The paramedic–general practitioner relationship: a scoping review
Sarah Petschack A , Robert Lasslett A * and Linda Ross A
A * and Linda Ross A
A Department of Paramedicine, Monash University, Frankston, Vic. 3199, Australia.
Australian Journal of Primary Health - https://doi.org/10.1071/PY23060
Submitted: 23 March 2023 Accepted: 20 July 2023 Published online: 14 August 2023
© 2023 The Author(s) (or their employer(s)). Published by CSIRO Publishing on behalf of La Trobe University. This is an open access article distributed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND)
Abstract
Background: Health services internationally are implementing programs that increase working ties between paramedics and general practitioners (GPs) to reduce unnecessary transport to emergency departments (EDs) and improve access to primary health care. As paramedic involvement in primary health care develops, there is increasing focus on the GP–paramedic collaborative relationship. Resulting issues regarding professional boundaries may occur, as paramedics practice in fields that were previously solely in the GP scope. An effective paramedic-GP working relationship will be an essential foundation to the success of future strategies.
Methods: A search of three electronic databases was completed (Ovid MEDLINE, Embase Classic + Embase and CINAHL Plus). Eligibility for inclusion required analysis of the relationship between paramedics and GPs. All processes were completed by two independent reviewers.
Results: After removal of duplicates, 4995 titles were screened by title and/or abstract. After full-text review, 15 studies were included. Five themes were identified that contribute significantly to the strengths and weaknesses of the relationship – the importance of communication, understanding scope of practice, leadership roles, responsibility for patient care and interdisciplinary training. Issues identified included significant variation in the structure of different emergency medical services and varying standards of education requirements for paramedics worldwide.
Conclusions: There were no published Australian studies that had the primary aim of examining the paramedic–GP relationship. The depth of research on this topic is lacking, despite increased interest over the past decade. The relevance of the international literature to the Australian setting is questionable.
Keywords: ambulance, collaboration, community, connected care, general practitioner, paramedics, primary health care, relationship.
Introduction
International demand for acute and non-acute health services continues to increase (Willson et al. 2022), with current models of health care provision considered unsustainable (Montgomery et al. 2017). Emergency departments (EDs) and jurisdictional ambulance services are frequently under-resourced and overstretched (He et al. 2011; Montgomery et al. 2017; Willson et al. 2022) – issues that are echoed in primary health care (PHC) (Mahtani et al. 2018; Eaton et al. 2020; Schofield et al. 2020). Up to 40% of lower-acuity ED presentations may be avoidable, providing the patient has suitable and timely access to PHC (Ismail et al. 2013; Willson et al. 2022). A high proportion of ambulance workload is made up of non-life-threatening concerns, potentially appropriate for management by PHC teams (Eastwood et al. 2016; 2020; Eaton et al. 2020).
The role of the Australian paramedic has evolved significantly over the past decade (Eastwood et al. 2016; Eaton et al. 2020). This expansion includes an increase in the scope of practice, introduction of professional registration and well-established tertiary education requirements (O’Meara et al. 2012; Eaton et al. 2020; Reaburn 2020). The paramedic caseload is increasingly comprised of low-acuity/PHC-suitable presentations, leading to changes in expectations of how paramedics assess and manage these patients (Eastwood et al. 2020; Eaton et al. 2020; Wagstaff and Mistry 2020). There is an increasing requirement for the paramedic role to encompass the confidence and competence to be selective with patient selection for transportation to EDs (Paulin et al. 2021), driven by EDs in Australia and abroad struggling with department congestion, long wait times and ambulance ramping (He et al. 2011; Finn et al. 2013; Willson et al. 2022). These challenges have driven a need for paramedics to, when appropriate, avoid patient transportation to EDs, utilising alternative patient care pathways, with the conveyance of all ambulance cases to an ED now considered an outdated and unsustainable practice (Blodgett et al. 2021; Paulin et al. 2021).
PHC services are also facing challenges in achieving adequate care for those in the community (O’Meara et al. 2012; Currie et al. 2020; Eaton et al. 2021a). There is a link between potentially avoidable hospitalisations and accessibility and effectiveness of PHC (Katteryl et al. 2012), and inappropriate patient transport to an ED may delay timely access to primary care (Eastwood et al. 2016). The combined pressures on both acute and non-acute health services have led to attempts to prevent unnecessary ambulance transport to EDs. Many organisations are trialling and implementing strategies, such as embedding paramedics within PHC teams or the implementation of paramedic referral pathways (Blodgett et al. 2017, 2020; Eaton et al. 2021a), the intent of which includes increasing patient satisfaction and reduction of burden on EDs. These novel approaches appear to increase collaboration between paramedics and those working in PHC, most frequently GPs (Bury et al. 2006). It is therefore valid to consider the importance of this professional relationship as an essential foundation to these strategies.
