7 | 40 | 9 | 6 | 1 | 39 | |
| Lao Pu Cheng | 11 | 54 | 12 | 10 | 3 | 50 | |
| Gao Du | 6 | 26 | 6 | 5 | 1 | 26 | |
| Peng Zhuang | 7 | 45 | 8 | 6 | 1 | 45 | |
| Nan Guan | 6 | 53 | 7 | 7 | 2 | 53 | |
| Xiao Guo | 8 | 32 | 8 | 8 | 2 | 30 | |
| Total | 63 | 315 | 70 | 64 | 15 | 304 |
Key population tracking in the grid management model improves the patient accessibility of public health services
The community health centre tracked a total of 6098 patients with coronary artery disease, 8707 hypertensive patients, and 3360 patients with type 2 diabetes in the case street area. Before this grid management model was introduced, 3048 patients with coronary artery disease, 5605 hypertensive patients, and 1984 patients with type 2 diabetes had already signed contracts with the community health centre and received public health services. After the grid management model was promoted, 614 patients with coronary artery disease, 752 hypertensive patients, and 301 patients with type 2 diabetes were newly included in the management program. However, as shown in Table 2, some patients who moved out of the jurisdiction, refused our services, and could not be included.
| Community healthy centre | Coronary artery disease | Hypertension | Type 2 diabetes | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient number (n) | Contract signed (n, %) | New contract (n, %) | Unable to include (n, %) | Patient number (n) | Contract signed (n, %) | New contract (n, %) | Unable to include (n, %) | Patient number (n) | Contract signed (n, %) | New contract (n, %) | Unable to include (n, %) | ||
| Xin Pu Cheng | 427 | 216 (50.59) | 67 (15.69) | 144 (33.72) | 634 | 358 (56.47) | 66 (10.41) | 210 (33.12) | 256 | 126 (49.22) | 24 (9.38) | 106 (41.41) | |
| Zhao Si Wu | 138 | 108 (78.26) | 14 (10.14) | 16 (11.59) | 376 | 273 (72.61) | 23 (6.12) | 80 (21.28) | 154 | 94 (61.04) | 11 (7.14) | 49 (31.82) | |
| Niu Wang | 456 | 366 (80.26) | 17 (3.73) | 73 (16.01) | 643 | 539 (83.83) | 24 (3.73) | 80 (12.44) | 265 | 197 (74.34) | 13 (4.91) | 55 (20.75) | |
| Liu Kou | 324 | 223 (68.83) | 66 (20.37) | 35 (10.8) | 682 | 385 (56.45) | 88 (12.9) | 209 (30.65) | 276 | 146 (52.9) | 41 (14.86) | 89 (32.25) | |
| Wu Li | 518 | 214 (41.31) | 43 (8.3) | 261 (50.39) | 617 | 387 (62.72) | 45 (7.29) | 185 (29.98) | 279 | 168 (60.22) | 19 (6.81) | 92 (32.97) | |
| Lao Pu Cheng | 784 | 371 (47.32) | 83 (10.59) | 330 (42.09) | 1378 | 775 (56.24) | 129 (9.36) | 474 (34.4) | 465 | 236 (50.75) | 38 (8.17) | 191 (41.08) | |
| Gao Du | 749 | 350 (46.73) | 62 (8.28) | 337 (44.99) | 687 | 485 (70.6) | 54 (7.86) | 148 (21.54) | 287 | 191 (66.55) | 19 (6.62) | 77 (26.83) | |
| Peng Zhuang | 825 | 332 (40.24) | 41 (4.97) | 452 (54.79) | 1078 | 653 (60.58) | 62 (5.75) | 363 (33.67) | 342 | 181 (52.92) | 19 (5.56) | 142 (41.52) | |
| Nan Guan | 893 | 271 (30.35) | 122 (13.66) | 500 (55.99) | 1356 | 797 (58.78) | 175 (12.91) | 384 (28.32) | 508 | 272 (53.54) | 79 (15.55) | 157 (30.91) | |
| Xiao Guo | 984 | 597 (60.67) | 99 (10.06) | 288 (29.27) | 1256 | 953 (75.88) | 86 (6.85) | 217 (17.28) | 528 | 373 (70.64) | 38 (7.2) | 117 (22.16) | |
| Total | 6098 | 3048 (49.98) | 614 (10.07) | 2436 (39.95) | 8707 | 5605 (64.37) | 752 (8.64) | 2350 (26.99) | 3360 | 1984 (59.05) | 301 (8.96) | 1075 (31.99) | |
Patient number is derived from the community grid, district health bureau, and hospital information system. Contract signed is included in health management information before this grid management model was introduced. New contract means patients we administrated after this grid management model was introduced. Unable to administrate reasons include moving out of the jurisdiction, losing track, and refusing our services.
