Patient initiated radiology requests: proof of wellness through images
Lizzie De Silva A * , Melissa Baysari
A * , Melissa Baysari  B , Melanie Keep
B , Melanie Keep  C , Peter Kench
C , Peter Kench  A and Jillian Clarke
A and Jillian Clarke  A
A
A Discipline of Medical Imaging Science, Sydney School of Health Sciences, Faculty of Medicine and Health, The University of Sydney, Susan Wakil Health Building, Camperdown Campus, Western Avenue, Camperdown, NSW 2006, Australia.
B Biomedical Informatics and Digital Health, Faculty of Medicine and Health, Charles Perkins Centre D17, The University of Sydney, Sydney, NSW 2006, Australia.
C Sydney School of Health Sciences, Faculty of Medicine and Health, The University of Sydney, Susan Wakil Health Building D18, Camperdown, NSW 2006, Australia.
Australian Journal of Primary Health - https://doi.org/10.1071/PY22247
Submitted: 24 November 2022 Accepted: 24 July 2023 Published online: 24 August 2023
© 2023 The Author(s) (or their employer(s)). Published by CSIRO Publishing on behalf of La Trobe University. This is an open access article distributed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND)
Abstract
Background: Traditionally, general practitioners (GPs) have initiated the need for, and ordered, radiological tests. With the emergence of consumer-centred care, patients have started to request scans from doctors on their own initiative. Consumeristic health care has shifted the patient–doctor dyadic relationship, with GPs trending towards accommodating patients’ requests.
Methods: A mixed method analysis was conducted using a survey instrument with open ended questions and concurrent interviews to explore participants’ responses from their requests for radiological studies from GPs. Themes emerging from both qualitative and quantitative methodologies were mapped onto the Andersen Newman Model (ANM).
Results: Data were analysed for ‘predisposing,’ ‘need’ and ‘enabling’ elements of the ANM model and were correspondingly mapped to patient’s requests for radiological referrals according to the elements of the ANM. Participants expressed anxiety about their health, were confident in the types of radiological scans they desired and typically indicated the need for evidence of good health. Their desire for such requested scans was often enabled through prior exposure to health information and the experience of specific symptoms. Requests came with the expectation of validation, and if these requests were denied, participants indicated that they would seek another doctor who would oblige.
Conclusions: In our modest study of Australian patients, participants were well informed about their health. Exposure to information seems to create a sense of anxiousness prior to visiting the doctor. Individuals sought visual proof of wellness through imaging, and doctors in return often accommodated patient requests for radiological studies to appease patients’ needs and to maintain workflow.
Keywords: diagnostic imaging, empowerment, health consumer, health outcome, internet, mixed methods, patient-doctor communication, patient preference, patient request, radiological requests.
Introduction
Traditionally, GPs have been central in patient care (Palanica et al. 2019), acting as the ‘gatekeepers’ to medical interventions by, for example, directing medical services, prescribing medications and facilitating decision-making (Palanica et al. 2019). However, with increased availability of online health information, patients are more informed and active in their health, particularly with some patients having a sense of consumeristic entitlement (Lee et al. 2014). This is not a new phenomenon, as patients are seen as developing their intellectual curiosity and ‘getting what they want’ (Lee et al. 2015). One element of consumer-driven care is seen in patients requesting a referral for a radiological study from their GPs. It is thought that some of these requests are fuelled by the availability of online health information, where individuals are more aware of their health needs and goals (Lee et al. 2015; Hodyl et al. 2020). Platforms, such as social media (Esen et al. 2019), mobile applications (Groß and Schmidt 2018) and community led online groups (Fiksdal et al. 2014), are encouraging individuals to become proactive during patient–doctor consultations. As such, doctors’ gatekeeping roles are diminishing as consumer driven needs increase (Lee et al. 2015).