The cornerstone of safe and effective patient care relies on sound teamwork and communication (Manser 2009; Rosen et al. 2018); therefore, the relationship between paramedics and GPs can be considered critical to the safety and efficacy of these pathways. The paramedic-GP relationship is not novel – GPs have historically interacted with paramedics through paramedic attendance at PHC clinics for patients requiring emergency care and transport to an ED. Much of the relationship has therefore been under different circumstances to what is now occurring, with a shift towards joint patient care efforts for the non-acute patient. To overcome the challenges and optimise opportunities for best patient care, developing a robust understanding of the relationship is vital for future cooperation.
The aim of this scoping review was to describe and analyse literature that has examined the paramedic–GP relationship.
Methods
Eligibility criteria/developing the search strategy
This literature review was conducted in accordance with the JBI methodology for scoping reviews (Peters et al. 2017). The search strategy used aimed to locate both published and unpublished studies that analysed the relationship between and paramedics and GPs. An initial limited search of MEDLINE and Google Scholar was undertaken to identify articles on the topic. The text words contained in the titles and abstracts of potentially relevant studies, and the index terms used to describe the studies were used to develop a comprehensive search strategy. The paramedic-specific search filter created by Olaussen et al. that is optimised for sensitivity was utilised in the strategy (Olaussen et al. 2017).
The Population/Concept/Context search strategy framework was initially utilised to categorise terms (Peters et al. 2017). After some piloted searches, the decision was made to exclude the context category (out-of-hospital/prehospital) to prevent the inadvertent exclusion of potentially relevant literature.
The searches were not restricted by year or country of publishing. All historical evidence was included without reference to year of publishing exclusion criteria, as there was no discernible timeframe that the analysis of the relationship in question was either more or less relevant. As the findings of initial searches revealed limited Australian studies, international literature was included, so long as they were available in English, despite there being variance in the structure of health care settings, and training and scope of paramedics.
Information sources
In March 2022, systematic searches were completed using the following electronic bibliographic databases: Ovid MEDLINE, Embase Classic + Embase and CINAHL Plus (EBSCOhost). The final search strategy used for Ovid MEDLINE is shown in Appendix 1. The reference lists of all included sources of evidence were screened for any additional studies that met the inclusion criteria. References of papers that were excluded due to being literature reviews were scanned to capture any further relevant papers.
Data charting process
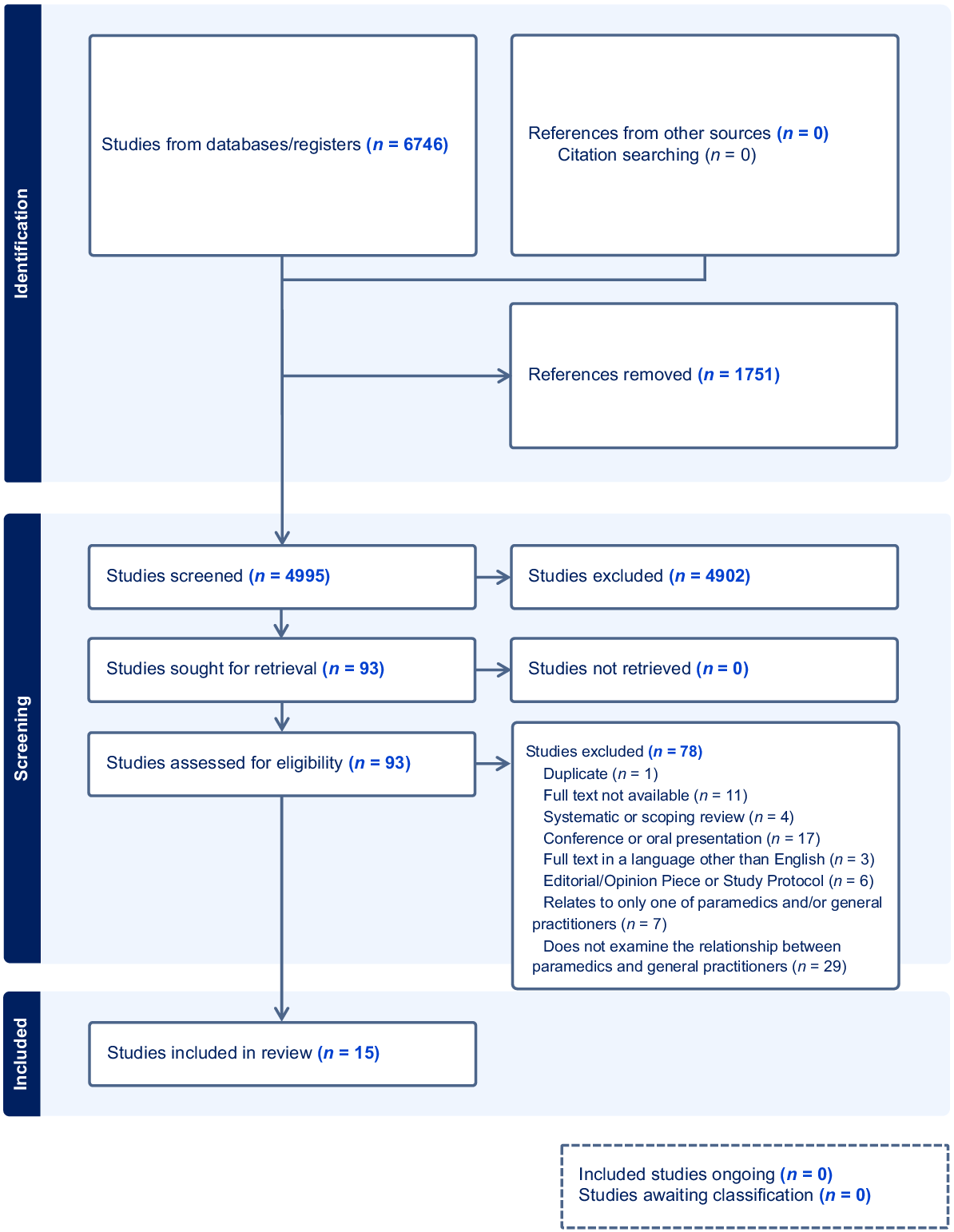
Following the completed searches, all identified citations were collated and uploaded into EndNote Version 8 (IBM). Citations were then imported into Covidence systematic review software (Veritas Health Innovation), and duplicates were removed automatically by the software or manually, as required. Titles and abstracts were screened by two independent reviewers (SP and RL) for assessment against the inclusion criteria. Potentially relevant sources were retrieved in full text and imported. Full-text screening was completed by the same two reviewers, with the final inclusion/exclusion criteria, shown in Table 1. Any conflicts that occurred throughout the review process were resolved through discussion between SP and RL with the assistance of the third author (LR), as required. The results of the search and study inclusion process are reported in a PRISMA-ScR flow diagram.