The health management rate has increased under the grid management model
After the implementation of grid management, the health management rate of not only the key patient groups such as those with hypertension, type 2 diabetes, and coronary artery disease but also the residents’ health files in the community health centres has significantly increased, as shown in Table 3. The number of residents’ health files has increased from 155,612 in 2022 to 374,250 in 2023; an increase of 140.50%. The number of health management personnel for hypertension patients increased from 4845 in 2022 to 7942 in 2023; an increase of 63.92%. The number of type 2 diabetes patients under health management increased from 1621 in 2022 to 2813 in 2023; an increase of 74.65%. The number of coronary artery disease patients under health management increased from 2050 in 2022 to 2911 in 2020; an increase of 42.00%.
| Community healthy centre | Resident health record | Coronary artery disease | Hypertension | Type 2 diabetes | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2022 | 2023 | Increase rate (%) | 2022 | 2023 | Increase rate (%) | 2022 | 2023 | Increase rate (%) | 2022 | 2023 | Increase rate (%) | ||||||||
| Management count | Standard management rate | Management count | Standard management rate | Management count | Standard management rate | Management count | Standard management rate | Management count | Standard management rate | Management count | Standard management rate | ||||||||
| Xin Pu Cheng | 13,864 | 30,653 | 121.10 | 167 | 57.92 | 194 | 62.85 | 16.17 | 365 | 65.15 | 548 | 60.54 | 50.14 | 128 | 50.69 | 229 | 65.16 | 78.91 | |
| Zhao Si Wu | 7923 | 16,984 | 114.36 | 118 | 50.33 | 169 | 67.77 | 43.22 | 246 | 42.87 | 356 | 58.28 | 44.72 | 97 | 57.78 | 128 | 77.26 | 31.96 | |
| Niu Wang | 15,834 | 33,856 | 113.82 | 238 | 67.82 | 328 | 61.91 | 37.82 | 443 | 68.30 | 675 | 59.54 | 52.37 | 136 | 67.34 | 258 | 64.27 | 89.71 | |
| Liu Kou | 12,945 | 30,876 | 138.52 | 168 | 46.50 | 243 | 59.97 | 44.64 | 337 | 52.54 | 582 | 57.43 | 72.7 | 125 | 40.45 | 228 | 62.51 | 82.4 | |
| Wu Li | 16,954 | 41,953 | 147.45 | 193 | 66.24 | 269 | 61.11 | 39.38 | 543 | 79.54 | 865 | 58.94 | 59.3 | 226 | 52.93 | 318 | 63.28 | 40.71 | |
| Lao Pu Cheng | 16,543 | 45,923 | 177.60 | 235 | 58.64 | 328 | 66.28 | 39.57 | 638 | 62.13 | 938 | 65.84 | 47.02 | 168 | 55.14 | 326 | 66.71 | 94.05 | |
| Gao Du | 12,853 | 37,954 | 195.29 | 184 | 54.25 | 285 | 58.85 | 54.89 | 417 | 45.76 | 724 | 57.43 | 73.62 | 136 | 62.74 | 247 | 60.26 | 81.62 | |
| Peng Zhuang | 14,987 | 46,723 | 211.76 | 194 | 46.71 | 293 | 59.88 | 51.03 | 521 | 38.43 | 917 | 57.32 | 76.01 | 135 | 54.98 | 238 | 62.43 | 76.3 | |
| Nan Guan | 20,753 | 46,563 | 124.37 | 259 | 68.90 | 378 | 63.33 | 45.95 | 734 | 68.34 | 1145 | 58.34 | 55.99 | 278 | 69.45 | 412 | 68.32 | 48.2 | |
| Xiao Guo | 22,956 | 42,765 | 86.29 | 294 | 65.74 | 424 | 58.40 | 44.22 | 729 | 73.04 | 1183 | 63.87 | 62.28 | 192 | 58.43 | 447 | 52.92 | 132.81 | |
| Total | 155,612 | 374,250 | 140.50 | 2050 | 59.68 | 2911 | 61.74 | 42.00 | 4973 | 61.86 | 7933 | 60.1 | 59.52 | 1621 | 58 | 2831 | 63.25 | 74.65 | |
Grid-based community proactive health management model may reduce hospitalisation of patients with chronic diseases
A hospitalisation investigation was carried out to assess benefits for contracted residents. After the implementation of grid management, the hospitalisation rate of patients with type 2 diabetes significantly decreased in 2023 (P < 0.05, Table 4), even though the number of signed patients rose. The hospitalisation rate of patients with coronary artery disease in 2023 was similar to that in 2022 (P > 0.05, Table 4). Hypertension patients exhibited a lower hospitalisation rate in 2023 compared to that in 2022; however, the difference was not statistically significant (P > 0.05, Table 4). Overall, a grid-based community proactive health management model may reduce hospitalisation of patients with chronic diseases.
