Student-led pop-up health check clinics: innovative health prevention strategy for a low socioeconomic community
Nicole M. Coombs A B * , Lauren Sewell C , Megan R. Jackson B , Kaye Borgelt C , Jessica Lee A and Joanne E. Porter
A B * , Lauren Sewell C , Megan R. Jackson B , Kaye Borgelt C , Jessica Lee A and Joanne E. Porter  B
B
A Federation University Australia, Institute of Health and Wellbeing-Nursing, Gippsland Campus, PO Box 3191, Gippsland Mail Centre, Churchill, Vic. 3841, Australia.
B Collaborative Evaluation & Research Group (CERG) Federation University Australia, Gippsland Campus, PO Box 3191, Gippsland Mail Centre, Churchill, Vic. 3841, Australia.
C Gippsland Primary Health Network, 11 Seymour Street, Traralgon, Vic. 3844, Australia.
Australian Journal of Primary Health - https://doi.org/10.1071/PY23034
Submitted: 28 February 2023 Accepted: 13 July 2023 Published online: 4 August 2023
© 2023 The Author(s) (or their employer(s)). Published by CSIRO Publishing on behalf of La Trobe University. This is an open access article distributed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND)
Abstract
Background: To improve preventative health screening in regional Victoria, Australia, a collaborative student-led health prevention strategy was initiated. The aim of this study is to evaluate the impact of four health check clinics using a free ‘pop-up’ format within community settings.
Methods: A mixed methods, explanatory sequential design was used to explore community health data and participant experiences in utilising the free health check clinics. The clinics were delivered over 6 months and located in three different communities within the regional government area. Descriptive statistics were used to analyse participant health data and a thematic analysis was utilised to determine themes from participant feedback and health outcomes.
Results: The clinics were attended by 188 community members, largely impacted by government lockdowns during the coronavirus disease 2019 (COVID-19) pandemic. Health check results indicate the population is overweight and at high risk of diabetes. Participants enjoyed the free and convenient nature of the health check program and the location of the venues. Feedback from participants indicate the health education provided was useful and advocated for changes in current behaviours. Many embraced the new information and community connections and made changes to improve their future health. Others claimed to enjoy the clinic experience but reported no action from the recommendations.
Conclusions: Evaluation of the health check clinics indicate they had a minor, yet positive impact on the local community in increasing engagement with preventative screening strategies. COVID-19 restrictions impacted participant numbers and thus more research is needed in a time where community movement is not limited.
Keywords: community clinic, evaluation, health checks, healthcare access, pop-up, prevention screening, primary health, student-led.
Introduction
Opportunistic health screening has traditionally been utilised during patient consultations and in health promotion or primary care programs for early detection of disease, health education and risk reduction (Gippsland Primary Health Network 2023). However, in the absence of symptoms, preventative health check services are often underutilised by the public (Brunner-Ziegler et al. 2013). Preventative primary care interventions reportedly contribute to reducing mortality and increasing independence (Birtwhistle et al. 2017), yet research suggests that populations of low education and socioeconomic status are less likely to use preventative services or ‘check in’ with their health (Dryden et al. 2012; Broholm-Jørgensen et al. 2019).
Similarly, in Gippsland, Victoria, Australia, unpublished results from a local community survey (Larter Consulting and Gippsland Primary Health Network 2021) provided a snapshot of the community’s healthcare practices, indicating low community engagement with general practice for opportunistic risk screening. A review of the literature conducted as a part of the Latrobe Health Innovation Zone: Early Detection and Screening including Tobacco Project (Gippsland Primary Health Network 2021a), also explored the provision of opportunistic risk screening in community settings, and found that screening conducted in ‘everyday settings’, can influence a participants’ care-seeking behaviours and reach those who are less connected to the healthcare system (Larter Consulting and Gippsland Primary Health Network 2021). The report highlighted an outreach approach for opportunistic screening had been demonstrated to have a high impact among specific targeted populations, with a ‘drop-in’ style of service being effective among low socioeconomic communities, as opposed to scheduled or structured strategies (Roberts and de Souza 2016; Trivedy et al. 2017). A pilot project implementing a HealthCheck tool (Reed 2018), showed one limitation in delivering risk assessment screening in this Gippsland community was the lack of connection to primary care services. As such, it was determined that familiar settings such as workplaces or community venues may proffer more opportunistic preventative connection with the local population.