| Inclusion | Exclusion |
|---|---|
Paramedics and general practitioners Relating to working relationship Full text available in English | Does not examine the relationship between paramedics and general practitioners Editorial/opinion piece or study protocol Systematic or scoping review Conference or oral presentation Full text not available Full text not available in English Duplicate |
Data items
Data were extracted from papers included in the review by two independent reviewers (SP and RL) using a data extraction template developed by the reviewing team. The data extraction included specific details: author, year/country of publishing, purpose/aim of study, participants, methodology and key findings relevant to the review question.
Quality assessment
The Quality Assessment with Diverse Studies appraisal tool was used to evaluate the methodological rigour of the included studies. This tool was chosen due to the heterogeneity of study types included in this review, and proven strong reliability and validity, especially when used for the appraisal of multi- or mixed-methods health services research (Harrison et al. 2021). Each of the 13 criteria were awarded a score between 0 and 3, which were then summed and converted to an overall percentage. The quality assessment was completed by two independent reviewers (SP and RL), and conflicts were resolved through discussion between the reviewers.
Synthesis of results
Analysis of the studies was completed by two independent researchers (SP and RL). Following the extraction of the basic characteristics, a more detailed extraction of the relevant study findings was completed. The two researchers reviewed both individual data charts, and subsequently further discussed any differences in the synthesis of the evidence. A concept map was used to categorise and condense the results, and to organise the key themes found in the literature.
Results
Selection of sources of evidence
An initial search of three databases resulted in 6746 studies. Following the removal of duplicates, 4995 studies remained. After title and abstract review, 93 studies remained, with 15 studies remaining after full-text review. No further studies were identified through both grey literature searching and backwards citation searching of included studies. A study selection overview is shown in Fig. 1.
Characteristics of sources of evidence
A detailed breakdown of the characteristics of the included studies can be seen in Table 2, with a summary of the main results of the individual studies in Table 3. Six studies were from the UK, three from Norway, two each from Australia and Ireland, and one each from the USA and Denmark. Eight of the included studies used a qualitative methodology study design. The next most common methodology was quantitative, with four studies utilising a cross-sectional study in the form of a questionnaire. The included studies were published between the years of 2006–2021. A total of 13 of the 15 included studies were published within the past decade, with eight of these being published since 2018.