| Community health centre | Coronary artery disease | Hypertension | Type 2 diabetes | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2022 | 2023 | 2022 | 2023 | 2022 | 2023 | ||||||||
| Management count | Hospitalisation count (n, %) | Management count | Hospitalisation count (n, %) | Management count | Hospitalisation count (n, %) | Management count | Hospitalisation count (n, %) | Management count | Hospitalisation count (n, %) | Management count | Hospitalisation count (n, %) | ||
| Xin Pu Cheng | 167 | 34 (20.36) | 194 | 29 (14.95) | 365 | 0 (0.00) | 548 | 2 (0.36) | 128 | 3 (2.34) | 229 | 5 (2.18) | |
| Zhao Si Wu | 118 | 12 (10.17) | 169 | 26 (15.38) | 246 | 6 (2.44) | 356 | 2 (0.56) | 97 | 4 (4.12) | 128 | 0 (0.00) | |
| Niu Wang | 238 | 41 (17.23) | 328 | 48 (14.63) | 443 | 1 (0.23) | 675 | 3 (0.44) | 136 | 1 (0.74) | 258 | 3 (1.16) | |
| Liu Kou | 168 | 21 (12.5) | 243 | 32 (13.17) | 337 | 0 (0.00) | 582 | 1 (0.17) | 125 | 5 (4.00) | 228 | 1 (0.44) | |
| Wu Li | 193 | 16 (8.29) | 269 | 27 (10.04) | 543 | 1 (0.18) | 865 | 3 (0.35) | 226 | 9 (3.98) | 318 | 4 (1.26) | |
| Lao Pu Cheng | 235 | 23 (9.79) | 328 | 28 (8.54) | 638 | 5 (0.78) | 938 | 2 (0.21) | 168 | 7 (4.17) | 326 | 5 (1.53) | |
| Gao Du | 184 | 14 (7.61) | 285 | 21 (7.37) | 417 | 1 (0.24) | 724 | 1 (0.14) | 136 | 3 (2.21) | 247 | 0 (0.00) | |
| Peng Zhuang | 194 | 9 (4.64) | 293 | 21 (7.17) | 521 | 2 (0.38) | 917 | 2 (0.22) | 135 | 0 (0.00) | 238 | 3 (1.26) | |
| Nan Guan | 259 | 25 (9.65) | 378 | 32 (8.47) | 734 | 5 (0.68) | 1145 | 2 (0.17) | 278 | 7 (2.52) | 412 | 0(0.00) | |
| Xiao Guo | 294 | 17 (5.78) | 424 | 28 (6.60) | 729 | 5 (0.69) | 1183 | 0 (0.00) | 192 | 0 (0.00) | 447 | 2 (0.45) | |
| Total | 2050 | 212 (10.34) | 2911 | 292 (10.03) | 4973 | 26 (0.52) | 7933 | 18 (0.23) | 1621 | 39 (2.41) | 2831 | 23 (0.81) | |
| P-value A | 0.912 | 0.279 | 0.034* | ||||||||||
Discussion
Grid management of family doctors has expanded the coverage of national basic public health services and family doctor contracted services
After the implementation of grid management, both the management rate and enrolment rate in the case area have increased significantly, including residents’ health files, along with the number of hypertension, type 2 diabetes and coronary artery disease patients. There are two main reasons for the improvement in enrolment and participation. First, grid management fully leverages the work characteristics of community grid members by consolidating the family doctor team. While carrying out grid work, grid members actively promote national basic public health services by using systematic home-based follow-up appointments, improving accessibility to public health services. The second is the precise management of the family doctor team in different areas, with each team responsible for the health management of key populations in several grids of the area. The grid organisation exchanges data with the social health centre on key populations, and the family doctor team track and monitors the key populations in the area that have not been provided services. This method is a change from the previous social health centre approach that waited for residents to seek health services, to the family doctor team actively going out to provide national basic public health services with prevention as the focus. This has made up for the blind spots in the country’s basic public health services.