In response to these findings, a collaboration between Gippsland Primary Health Network (Gippsland PHN), the Collaborative Evaluation and Research Group (CER) and School of Nursing from the local university was established, to plan and deliver a free, pop-up health check service within the local government area of Latrobe, Gippsland. Undergraduate nursing students were included in the program delivery team, as the benefits of the service learning model are well recognised in supporting a pressured health system and complimenting limited clinical placement hours during their learning journey (Stuhlmiller and Tolchard 2018; Coombs et al. 2021). The pop-up health check clinics hoped to increase access to preventative screening and health education, for a population known to have poor healthcare connections. The aim of this study was to evaluate the effectiveness of utilising pop-up style services in this area and determine their impact on the population’s health behaviours.
Methods
A mixed methods approach was utilised in this study, with an explanatory sequential design. Mixed methods was most appropriate for this study due to the objective nature of the health check data, and the subjective interpretation and experiences of participants. It was important to explore follow-up behaviours after participants received any health education (dependent on health check results) and whether the clinics influenced preventative behaviour changes. Therefore, evaluating the effectiveness of the clinic would require both quantitative and qualitative data, which were collected via the use of paper-based clinical records and telephone interviews.
Participants and recruitment
Participants in this study were adults aged >18 years, living in Latrobe. Four clinics were conducted in three different Latrobe communities and operated between August and November 2021. Advertising of the clinics was conducted via local newspapers and radio, as well as displaying brightly coloured flags and banners outside each venue during operating hours. Participation was voluntary, where people could walk in without appointment, receive explanation of the study purpose, and receive plain language information and sign consent. Jargon-free verbal explanations were provided, and participants could partake in all or any of the health checks offered. Further consent and contact details were collected from those wishing to participate in follow-up calls to discuss outcomes and follow-up behaviours. All participants were advised data would be reported as aggregated research findings only.
Setting
Located approximately 150 km from Melbourne, with a population of 77 318 people (Australian Bureau of Statistics (Victoria) 2021), Latrobe is considered relatively disadvantaged. The Social Economic Indexes for Areas (SEIFA) index indicate that many households have a low income, many people have no qualifications, or are employed in low skill occupations (Remplan 2022). People living in this community also have high rates of chronic disease. Australian Institute of Health and Welfare (Australian Institute of Health and Wellbeing (Australian Government) 2021) data show the incidence of heart, stroke and vascular disease for persons aged ≥18 years in Latrobe is 7.5% compared to 6.2% across Australia, and up to 8.2% within certain postcodes in the area. Avoidable deaths resulting from heart disease per 100 000 people in Latrobe is 65.5, compared to a 40.3 average for Gippsland and 32.4 in Victoria (Gippsland Primary Health Network 2022).
Therefore, four temporary pop-up health clinics were created in vacant retail venues within the Latrobe communities of Churchill, Morwell, and Traralgon, using two different shopping centres and one roadside retail strip. The clinic operating hours were Tuesday–Friday from 11 am to 5 pm and Saturday 9.30 am to 1.30 pm, for 3 weeks at each venue. The clinics were equipped with clinical working spaces for the nursing students, academics, and research team, along with providing tables, couches, and chairs for participants. The spaces aimed to provide a comforting atmosphere, with a refreshments station for participants alongside self-select pamphlet information regarding local health promotion initiatives and healthcare services. As the clinics were operating during the coronavirus disease 2019 (COVID-19) pandemic, venues were designed to comply with government restrictions, with QR code check-in requirements, density limit allocations, hand sanitiser and mask-wearing requirements. The initial clinic site was closed after the first week, as the community was subject to a compulsory lockdown by the Victorian government due to rising COVID-19 infection rates. This site was used again later to ensure members of this community were given equal opportunity to access the free health check service.
Data collection and analysis
Data were collected from participants attending all three clinic locations. All clinical health data were collected by the nursing students or supervising academics working in the clinics. A research assistant conducted offsite telephone interviews with consenting participants from all four clinics.