In Australia, only qualified health practitioners, such as GPs, can write a referral letter for radiological services, including imaging and image guided procedures in computer tomography (CT), magnetic resonance imaging (MRI), X-rays and ultrasounds. Thus, patients who want to have a radiology test performed need to approach their GP for the referral. Moreover, with Medicare subsidised services, most of these requests for studies come at little to no cost to patients. To explore factors contributing to patients’ requests for radiological imaging, we used the Andersen Newman Model (ANM) for healthcare utilisation (Andersen and Newman 1973). This model provides a framework with which to discover aspects that facilitate or impede the use of healthcare resources. Past studies using the model have addressed the phenomenon of doctors fulfilling requests for patient satisfaction (Jerant et al. 2018), explored patients’ spoken and unspoken expectations during a clinical consultation (Fenton et al. 2015) and further explored patients’ perceived needs during clinical visits (Benetoli et al. 2018). Most of these studies have been situated within a general practice context with requests for prescribed medications (Kravitz et al. 2003; Paterniti et al. 2010; Hogue et al. 2012; Fenton et al. 2015), while limited work has focused on patient perceived needs for radiological tests and their experiences around these requests (Alamri et al. 2014; Walderhaug et al. 2022).
The ANM (Andersen and Newman 1973) provides a conceptual framework in recognising antecedents for healthcare use through understanding human behaviour, specifically within the patient–doctor relationship (Andersen 1995; Bradley et al. 2002; Petrovic and Blank 2015). A study by Strain (1990) on GP home visits to the elderly, suggested the need to include psycho-social and socio-cultural elements to ANM (Strain 1990). Petrovic and Blank (2015) described adherence to prescribed medication among the elderly with chronic illnesses using ANM, recognising how the model lends itself to examining elements of trust between patients and doctor. Thus, the original model (Andersen and Newman 1973), the purpose of which was to discover conditions that facilitate or impede the use of health care, has evolved throughout the years, originally focusing on the family, but now applicable to individual patients (Andersen 1995; Bradley et al. 2002; Andersen and Newman 2005). Kravitz et al. (2003) used a modified version of ANM on patients requesting services within a general practice. Their study demonstrated the socio-cultural characteristics or ‘predispositions’ that exist prior to illness, and extended this to include the logistics or ‘enabling’ factors of accessing care, and described the ‘need’ for seeking such care. Using this modified framework by Kravitz et al. (2003), we describe ‘predisposition’, ‘enabling’ and ‘need’ factors that initiate patients’ requests for radiological studies. We hope, by using a two-phase explanatory design, to address the gap in understanding such patient-initiated radiological requests, particularly with consideration of patient–doctor interactions.
Thus, ANM is an appropriate model to examine in our study, as the individual unit of analysis is the patient requesting a radiological service, but it also lends itself to the expansion of the patient–doctor dyad in which its application occurs during clinical negotiations, such as the doctor acquiescing to a patient’s specific request. In this study, we included the survey instrument, the open-ended questions and concurrent interviews to further identify unique views and experiences.
Aim and objectives
The overarching aim of this study was to explore predisposing, need and enabling elements of patients requesting radiological referrals, and their self-reported experiences and outcomes from such requests.
Objective 1: What themes emerge as patients’ predisposing, need and enabling factors specific to requesting radiological referrals?
Objective 2: What are the main drivers for requesting radiological studies?
Objective 3: What is the patient reported outcomes from such requests?
Methods
This mixed method study was approved by the University of Sydney Ethics Review Board. The data was collected from January 2022 to February 2022, starting with a survey that aimed to understand participants’ experiences as a patient requesting a radiological referral from a doctor when attending a primary care facility. The questionnaire provided volunteers with the option of a follow-up interview, to further explore their responses. Sixty participants who had requested a radiological referral from their doctor within the last 5 years responded to the survey, and eight participants were interviewed.