| Author(s) | Year | Country | Purpose | Participants (n) | Study Design | QuADS score (%) |
|---|---|---|---|---|---|---|
| Blodgett et al. | 2017 | UK | Analysis of barriers and motivators of a prehospital GP referral system from the paramedic perspective | Paramedics (n = 8) | Mixed qualitative observational study using informal, semi-structured interviews via grounded theory | 33 (85%) |
| Burns | 2018 | UK | Seek the GP perspective regarding paramedics providing referrals to urgent/primary care | GPs (n = 7) | Qualitative, semi-structured interviews using a phenomenological approach with purposive sampling. | 21 (54%) |
| Bury et al. | 2006 | Ireland | Explore perceptions of GPs and EMTs of each other’s roles in managing community emergencies | GPs (n = 369), EMTs (n = 226) | Quantitative, anonymous questionnaire of GPs and EMTs within regions, 4-point scale for agreement. | 27 (69%) |
| Eaton et al. | 2021 | UK | Design and evaluate an education framework to support APPs transitioning into primary care | APPs (n = 7) GPs (n = 4) | Qualitative, semi-structured focus groups using naturistic enquiry methodology in collective groups | 29 (74%) |
| Forland et al. | 2009 | Norway | Analyse how ambulance workers perceive their competence in managing prehospital emergencies compared with other professions | Ambulance workers (n = 156) | Questionnaires with two groups of ambulance workers. | 28 (72%) |
| Hjortdahl et al. | 2014 | Norway | Gain insight into EMTs’ experience working alongside GPs in prehospital emergency care. | EMTs (n = 5–9 × 4) | Focus group interviews | 29 (74%) |
| Lazarsfeld-Jensen et al. | 2014 | Australia | Evaluation of interprofessional simulation-based education between GPs and paramedics | GPs (n = 5) Paramedics/nurses/students (n = 11) | Multi-method qualitative review with observation of simulated scripted scenarios | 32 (82%) |
| Mieritz et al. | 2018 | Denmark | Evaluate communication between GPs and emergency dispatch staff when organising emergency ambulance cases | Calls (n = 1334) | Retrospective analysis of calls where GPs requested an emergency ambulance | 34 (87%) |
| Myers et al. | 2020 | USA | Analysis of a community paramedicine program to review overall GP satisfaction with the program | GPs (n = 18) | Online survey of GPs with direct involvement in referral to the program (one element of total study) | 32 (82%) |
| Nystoyl et al. | 2018 | Norway | Examine collaboration between ambulance workers and GPs in clinical management of prehospital patients | Missions (n = 172) Patients (n = 180) | Retrospective observational study | 31 (80%) |
| O’Meara et al. | 2016 | Australia | Identification and analysis of how paramedics create and maintain professional boundaries while working in community paramedicine | 3 × focus groups (10–20 participants each) | Multi-method approach including observation of practice, informal discussion, interviews and focus groups | 34 (87%) |
| Power et al. | 2020 | Ireland | Understand GP opinion on changes to clinical pathways enabling paramedics to treat and refer to GPs | GPs (n = 39) | Survey divided into four domains | 35 (90%) |
| Proctor | 2019 | UK | Review student paramedics’ views on incorporating placements in GP clinics on their paramedicine degree | Paramedic students (n = 6) | Pedagogic study including case study, semi-structured interviews and thematic analysis | 32 (82%) |
| Schofield et al. | 2020 | UK | Explore how paramedics can be utilised to work in general practice | Paramedics (n = 81) GPs (n = 40) | Mixed methods scoping study with literature review, mixed format national survey and interviews | 35 (90%) |
| Villarreal et al. | 2017 | UK | Investigate whether co-responding GPs to emergency calls reduces transports to ED | Cases (n = 1903) | Prospective study of patients who are deemed to be suitable for GP assessment in the field | 31 (80%) |
UK, United Kingdom; USA, United States of America; EMT, emergency medical technician; GP, general practitioner; APP, advanced paramedic practitioner; QuaDS, Quality Assessment with Diverse Studies.
| Author(s) | Summary of main results |
|---|---|
| |
Burns (2018), UK |
|
Bury et al. (2006), Ireland |
|
| |
Forland et al. (2009), Norway |
|
Hjortdahl et al. (2014), Norway |
|
Lazarsfeld-Jensen and Bridges (2014), Australia | |
Mieritz et al. (2018), Denmark | |
Myers et al. (2020), USA |
|
Nystøyl et al. (2018), Norway | |
O’Meara et al. (2015), Australia | |
Power and Bury (2020), Ireland |
|
Proctor (2019), UK |
|
| |
|
EMT, emergency medical technician; GP, general practitioner; APP, advanced paramedic practitioner.
Quality assessment
The mean Quality Assessment with Diverse Studies score was 79.0% (range 53.8–89.7%). Studies generally performed well on items relating to the theoretical or conceptual underpinning of the research, the description of the research setting and target population, and the appropriateness of the method of analysis to meet the research aim/s. Items relating to justification for the analytic method selection and consideration of research stakeholders in the study design were generally less well considered. The Quality Assessment with Diverse Studies scores are listed in Table 2.
Synthesis of results
The analysis of the studies identified that the perceived strengths and weaknesses of the relationship have five key themes: the importance of communication, concerns relating to scope of practice, leadership roles, responsibility for patient care, and the significance of interdisciplinary training and feedback.
The perceived standard of communication between the two working groups varied, with GPs more likely to report concerns around paramedic use of tone, whereas paramedics were more likely to report issues associated with a general lack of communication (Blodgett et al. 2017; Burns 2018). Three studies reported that both the paramedics and GPs thought that communication was rarely problematic, and allowed for cohesive multidisciplinary models of care (Villarreal et al. 2017; Mieritz et al. 2018; Myers et al. 2020). Two papers found that poor communication could contribute significantly to issues and barriers within the working relationship (Blodgett, Robertson et al. 2017; Burns 2018). Experiences of suboptimal communication were reported by both paramedics and GPs.