Quantitative data were collected via a paper-based, duplicate document, capturing all the health check results and demographic data for each participant. One copy was kept by the research team, and one copy given to participants for their own records, or to take to their healthcare provider if required. The documentation contained data such as height, weight, body mass index (BMI), blood pressure reading, pulse, respiratory rate, cholesterol level, blood sugar level and a diabetes risk score. All data recorded at the clinic were obtained through conducting the relevant assessment or measure (i.e. weight taken from participant standing on scales at the site). Participants were provided health education from nursing students and academic supervisors on interpretation of the health data findings, with appropriate escalation of care undertaken when necessary. The health check duration was approximately 15–20 min, with additional time allocated based on participant care or education needs.
Data were then analysed using SPSS Statistics for Windows Ver. 26 (IBM Corp 2019.Armonk, NY: IMB Corp), with descriptive statistics used to measure frequencies and relationships between variables. An enumerative content analysis was also utilised for the various recommendations made by nursing staff to identify the most common education being provided. Recommendations were recorded on the health check document, with these data were then tabulated, coded and had frequencies counted.
Qualitative data were collected via semi-structured telephone interviews with consenting participants, 4 weeks post attending the clinic. The interviews were 5–12 min in duration and provided opportunity for participant feedback and to ascertain whether participants engaged in further health promotion activities or sought further medical advice based on their health data findings, and whether they found the information provided in the clinic useful. Notes were taken during each call and important comments documented for analysis. A thematic analysis of the participant feedback was then conducted using six steps recommended by Braun and Clarke (2022). This approach involved familiarisation with the interview data; initial codes being generated; development of themes; refining and reviewing the themes and providing appropriate names; then reporting the themes in a final report of the outcomes. The thematic analysis process was undertaken by four members of the research team to reduce the potential for bias. Any discrepancies were resolved by group discussion until consensus was obtained.
Ethics approval
Ethics approval was granted by the Federation University Human Research Ethics Committee (approval number A21-087), based on the Australian Research Council (2018) National Statement on Ethical Conduct in Human Research. The research was undertaken with appropriate informed consent of participants or guardians.
Results
Quantitative data
A total of 188 participants utilised the pop-up health check clinics in their communities. Of these participants, 58% (n = 108) identified as female and the average age of participants was between 50 and 70 years (60%, n = 109). Health check data indicated the population had blood pressure readings within the normal range, with the average reading of 130/80 mmHg. The average pulse was 82 beats per minute and respiratory rates were also normal, averaging 17 breaths per minute. The average height was 168.4 cm and average weight, 86.6 kg. However, breaking down weight by gender, 68% (n = 50) of men weighed >80 kgs and 69% (n = 75) of women weighed >70 kgs
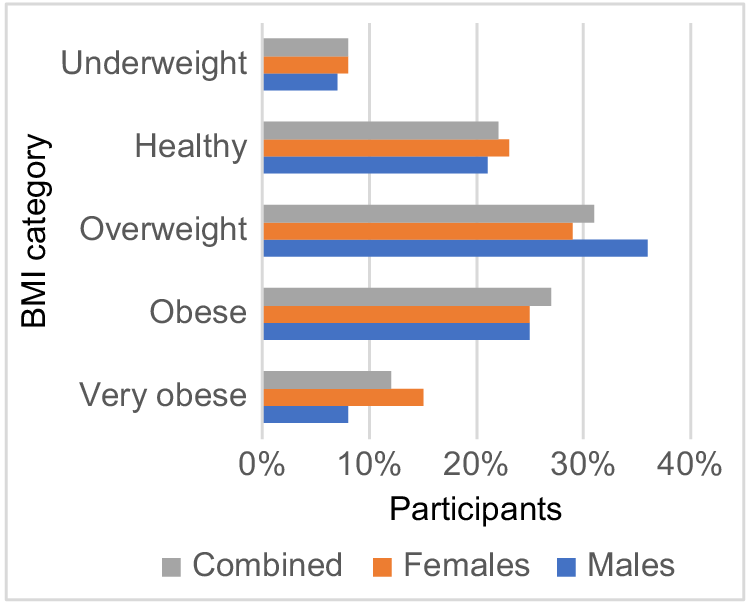
BMI measures (weight (kg) × height (cm)) resulted in 70% (n = 130) of participants falling outside the healthy range (see Fig. 1). Average waist measurement for males was 106.5 cm, and 100.25 cm the average for females. Sixty-four percent of males fell outside the recommended measures, with those having waist measurements >111 cm represented by 38% (n = 28) of the full male sample. Twenty-seven percent (n = 29) of females had waist measurements within the recommended healthy range, and 26% (n = 28) had measurements >110 cm.