Participants
Participants were recruited using the online market research platform Qualtrics (https://www.qualtrics.com/au), and were eligible to complete the survey if they were over the age of 18 years and had requested radiological studies in the past 5 years from GPs working in primary healthcare facilities within Australia. Qualtrics members were sent an invitation via email or by in-app and SMS notification asking if they would be interested in participating in a 20 min anonymous survey offering a small reward upon completion. Consent was implied when participants submitted the completed questionnaire. The participants were also asked at the end of the survey if they would be interested in being interviewed to further explore their responses. If they answered yes, they were able to submit their contact details. They were required to read a participant information statement. Individuals were advised their participation was voluntary and verbal consent given at the start of the interview.
Study design
The survey and interview questions were piloted with Qualtrics’ first six respondents, and minor alterations made. The survey consisted of 30 questions to capture patients’ demographics such as gender, age, educational attainment and employment status. The survey asked about participants’ frequency of internet use, if they had a chronic health condition, their self-reported ratings of health and lifestyle, who they first turn to for health information, their experiences interacting with doctors in requesting referrals and the doctors’ response to their requests. The final component asked about the outcome from their request. The questionnaire also included open-ended sections for participants to provide in-depth answers. Overall, the survey took approximately 30 min to complete.
The interview was semi-structured to facilitate an in-depth discussion of the topics. Participants were given an opportunity to speak freely about their experiences in requesting radiological referrals. They were invited to describe their experiences in making a request, including their thoughts around their clinical encounter, the doctor’s responses, the types of websites they visited, their overall views on health and lifestyle and their satisfaction with the outcome of their radiological requests. Interviews typically lasted from 20 to 30 min (average = 22.75 min, s.d. 6.88).
Data collection
Both data sets were collected with the intention of using a convergent parallel mixed methods approach for data analysis (Creswell 2008) and to integrate findings. Interviews were conducted by the first author, using the recording app on their iPhone. Interview data was transcribed, anonymised, transferred to secure storage and permanently deleted from the iPhone.
Data analysis
Using IBM SPSS software (ver. 28), the quantitative survey data were analysed using descriptive statistics resulting in frequency tables and cross tabulations.
NVivo (release 1.6.1) was used for data analysis of the open-ended questions and the interview data. After recording the interviews, the data were transcribed by the first author into a word document and then imported into NVivo. A two-step approach was used for coding. A conventional thematic analysis (Hsieh and Shannon 2005) allowed codes to flow freely from the data and, using a directed analysis approach (Hsieh and Shannon 2005), were then mapped to the dimensions of the ANM: ‘predisposing’, ‘enabling’ and ‘needs’. The coded data and the themes were reviewed by the research team with discrepancies resolved through discussion.
Abbreviations used to describe interview and survey participants are as follows: gender (M/F); age (years); level of education high school (HS), university (U), postgraduate (PG), and diploma (D); and employment status employed (E), unemployed (UE) and retired (R).
Results
There were 60 respondents who completed the survey of whom 10 agreed to be interviewed, however, thematic saturation was achieved after eight and further interviews were ceased. A true survey response rate was unable to be determined using the external market research panels, as some panel members may have overlooked the invitation, or declined participation based on the incentives offered. Most of the requests were for X-rays and ultrasounds, as indicated in Table 1.
| Imaging modality (n = 60) | n (%) |
|---|---|
| X-Ray | 26 (43) |
| Ultrasound | 18 (30) |
| Magnetic resonance imaging | 8 (10) |
| CT (computerised tomography) | 4 (7) |
| Total | 54 (90) |
| Missing | 6 (10) |
Response options are not mutually exclusive as respondents could choose more than one answer.