Understanding and agreement of scope of practice was found to be a contributing factor to issues within the relationship, primarily from a GP perspective, with concerns regarding paramedic scope of practice and knowledge. Two studies from the GP perspective found that strain on the relationship occurred when doctors felt that paramedics were practicing outside their scope (Burns 2018; Eaton et al. 2021b). Both qualitative and cross-sectional studies identified GP concerns with perceived paramedic knowledge gaps and reported lack of confidence in paramedics safely practicing within a recently expanded scope of practice (Hjortdahl et al. 2014; Mieritz et al. 2018; Schofield et al. 2020). O’Meara et al. highlighted that having paramedics practicing outside the historically accepted scope of their practice and/or shifting into the expanded area of PHC crosses professional boundaries (O’Meara et al. 2015). Lazarsfield-Jenson et al. found that focusing on interdisciplinary simulation training increased the overall understanding of each other’s scope of practice, aligning with overall improvements within the relationship (Lazarsfeld-Jensen and Bridges 2014).
It was found that lack of clarity around professional roles, and ambiguity around leadership, contributed negatively to the paramedic relationship, with the importance of clinical leadership within the relationship being a reccurring theme. Where Scandinavian GPs were required to respond to emergency incidents in the community, paramedics/emergency medical technicians expressed their belief that the GPs should act as scene leaders, while also identifying a potential correlation of perceived substandard GP leadership, leading to poor cooperation in this context (Forland et al. 2009; Hjortdahl et al. 2014).
Multiple qualitative studies identified responsibility for patient care as an issue on both sides of the relationship (Blodgett et al. 2017; Burns 2018). Paramedics reported frustration that GPs were sometimes unwilling to take on referrals of some patients, perceiving that the doctors were afraid to take on a reasonable level of responsibility for patient care (Blodgett et al. 2017). GPs reported a sense that paramedics occasionally used professional collaboration to shift the burden of responsibility for patient care to GPs and were not focused on an appropriate team based model of care (Burns 2018).
The importance of interdisciplinary training and feedback through shared learning as a means of strengthening the relationship between paramedics and GPs was identified, with consistent reference only to the value of feedback from GP to paramedic, with no mention of the converse. Shared learning was addressed in six studies, often with focus on professional feedback. Studies from the paramedic perspective highlighted the importance of receiving feedback from GPs, especially for paramedics transitioning to work within PHC teams (Hjortdahl et al. 2014; Blodgett et al. 2017; Eaton et al. 2021b). Variations in paramedic and GP perception of the adequacy of feedback and mentorship were identified. GPs tended to believe that feedback and supervision was sufficient, but paramedics believed that current practices did not optimise their individual practice nor their ability to collaborate successfully (Blodgett et al. 2017; Burns 2018; Eaton et al. 2021b). There was agreement that professional respect is enhanced through interdisciplinary training, while also finding that empathy for the professional challenges of each discipline is improved with increased awareness of professional skill sets (Bury et al. 2006; Hjortdahl et al. 2014; Lazarsfeld-Jensen and Bridges 2014; Proctor 2019).
Discussion
In some cases, the value of the study to the Australian context was questionable. Scandinavian studies involved an Emergency Medical Services (EMS) configuration where paramedics and GPs work alongside each other in the community emergency response setting – an uncommon scenario within Australia. These studies found that staff reflected more positively on the relationship when compared with studies that investigated the relationship where paramedics and GPs did not work together in a single service (Forland et al. 2009; Hjortdahl et al. 2014; Mieritz et al. 2018; Nystøyl et al. 2018). Examining the experience of the relationship in a variety of settings is essential to best inform future collaborative efforts. The question of whether the two professions should be participating together in a single episode of patient care, and in what capacity, is unresolved and key to directing the future of the relationship.
An identified theme relating to transfer of patient care responsibility was complex to analyse. Multiple contributing factors included poor communication, and a lack of trust and understanding of each other’s scope of practice, collectively contributing to issues surrounding responsibility for patient care. It is reasonable to infer that if a GP perceives a paramedic to lack the necessary skills in patient assessment, they may feel uncomfortable receiving a paramedic patient referral and the transfer of the associated responsibility. Although there was a perception in the literature that understanding of scope of practice underpins interdisciplinary trust, there was no examination of the exact nature of the scope of practice knowledge issue with sufficient detail.
The importance of interdisciplinary training to improve interprofessional understanding and empathy was highlighted throughout the literature (Hjortdahl et al. 2014; Lazarsfeld-Jensen and Bridges 2014; Proctor 2019; Eaton et al. 2021b). Multiple studies specifically detailed the desire of paramedics to receive more feedback from GPs (Blodgett et al. 2017; Eaton et al. 2021b). The concept of paramedics providing feedback to GPs was not discussed in any examined literature. This may be indirectly attributable to entrenched medical hierarchy, based on the belief that the more extensive training of the GP makes it inappropriate for paramedics to give feedback. Effective feedback has been found to be one of the most important factors for improving multidisciplinary teamwork (Salas et al. 2018). Therefore, in any model of care that relies on the collaboration of two different professions, opportunities for two-way feedback are vital.
The importance and value of the paramedic–GP relationship is expressed through the notion that a singular negative encounter or interaction between disciplines can have lasting impact on future effective cooperation (Blodgett et al. 2017). Successfully establishing health care services that rely on collaboration between the two professions will be enhanced by addressing any existing challenges and barriers to a closer working relationship (O’Meara et al. 2015).