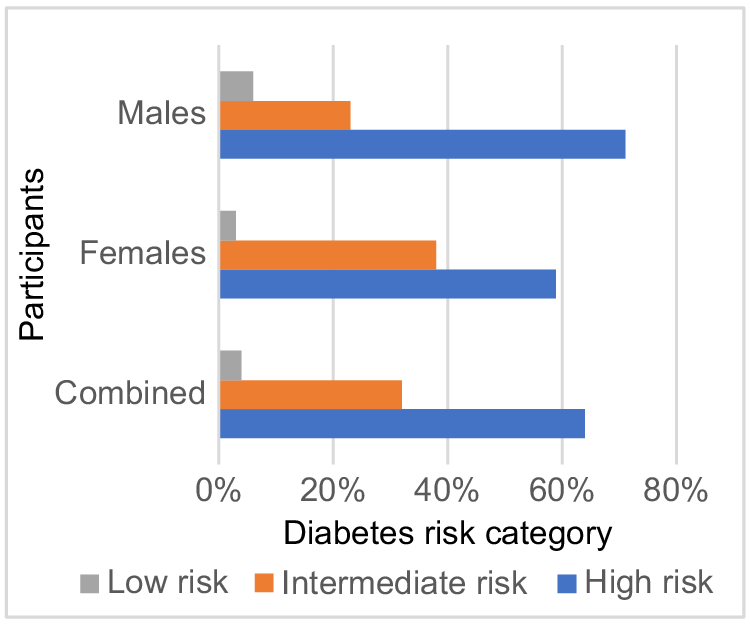
These waist measurements also contributed to diabetes risk scores. Four percent (n = 3) produced low risk scores, with 64% (n = 46) having high risk scores (see Fig. 2). Any discrepancy seen in the numbers was due to some participants already having diabetes or not wishing to partake in this assessment.
With the pop-up clinics promoting the importance of regular health checks, findings such as these initiated health discussions between the nursing staff and the participants, with recommendations made regarding healthy behaviour changes. The most common discussion was regarding confirmation or reassurance about good health practices (see Table 1). This was followed by diet and exercise recommendations and encouragement to see a local doctor regarding an abnormal health check result or medication queries.
| Recommendation topic | Number of discussions (n) |
|---|---|
| Continue good work/confirmation/reassurance | 77 |
| Diet and exercise advice | 69 |
| General Practitioner- abnormal result/medication review | 37 |
| General Practitioner- generic | 31 |
| Reduce smoking | 14 |
| Specific condition information - monitoring/medications (BGL, BP advice) | 13 |
| Alcohol advice | 13 |
| Stress/sleep issues | 6 |
BGL, blood glucose level; BP, blood pressure.
Qualitative data
In total, 109 participants consented to follow-up phone calls. Of the 109 participants, 74 participants were contactable and willing to be interviewed. Of these, 61% were female, 35% male and 4% identifyed as non-binary or transgender. Ages ranged from 15 to 80+ years, with a median range of 56–60 years. Of those who provided feedback, 37% had made changes to their current behaviours or sought medical intervention from the advice given in the clinics, whereas 17% were thinking about making changes. The remaining participants had not acted on the recommendations or had been reassured that their current behaviours were keeping them healthy. Thematic analysis identified two themes; (1) With knowledge comes power; and (2) It’s all in the delivery. Each theme also contained their own subthemes.
Most participants stated the clinic was valuable or useful. Several participants stated the information from the clinic had empowered them to take charge of their health or had motivated them to want to make changes to prevent poor health in the future. One participant claimed the information had ‘changed his life’. Participants used words such as ‘surprising, reassuring and motivating’, with half stating the information provided in the clinics was helpful. Some mentioned a change to exercise, either going to the gym, walking or even working more in the garden. One participant stated, ‘I have started swimming and I feel lighter and more energetic’. Others had made dietary changes such as reducing dairy or red meat, with another explaining they ‘cut out all take-away food…used to be 4–5 times a week’ and enjoyed the added benefit of saving money. Other participants stated they had consulted with their GP after attending the health clinic. Notably, one participant who identified as having high blood pressure in the pop-up clinic consulted their GP and had their medication reviewed with good effect. Another had purchased a blood pressure machine for home to continue monitoring. Of the participants who disclosed their smoking status, some participants requested resources for smoking cessation.