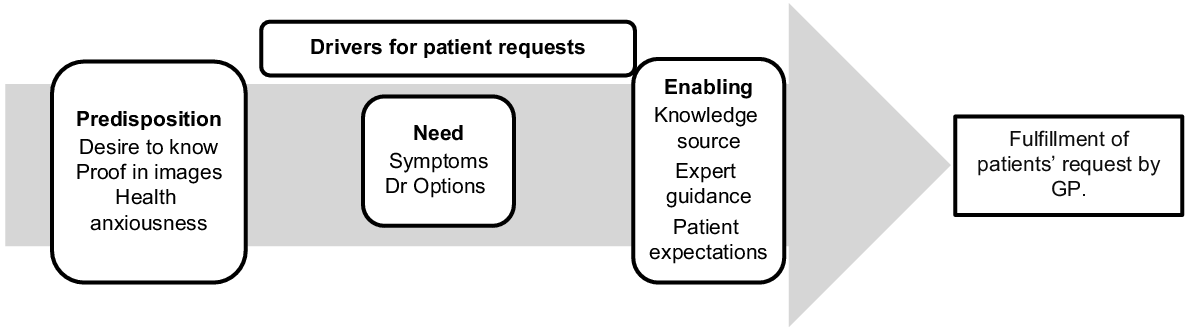
Fig. 1 indicates the steps that drive patients to request radiological referrals and demonstrates variables at play within clinical negotiations between patients and their GPs. These variables form the basis of patients having requests fulfilled.
Emerging themes from interviews and surveys with respect to drivers of patient requests. Adapted from a study by Kravitz et al. (2003), p. 1674.
Predisposition
Three psycho-social determinants that reflect predispositions of patients’ behaviour emerged as themes from our analysis. These included health anxiousness, proof of wellness in images and a desire to know.
Anxiousness about their health was the dominant driver for patients requesting referrals. This finding was reflected in both the surveys and interviews. Most participants expressed a level of anxiety or worry over their symptoms, in that they felt it could be something serious that they needed to address. In the survey responses, 75% of the total population (n = 60) were either anxious or worried. In cross-tabulating gender and health anxiousness, males (n = 12, 35%) and females (n = 7, 28%) indicated anxiousness over their health. Those aged 18–24 years (n = 4, 50%) were the least anxious, whereas those aged 35–44 years (n = 10, 41.7%) were the most anxious.
In the interviews and open-ended questions, participants explained, ‘I would chew myself out just thinking about what could be?’ (M, 18–24, U, E). Another interviewee affirmed, ‘It is helpful knowing I don’t have cancer’ (M, 35–44, HS, E). Integrating both methodologies, males are more anxious than females, although the qualitative data indicate that there is a broader age range of anxious individuals in the interviews compared to the surveys, where anxiousness was mostly seen in the 35–44 year age group.
Respondents indicated that they requested radiological scans because they wanted proof of wellness through imaging. This eased their concerns about their symptoms. For example, an obstetric ultrasound patient, concerned about a miscarriage, was reassured by a live image of her baby’s beating heart. She wrote in the open-ended section of the survey, ‘It became less stressful for me once I knew bubby was okay with a heartbeat’ (F, 25–34, HS, E). Similarly, one interviewee stated, ‘So, I said (to the doctor) … the best way to learn about what’s happening with my anatomy is through X-rays’ (F, 35–44, U, UE), while another commented, ‘It is just two pictures. And they can confirm if I have a potentially dangerous, serious respiratory condition’ (M, 18–24, U, E). Both surveys and interviews confirmed patients’ desires to see proof of their wellness in images.
Participants justified their requests, having researched their symptoms online, indicating that they were knowledgeable about their conditions prior to visiting the doctor. Their confidence increased when their doctor granted their request and validated their need for imaging. In his interview, one participant with a medical background expressed, ‘I just rely on my own medical knowledge. Yes. And then if I feel like I need a referral for something or if I’m not 100% sure, with my provisional diagnosis, then I will consult help’ (M, 25–34, PG, E). Meanwhile another interviewee stated, ‘I told the doctor, I’m not sure what’s wrong but I think its patella tendonitis and they said yes. Then I said, maybe I should get a scan – an MRI and I got a referral for that’ (M, 25–34, U, E). In the open-ended questions of the survey one participant was confident about their requests, ‘I don’t make frivolous requests and we always discuss the relevance of the tests’ (F, 65–74, D, R). Such confidence in their medical knowledge was reflected in both surveys and interviews. One of the survey prompts was ‘I always consult the internet for health advice’. The majority of those who answered positively (n = 9, 60%) had completed university level education. These individuals were mostly employed (n = 26, 62%) and in the age bracket 34–44 years (n = 14, 61%).