Annual hospitalisation rates in key populations do not fully define the benefits of the community proactive health management model
First, better blood glucose control reduces the risk of hospitalisation for infections in diabetes patients (Khalifa et al. 2023). After the implementation of grid management, the blood glucose levels of diabetic patients have become more stable. This may be why the hospitalisation rate in 2023 (0.81% per year) is lower than that for 2022 (2.41% per year). Second, the grid-based community proactive health management model did improve treatment compliance in patients with coronary artery disease; however, the hospitalisation rate of these patients in 2023 was similar to that in 2022. Our investigation found that with the promotion of health education and family follow-up assessment, several patients who did not consciously receive secondary prevention for coronary artery disease and lipid monitoring were actively hospitalised for coronary artery assessment. Third, hypertension patients exhibited a lower hospitalisation rate in 2023 compared to those in 2022; however, the difference was not statistically significant. Stroke, myocardial infarction, and heart failure are acute complications of hypertension, but the incidence is approximately 1/10,000 (Dzau and Hodgkinson 2024). The hospitalisation rate alone cannot define the benefit to consumers. More evaluation indicators are needed to evaluate the control of other hypertensive complications, including renal failure and retinopathy.
The content of grid management for family doctors needs to be enriched
Currently, the family doctor team in this street has enhanced the number of grid members in the area, and grid management has achieved full coverage of these residential areas. However, there are many enterprises and schools in the jurisdiction of this street, and they had not yet joined the grid management model at the time of writing. It is also the case that the current implementation of grid management mainly focuses on the health management of patients with hypertension, type 2 diabetes, and coronary artery disease, as well as the services to which their family doctors have signed. The services do not cover the whole population age range.
Suggestions for improving team building and enriching the benefits and advantages of grid management
The next step is to further improve the grid management team of family doctors. Based on incorporating grid members and community volunteers into the family doctor team, we are considering the inclusion of school doctors and enterprise medical staff in the family doctor team of the social health centre. Through the promotion of national basic public health services by school and enterprise internal medical staff, we can enhance the implementation effect of national basic public health services in schools and enterprises. In addition, the content of grid management services could be expanded. Since 2018, Shenzhen has been exploring community grid institutions, community workstations, police districts, and other community organisations to participate in the health management of patients with severe mental disorders and has achieved good results. We intend to learn from the successful experience of grid-based health management for the existing coronary artery disease, hypertension, and type 2 diabetes patients and gradually expand the national basic public health services offered, such as health management for children aged 0–6 years, maternal health management, vaccination services, health education, and health literacy improvement services, to further broaden the service content of grid-based management provided by family doctors.
Data availability
The data that support this study cannot be publicly shared due to ethical or privacy reasons and may be shared upon reasonable request to the corresponding author if appropriate.
References
Aghagoli G, Gallo Marin B, Soliman LB, Sellke FW (2020) Cardiac involvement in COVID-19 patients: risk factors, predictors, and complications: a review. Journal of Cardiac Surgery 35, 1302-1305.
| Crossref | Google Scholar | PubMed |
Bangura MS, Gonzalez MJ, Ali NM, Ren R, Qiao Y (2020) A collaborative effort of China in combating COVID-19. Global Health Research and Policy 5, 47.
| Crossref | Google Scholar | PubMed |
Brotons P, Virumbrales M, Elorduy M, et al. (2020) Perceptions of students confined by the COVID-19 pandemic on distance learning in medicine. Revista Médica de Chile 148, 1461-1466.