Some participants stated they had not made any changes following the health check. Of these, most stated the information had been useful or reassuring, ‘this is probably more suited to older people, but I’m glad I could get my blood sugar checked’. Some expressed positive feedback such as ‘very happy with the program’ and ‘Keep up the good work’, but their pop-up clinic experience had not prompted any action or changes in behaviour. Some had told their family about the clinics but had not implemented any actions themselves. Comments such as ‘made me have a good look at myself’ and ‘was motivated for 10 s’ were made, but with no declared outcomes. Of the rare few participants who did not find the clinic useful, their comments related to lack of confidence in the student nurses and dissatisfaction with mistakes made when having their blood glucose levels checked, causing them to feel pain by having their finger pricked more than once.
The quality of delivery was mentioned by more than half of the participants, using words such as ‘knowledgeable, kind, professional, well organised, good initiative, fantastic, beneficial, great service, and high standard’ to describe the clinic experience. They expressed a desire for the service to continue and their appreciation of the students having the opportunity to learn, as well as helping the community. Another participant stated they were ‘nervous when I entered, but the students and staff comforted me and settled me down’. Participants enjoyed meeting local nursing students and staff and thought them ‘supportive, polite and good communicators’.
Several participants expressed positive opinions about the location and accessibility of the clinic. The free service was valued, as was the ‘quick and easy’ walk-in service. Participants appreciated the convenience of providing the service in shopping centres, with many commenting on difficulty accessing a GP in the area. One participant stated they ‘loved it...would like to see more of this…excellent location’, commending the organisers for the initiative. The access to additional resources and other local service connections was also valued by participants, making connections with smoking cessation programs, dietary advisors, diabetes supports and cancer screening strategies in the area. Those with co-morbidities stated they felt reassured by having easy access to blood pressure, cholesterol, or blood sugar checks; one claiming ‘I want to monitor my blood pressure regularly, but it’s hard to get in to see my doctor’. Constructive comments were also provided, ‘could have been advertised better, I had difficulty finding the clinic’, or concerns about the space within the clinic regarding social distancing or privacy issues. Overall, an overwhelmingly positive response was seen from the participants, who shared their experiences, made suggestions, and expressed appreciation for the benefits the clinic had on them and their community.
Discussion
Previous student-led healthcare services have not always evaluated the impact of programs from the perspective of the recipients of care (Simmons et al. 2022). However, in this study, those that attended the free pop-up health clinics were generally very positive about the clinic experience, with participants stating that information they had received in the health check had empowered them to take charge of their health or motivated them to want to make positive changes. Comparable with other Australian student-led clinic studies, participants in this study also felt confident in the knowledge and skills of the nursing students conducting the checks and were satisfied with the service provided (Beckman et al. 2022). Participants also indicated they had increased engagement with the primary health system and consulted with their GP because they had attended the pop-up health clinic.
However, due to the relatively small sample size in comparison to the overall population of the community in focus, generalisation of the results is cautioned. Although early detection of chronic disease was identified in many participants, the pop-up clinic concept was still limited in both reach and community impact. This is contrary to previous suggestions that health screenings conducted in ‘everyday settings’ such as shopping centres may influence a participants’ care-seeking behaviour and reach vulnerable groups who are less connected to the healthcare system (Roberts and de Souza 2016; Larter Consulting and Gippsland Primary Health Network 2021). As a trial intervention, there was no predicted participation number, and although the clinics were fitted out with branded banners and posters inviting participants to have a free health check and local media advertising was conducted, further research is required to determine the impact of the publicity strategy on public engagement with the program, or whether engagement was coincidental given the clinic location decisions.