Ten of the studies were published in the UK and Scandinavia, which suggests that other countries have been more innovative in health service provision and expanded paramedic involvement. In the UK, one of the driving factors for paramedics working within PHC teams is workforce shortages within traditional PHC professions, including GPs (Montgomery et al. 2017; Eaton et al. 2021a). Australian demand for both acute and nonacute health care is also increasing at a concerning rate (FitzGerald et al. 2012; Currie et al. 2020). There are ongoing challenges associated with the unequal distribution of health professionals, including GPs, needed to meet rural/remote Australia PHC demands (O’Meara et al. 2012; Currie et al. 2020). As overall demand for PHC services increases in Australia, there will be the subsequent need for reform of models of care that may require further collaboration between paramedics and GPs. Key potential challenges for future paramedic involvement in Australian primary care will include ensuring that patient care does not become fragmented, that the quality and safety of PHC is not diluted, and understanding if and how GPs will be provided with time, funding, and appropriate methodology to mentor/supervise/educate paramedics.
Summarising the overall state of the relationship was limited by inconsistences in the literature and the absence of collaborative studies comparing acute and nonacute settings. The majority of studies evaluated individual experiences of the relationship in one setting; for example, both paramedics’ and GPs’ involvement in a referral scheme or paramedics embedded in a GP clinic. As such, the included studies lack the depth required to deeply understand the relationship, as it exists across multifaceted environments of clinical practice, whereby the groups may interact in the community, hospitals or a PHC – any of which might involve the care of acute or non-acute patients.
Significant variation in the training level and scope of practice of the paramedic is observed in the included studies. The search criteria included all potential terms pertaining to paramedic, including emergency medical technician/ambulance officer and so on, accepting that there are vast differences in the education standards for these roles. As Australia predominantly has a tertiary education entry requirement for state-based ambulance services (Reaburn 2020), it could be argued that some of the literature is not representative of the Australian paramedic–GP relationship. Another limitation of this review was access to full-text articles. There was a total of 16 articles that were not accessible in full-text version, and it is therefore possible that some relevant literature has been omitted from this review.
There is a need for an Australian-based study that examines the relationship between paramedics and GPs that would ideally investigate both perspectives. To achieve holistic understanding, there needs to be an investigation of how these two professional groups interact within and outside of PHCs. The findings of this research could inform the development of collaborative models of care that optimise relevant skill sets. Reform in this area could potentially improve outcomes for patients and health care services.
As models of care evolve, interest in the GP–paramedic relationship is increasing. This review found five main themes contributing to the relationship – the importance of communication, understanding each other’s scope of practice, leadership roles, responsibility for patient care and the significance of interdisciplinary training. Internationally, paramedic involvement in PHC is increasing, with an aim to avoid unnecessary ED transport and improve access to PHC for patients. Further investigation of the Australian context is required to optimise both current and future interdisciplinary collaborations and relationships.
References
Blodgett J, Robertson D, Ratcliffe D, Rockwood K (2017) Creating a safety net for patients in crisis: paramedic perspectives towards a GP referral scheme. Journal of Paramedic Practice 9, 11-17.
| Crossref | Google Scholar |
Blodgett JM, Robertson DJ, Ratcliffe D, Rockwood K (2020) Piloting data linkage in a prospective cohort study of a GP referral scheme to avoid unnecessary emergency department conveyance. BMC Emergency Medicine 20(1), 48.
| Crossref | Google Scholar |
Blodgett JM, Robertson DJ, Pennington E, Ratcliffe D, Rockwood K (2021) Alternatives to direct emergency department conveyance of ambulance patients: a scoping review of the evidence. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine 29, 4.
| Crossref | Google Scholar |
Burns J (2018) GP perspectives of paramedic referrals to urgent and primary care. Journal of Paramedic Practice 10, 284-289.
| Crossref | Google Scholar |
Bury G, Egan M, Reddy L (2006) EMTs and GPs: what do we think of each other? Emergency Medicine Journal 23(7), 534-536.
| Crossref | Google Scholar |
Currie J, Carter MA, Lutze M, Edwards L (2020) Preparing Australian nurse practitioners to meet health care demand. The Journal for Nurse Practitioners 16, 629-633.
| Crossref | Google Scholar |
Eastwood K, Morgans A, Smith K, Hodgkinson A, Becker G, Stoelwinder J (2016) A novel approach for managing the growing demand for ambulance services by low-acuity patients. Australian Health Review 40(4), 378-384.
| Crossref | Google Scholar |
Eastwood K, Morgans A, Smith K (2020) Characteristics associated with emergency department suitability in low-acuity ambulance cases. Australasian Journal of Paramedicine 17, 1-9.
| Crossref | Google Scholar |
Eaton G, Wong G, Williams V, Roberts N, Mahtani KR (2020) Contribution of paramedics in primary and urgent care: a systematic review. British Journal of General Practice 70(695), e421-e426.
| Crossref | Google Scholar |
Eaton G, Wong G, Tierney S, Roberts N, Williams V, Mahtani KR (2021a) Understanding the role of the paramedic in primary care: a realist review. BMC Medicine 19(1), 145.