| Crossref | Google Scholar | PubMed |
Cheng YD, Yu J, Shen Y, Huang B (2020) Coproducing responses to COVID-19 with community-based organizations: lessons from Zhejiang Province, China. Public Administration Review 80, 866-873.
| Crossref | Google Scholar | PubMed |
Dzau VJ, Hodgkinson CP (2024) Precision hypertension. Hypertension 81, 702-708.
| Crossref | Google Scholar | PubMed |
Guo LX, Yu SW, Feng JJ (2019) Analysis and optimization of development model of community sports public service under the perspective of active health. Journal of Shijiazhuang University 21, 102-106.
| Google Scholar |
He B, Guo H, Wang J (2019) Basic public health services in Jiangsu province to save the problems in research. Chinese Social Medical Journal 4, 190-193 [In Chinese].
| Google Scholar |
Hu C, Huang X (2020) City residents signing the family doctor service satisfaction survey and influence factors analysis. Journal of General Practice Medicine in China 11, 119-122 [In Chinese].
| Google Scholar |
Khalifa WA, Argoon SA, AbdEllah-Alawi MHM (2023) Determinants of healing of diabetic foot ulcer comparing two offloading modalities: a randomized prospective study. The Foot 56, 102016.
| Crossref | Google Scholar | PubMed |
Li XC, Yu MS (2020) Proactive health: from idea to model. China Sport Science 40, 83-89.
| Google Scholar |
Liu Z, Wang Z, Ouyang C (2019) Current situation analysis and mechanism optimization of grid management for epidemic prevention and control in urban communities. Chinese Journal of Social Medicine 37, 577-580 [In Chinese].
| Google Scholar |
Liu Z, Lin S, Shen Y, Lu T (2021) Collaborative neighborhood governance and its effectiveness in community mitigation to COVID-19 pandemic: from the perspective of community workers in six Chinese cities. Cities 116, 103274.
| Crossref | Google Scholar | PubMed |
Núñez-Gil IJ, Fernández-Ortiz A, Maroud Eid C, et al. (2021) Underlying heart diseases and acute COVID-19 outcomes. Cardiology Journal 28, 202-214.
| Crossref | Google Scholar | PubMed |
Pavel M, Jimison HB, Korhonen I, Gordon CM, Saranummi N (2015) Behavioral informatics and computational modeling in support of proactive health management and care. IEEE Transactions on Biomedical Engineering 62, 2763-2775.
| Crossref | Google Scholar | PubMed |
Ren J, Li J, Ni N (2018) Community health service grid management pattern exploration. Chinese Community Physicians 1135, 189-191 [in Chinese].
| Google Scholar |
Teuwen L-A, Geldhof V, Pasut A, Carmeliet P (2020) COVID-19: the vasculature unleashed. Nature Reviews Immunology 20, 389-391.
| Crossref | Google Scholar | PubMed |
Wang D, Hu B, Hu C, et al. (2020a) Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 323, 1061-1069.
| Crossref | Google Scholar | PubMed |
Wang D, Wang H, Liu G (2020b) Investigation on residents’ awareness rate and satisfaction degree of key population of national basic public health service project in Shenzhen. Modern Preventive Medicine 47, 1035-1038 [In Chinese].
| Google Scholar |
Yan D, Duan X, Wang Q (2020) Practice of prevention and control of novel coronavirus pneumonia in community health service institutions under the primary medical group system. Practical Cardio-Cerebral Pulmonary Vascular Disease 28, 15-20 [In Chinese].
| Google Scholar |
Ye TT, Zhao YW, Wang XS, Ling YH, Wang H (2021) Research on community chronic disease management model based on the concept of “active health”. Health Economic Research 38, 45-48.
| Google Scholar |
Zheng M, Li Q, Zhang Y (2018) Analysis on health status and health service demand of the elderly aged 65 and above in Futian District, Shenzhen. Chinese Social Medical Journal 35, 87-90 [In Chinese].
| Google Scholar |
Zheng Y-Y, Ma Y-T, Zhang J-Y, Xie X (2020) COVID-19 and the cardiovascular system. Nature Reviews Cardiology 17, 259-260.
| Crossref | Google Scholar | PubMed |