The timing of the clinic delivery was also a consideration during the evaluation. Victoria was impacted substantially during the COVID-19 pandemic and spent long periods with stringent restrictions, which severely curtailed community movement, constituting what was at the time, one of the world’s longest and strictest lockdowns (Trauer et al. 2021). Lockdowns seriously impacted operation of the pop-up clinics, with some clinics postponed at short notice and decreased foot traffic impacting participant numbers as the community chose to limit unnecessary visits to potentially high-risk areas such as shopping centres. The location of each clinic was also determined according to availability of empty shopfronts during the designated period, with a preference for locations with higher foot traffic such as shopping plazas. Further research is needed to replicate this research in a time not impacted by community lockdowns to ascertain if this would result in greater community participation.
The effectiveness of a screening program also needs to consider the potential and readiness for behaviour change in relation to the intended audience. Older populations are less likely to see the benefits of positive behaviour changes to improve future health outcomes, as they are more likely to already be living with the health consequences of earlier lifestyle choices (McPhee et al. 2016). With 60% of our clinic participants within the age bracket of 50–70 years, although positive changes are still recommended to reduce chronic illness, some already report having diabetes or other existing cardiac or respiratory ailments, whereas promoting healthier behaviours to a younger population in this setting offers capacity building among those who can modify their lifestyle to include healthy behaviours and thus reduce the risk of developing chronic illness in future years.
In common with many other regional areas in Australia, access to GPs has been identified as a barrier in the Gippsland region. Gippsland PHN reports an average of 107 medical practitioners per 100 000 people (Gippsland Primary Health Network 2022), compared with the average across Victoria of 120 per 100 000 people (Australian Government Department of Health 2022), with affordable and timely access to GPs identified as a top health issue in the area (Gippsland Primary Health Network 2021b). Student-led healthcare programs offer a sustainable and collaborative alternative health service that can help support underserved populations (March et al. 2023), and this study demonstrates the community appreciation of having improved, opportunistic access to simple checks for blood pressure and blood sugar levels, when other services are unavailable.
As such, a more focused evaluation could be suggested for future delivery, with the aim to identify other potential causes of healthcare disconnect within this community. Although the mixed method approach used in this study provided insight into participant satisfaction and current health status, perhaps deeper understanding of social determinants could be ascertained through more targeted follow-up interviews. This study also predominantly focuses on access to GP healthcare services. Further exploration is needed to understand this community’s association with other social and allied health services available.
Despite the impact of the COVID-19 pandemic, the outcomes of the four pop-up clinics were predominantly positive. The clinics identified health areas of concern within the community, with the sampled population being largely overweight and having high risk of diabetes. Although participant numbers were not high in relation to the whole population, those who did attend any of the clinics appreciated the ease of access and free service, taking advantage to ‘check in’ with their current health status at their own convenience. Community members appreciated the learning opportunities the clinics provided for future nurses and supported the connections made with their communities. The impact of COVID-19 lockdown restrictions on the community at the time of pop-up clinic delivery limits conclusions about the design of the model and success in preventative health screening engagement. Further research in this area is recommended, particularly with a focus on engaging with younger populations in workplace and/or education settings, collecting smoking data and measuring readiness for change.
Acknowledgements
The researchers would like to acknowledge Gippsland Primary Health Network and Collaborative Evaluation & Research Group (CERG) Federation University, for the opportunity to create this community health initiative. We also commend all nursing students who have continued to be resilient and embrace any learning opportunities despite the many COVID-19 pandemic disruptions.
References
Australian Bureau of Statistics (Victoria) (2021) Census QuickStats. (Australian Bureau of Statistics [Latrobe]) Available at https://www.abs.gov.au/census/find-census-data/quickstats/2021/LGA23810 [Accessed December 2022]
Australian Government Department of Health (2022) Primary care GP statistics in Victoria. Available at https://hwd.health.gov.au/resources/data/gp-primarycare.html
Australian Institute of Health and Wellbeing (Australian Government) (2021) Geographical variation in disease: diabetes, cardiovascular and chronic kidney disease. Available at https://www.aihw.gov.au/reports/chronic-disease/geographical-variation-in-disease/data [Accessed December 2022]
Beckman EM, Mandrusiak A, Forbes R, Mitchell L, Tower M, Cunningham B, Lewis P (2022) A student-led, interprofessional care, community-based healthcare service: student, clinical educator and client perceptions of interprofessional care and education. Focus on Health Professional Education: A Multi-Professional Journal 23, 90-108.