| Crossref | Google Scholar |
Eaton G, Happs I, Tanner R (2021b) Designing and implementing an educational framework for advanced paramedic practitioners rotating into primary care in North Wales. Education for Primary Care 32(5), 289-295.
| Crossref | Google Scholar |
Finn JC, Fatovich DM, Arendts G, Mountain D, Tohira H, Williams TA, Sprivulis P, Celenza A, Ahern T, Bremner AP, Cameron P, Borland ML, Rogers IR, Jacobs IG (2013) Evidence-based paramedic models of care to reduce unnecessary emergency department attendance – feasibility and safety. BMC Emergency Medicine 13, 13.
| Crossref | Google Scholar |
FitzGerald G, Toloo S, Rego J, Ting J, Aitken P, Tippett V (2012) Demand for public hospital emergency department services in Australia: 2000–2001 to 2009–2010. Emergency Medicine Australasia 24, 72-78.
| Crossref | Google Scholar |
Forland O, Zakariassen E, Hunskar S (2009) Cooperation between ambulance personnel and regular general practitioners. Tidsskrift for den Norske laegeforening : tidsskrift for praktisk medicin, ny raekke 129(11), 1109-1111.
| Crossref | Google Scholar |
Harrison R, Jones B, Gardner P, Lawton R (2021) Quality assessment with diverse studies (QuADS): an appraisal tool for methodological and reporting quality in systematic reviews of mixed- or multi-method studies. BMC Health Services Research 21, 144.
| Crossref | Google Scholar |
He J, Hou X-Y, Toloo S, Patrick JR, Gerald GF (2011) Demand for hospital emergency departments: a conceptual understanding. World Journal of Emergency Medicine 2, 253-261.
| Crossref | Google Scholar |
Hjortdahl M, Zakariassen E, Wisborg T (2014) The role of general practitioners in the pre hospital setting, as experienced by emergency medicine technicians: a qualitative study. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine 22, 47.
| Crossref | Google Scholar |
Ismail SA, Gibbons DC, Gnani S (2013) Reducing inappropriate accident and emergency department attendances: a systematic review of primary care service interventions. British Journal of General Practice 63, e813-e820.
| Crossref | Google Scholar |
Lazarsfeld-Jensen A, Bridges D (2014) Gaining a new respect for the other guys: scripted scenarios for inter professional education in paediatric emergencies. Australasian Journal of Paramedicine 11(2), 1-8.
| Crossref | Google Scholar |
Mahtani KR, Eaton G, Catterall M, Ridley A (2018) Setting the scene for paramedics in general practice: what can we expect? Journal of the Royal Society of Medicine 111(6), 195-198.
| Crossref | Google Scholar |
Manser T (2009) Teamwork and patient safety in dynamic domains of healthcare: a review of the literature. Acta Anaesthesiologica Scandinavica 53, 143-151.
| Crossref | Google Scholar |
Mieritz HB, Ronnow C, Jorgensen G, Mikkelsen S, Zwisler ST (2018) Communication between general practitioners and the emergency medical dispatch centre in urgent cases. Danish Medical Journal 65(1), A5435.
| Google Scholar |
Montgomery HE, Haines A, Marlow N, Pearson G, Mythen MG, Grocott MPW, Swanton C (2017) The future of UK healthcare: problems and potential solutions to a system in crisis. Annals of Oncology 28, 1751-1755.
| Crossref | Google Scholar |
Myers LA, Carlson PN, Krantz PW, Johnson HL, Will MD, Bjork TM, Dirkes M, Bowe JE, Gunderson KA, Russi CS (2020) Development and implementation of a community paramedicine program in Rural United States. Western Journal of Emergency Medicine 21(5), 1227-1233.
| Crossref | Google Scholar |
Nystøyl DS, Hunskaar S, Breidablik HJ, Østeras Ø, Zakariassen E (2018) Treatment, transport, and primary care involvement when helicopter emergency medical services are inaccessible: a retrospective study. Scandinavian Journal of Primary Health Care 36(4), 397-405.
| Crossref | Google Scholar |
Olaussen A, Semple W, Oteir A, Todd P, Williams B (2017) Paramedic literature search filters: optimised for clinicians and academics. BMC Medical Informatics and Decision Making 17, 146.
| Crossref | Google Scholar |
O’Meara P, Tourle V, Stirling C, Walker J, Pedler D (2012) Extending the paramedic role in rural Australia: a story of flexibility and innovation. Rural and Remote Health 12(2), 1978.
| Google Scholar |
O’Meara P, Stirling C, Ruest M, Martin A (2015) Community paramedicine model of care: an observational, ethnographic case study. BMC Health Services Research 16, 39.
| Crossref | Google Scholar |
Paulin J, Kurola J, Koivisto M, Iirola T (2021) EMS non-conveyance: a safe practice to decrease ED crowding or a threat to patient safety? BMC Emergency Medicine 21(1), 115.
| Crossref | Google Scholar |
Power B, Bury G (2020) A survey of general practitioner’s opinion on the proposal to introduce ‘treat and referral’ into the Irish emergency medical service. Irish Journal of Medical Science 189(4), 1457-1463.
| Crossref | Google Scholar |
Proctor A (2019) Student paramedics’ views on placements in general practice as part of a degree. Journal of Paramedic Practice 11, 519-525.
| Crossref | Google Scholar |
Reaburn G (2020) The Australasian College of Paramedic Practitioners. A specialist college for paramedics with primary healthcare skills. Australasian Journal of Paramedicine 17,.
| Crossref | Google Scholar |
Rosen MA, DiazGranados D, Dietz AS, Benishek LE, Thompson D, Pronovost PJ, Weaver SJ (2018) Teamwork in healthcare: key discoveries enabling safer, high-quality care. American Psychologist 73, 433-450.
| Crossref | Google Scholar |
Salas E, Zajac S, Marlow SL (2018) Transforming health care one team at a time: ten observations and the trail ahead. Group & Organization Management 43, 357-381.
| Crossref | Google Scholar |
Schofield B, Voss S, Proctor A, Benger J, Coates D, Kirby K, Purdy S, Booker M (2020) Exploring how paramedics are deployed in general practice and the perceived benefits and drawbacks: a mixed-methods scoping study. BJGP Open 4(2), bjgpopen20X101037.
| Crossref | Google Scholar |
Villarreal M, Leach J, Ngianga-Bakwin K, Dale J (2017) Can a partnership between general practitioners and ambulance services reduce conveyance to emergency care? Emergency Medicine Journal 34(7), 459-465.
| Crossref | Google Scholar |
Wagstaff B, Mistry V (2020) The integration of paramedics into primary care. British Journal of General Practice 70, 123.
| Crossref | Google Scholar |
Willson KA, Lim D, Toloo G-S, FitzGerald G, Kinnear FB, Morel DG (2022) Potential role of general practice in reducing emergency department demand: a qualitative study. Emergency Medicine Australasia 34, 717-724.
| Crossref | Google Scholar |
Appendix 1. Search strategy completed in Ovid Medline
| Search Line | Search | Results |
| 1 | (Ambulances or Emergency Medical Technicians or Air Ambulances or emergency medical services).sh. or paramedic*.tw. or ems.tw. or emt.tw. or prehospital.tw. or pre-hospital.tw. or first responder*.tw. or emergency medical technicians.tw. or emergency services.tw. or Ambulance*.tw. or HEMS.tw. or field triage.tw. or out-of-hospital.tw. | 106 595 |
| 2 | Allied health personnel/or emergency medical technicians/ | 17 663 |
| 3 | General practitioners/or physicians, family/or physicians, primary care/ | 30 298 |
| 4 | General Practice/or Family Practice/ | 77 248 |
| 5 | Primary Health Care/ | 87 165 |
| 6 | (primary care or primary health care).tw. | 129 764 |
| 7 | (GP* or General practitioner*).tw. | 205 874 |
| 8 | LOCUM*.tw. | 477 |
| 9 | Primary health care provider.tw. | 140 |
| 10 | 1 or 2 | 116 129 |
| 11 | 3 or 4 or 5 or 6 or 7 or 8 or 9 | 400 637 |
| 12 | 10 and 11 | 4133 |
| 13 | Cooperative behaviour/or Interpersonal Relations/ | 119 449 |
| 14 | Cooperat*.tw. | 129 698 |
| 15 | Relationship*.tw. | 1 268 945 |
| 16 | Attitude/or ‘attitude of health personnel’/or attitude*.tw. | 277 137 |
| 17 | Teamwork*.tw. | 9942 |
| 18 | Communication/ | 93 390 |
| 19 | Communicat*.tw. | 278 984 |
| 20 | Interprofessional relations/or interdisciplinary communication/ | 69 827 |
| 21 | Communication barriers/ | 7067 |
| 22 | Aware*.tw. | 219 124 |
| 23 | Rapport*.tw. | 5256 |
| 24 | Agree*.tw. | 325 908 |
| 25 | Integrat*.tw. | 488 749 |
| 26 | Collabor*.tw. | 146 021 |
| 27 | Inter-professional.tw. | 1342 |
| 28 | Perception/ | 40 977 |
| 29 | Trust/ | 11 589 |
| 30 | Network*.tw. | 447 781 |
| 31 | Compatib*.tw. | 104 932 |
| 32 | Understand*.tw. | 1 126 631 |
| 33 | Insight*.tw. | 436 339 |
| 34 | Judge*.tw. | 84 503 |
| 35 | Extended role*.tw. | 389 |
| 36 | Referral and consultations/or referral*.tw. | 159 529 |
| 37 | Scope.tw. or ‘Scope of practice’ | 64 825 |
| 38 | Link*.tw. | 948 627 |
| 39 | Interrelate*.tw. | 42 046 |
| 40 | Associat*.tw. | 4 421 971 |
| 41 | Correspond*.tw. | 599 852 |
| 42 | Connect*.tw. | 372 365 |
| 43 | Liais*.tw. | 8180 |
| 44 | 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 | 9 010 404 |
| 45 | 12 and 44 | 2346 |
*, truncation symbol when used in OVID MEDLINE.