| Crossref | Google Scholar |
Birtwhistle R, Bell NR, Thombs BD, Grad R, Dickinson JA (2017) Periodic preventive health visits: a more appropriate approach to delivering preventive services: from the Canadian task force on preventive health care. Canadian Family Physician 63, 824-826.
| Google Scholar |
Broholm-Jørgensen M, Kamstrup-Larsen N, Guassora AD, Reventlow S, Dalton SO, Tjørnhøj-Thomsen T (2019) ‘It can’t do any harm’: a qualitative exploration of accounts of participation in preventive health checks. Health, Risk & Society 21, 57-73.
| Crossref | Google Scholar |
Brunner-Ziegler S, Rieder A, Stein KV, Koppensteiner R, Hoffmann K, Dorner TE (2013) Predictors of participation in preventive health examinations in Austria. BMC Public Health 13, 1138.
| Crossref | Google Scholar |
Coombs NM, Missen K, Allen L (2021) Beyond simulation – extracurricular volunteering in nursing education: a focus group. Nurse Education Today 96, 104603.
| Crossref | Google Scholar |
Dryden R, Williams B, Mccowan C, Themessl-Huber M (2012) What do we know about who does and does not attend general health checks? Findings from a narrative scoping review. BMC Public Health 12, 723.
| Crossref | Google Scholar |
Gippsland Primary Health Network (2021a) Latrobe health innovation zone: what do we do. (Gippsland Primary Health Network). Available at https://gphn.org.au/what-we-do/programs/latrobe-health-innovation-zone/ [Accessed December 2022]
Gippsland Primary Health Network (2021b) Resources: priority issue papers. Available at https://gphn.org.au/resources
Gippsland Primary Health Network (2022) Gippsland PHN Health needs: Latrobe City snapshot. Available at https://gphn.org.au/wp-content/uploads/files/pdf/Latrobe-Snapshot-V7.pdf
Gippsland Primary Health Network (2023) Risk assessment and opportunistic screening. Available at https://gphn.org.au/what-we-do/programs/latrobe-health-innovation-zone/risk-assessment-and-opportunistic-screening/ [Accessed May 2023]
March S, Mangoyana C, Oakley P, Lalloo R, Walsh LJ (2023) Positive impacts of oral health services provision by a student-led primary care clinic to an Australian rural indigenous community. Australian Dental Journal 0, 1-9.
| Crossref | Google Scholar |
McPhee JS, French DP, Jackson D, Nazroo J, Pendleton N, Degens H (2016) Physical activity in older age: perspectives for healthy ageing and frailty. Biogerontology 17, 567-580.
| Crossref | Google Scholar |
Remplan (2022) Our Place – Our Community. (Remplan [Latrobe City]) Available at https://app.remplan.com.au/latrobe/community/wellbeing/seifa-relative-disadvantage?state=7YrohY!LwlkSXxq6s3DbnACGw92puwTKFJket2FmFrFZFAN1 [Accessed December 2022]
Roberts DJ, de Souza VC (2016) A venue-based analysis of the reach of a targeted outreach service to deliver opportunistic community NHS health checks to ‘hard-to-reach’ groups. Public Health 137, 176-181.
| Crossref | Google Scholar |
Simmons LM, Emily C, Barker R, Barnett F (2022) Measuring health outcomes, experience of care and cost of healthcare in student-led healthcare services: a literature review. Focus on Health Professional Education: A Multi-Professional Journal 23, 37-64.
| Crossref | Google Scholar |
Stuhlmiller CM, Tolchard B (2018) Population health outcomes of a student-led free health clinic for an underserved population: a naturalistic study. Journal of Community Health 43, 193-200.
| Crossref | Google Scholar |
Trauer JM, Lydeamore MJ, Dalton GW, Pilcher D, Meehan MT, Mcbryde ES, Cheng AC, Sutton B, Ragonnet R (2021) Understanding how Victoria, Australia gained control of its second COVID-19 wave. Nature Communications 12, 6266.
| Crossref | Google Scholar |
Trivedy C, Vlaev I, Seymour R, Philpott M (2017) An evaluation of opportunistic health checks at cricket matches: the boundaries for life initiative. Sport in Society 20, 226-234.
| Crossref | Google Scholar |