Enabler
Themes emerging from our study indicated that participants acknowledged the accessibility of resources through online sources and recognised the need for medical expertise in guiding their decision-making. However, these individuals also expected their requests to be met.
Participants indicated in the survey that they often searched Google to expand their knowledge base, as shown in Table 2, and those interviewed were confident that their sources were mostly from reputable sites. According to the interviewees, sites such as PubMed, Harvard Medical School or the Mayo Clinic, had reliable, researched content with sound evidence-based medical information. Interviewees stated, ‘I … go to PubMed and to Google Health and just read journals’ (F, 35–44, U, UE), another pointed out ‘I don’t search by subject. I search by author because they are experts in the field’ (M, 35–44, U, E).
| Prompt to search websites (n = 60) | n (%) |
|---|---|
| When the need arises | 35 (58.3) |
| Regularly, I want to keep on top of things | 11 (18.3) |
| Occasionally for curiosity | 10 (16.7) |
| Rarely | 4 (6.7) |
| Total | 60 (100) |
Participants were asked to select one option that was most applicable.
Table 2 indicates the response to the question ‘How often do you consult online sources for health information? Please indicate your most frequent reason’. Most looked when the need arose, such as when experiencing certain symptoms. However, participants in the interview also acknowledged the dangers of non-evidence-based online information, for example, one of the interviewees acknowledged, ‘Always a bit worried about being like Dr. Google’ (F 35–44, U, E). Another participant was disturbed by social media influencers advising their audience, ‘A lot of people thanks to social media and Tik Tok … are to blame … all these people suddenly have become experts … I mean, same with COVID-19. If anything, COVID-19 has taught us … how people, ordinary people, would give medical advice about COVID-19 …’ (F, 35–44, U, UE). Although the interviews indicated participants were cautious with online information, the surveys reflected greater value in consulting sites when needed.
Although patients were confident in their self-diagnosis, they often turned to their doctors for confirmation, validation and expert guidance. For example, some participants in the interviews researched their condition and then informed the doctor on the latest available treatments but wanted the doctor to guide them in making their final medical choices. Participants in the interview agreed, ‘I started listening …, sometimes we must unlearn what we’ve learned to become better patients. When we think we know too much …, we don’t in fact do and we let the experts guide us’ (M, 35–44, U, E). A migraine sufferer appreciated the GPs assertiveness, ‘… and if she says, no, you don’t need it. I will always trust what the doctor says, but that’s, why I guess I like her’ (F, 45–54, U, E).
Although some participants in the interviews appreciated their doctors’ assertiveness in refusing certain requests, many survey respondents (n = 52, 85%) indicated that their doctors accommodated their requests. When asked in the survey if their doctors addressed their requests, the majority of those who did not have regular doctors (n = 5, 71%) stated that the doctor was happy to provide a referral without any questions. For those with a regular doctor, most survey respondents (n = 32, 60%) stated the doctor was happy to write a referral but wanted to discuss the requested study in more detail. Although our qualitative data indicated participants were seeking expert guidance, those in the survey had their requests fulfilled, particularly individuals seeing a regular doctor. Although these regular doctors wanted to discuss in detail the requested study, they still met their patients’ expectations.
Participants felt the need to share their health information findings or self-diagnosis with an expectation for validation and acceptance from their doctors. When this validation was not given, participants indicated dissatisfaction with their doctors. However, both survey and interview data indicated doctors mostly fulfilled participants’ expectations, and when doctors did not, some participants opted to see an alternative doctor who would oblige. In sharing their self-diagnosis, participants in the interview expressed, ‘I just looked to different websites saying the symptoms that I had … and all indicated that I had a broken wrist. I told the doctor I’d like to get an X-ray on my wrist – he agreed with me’ (M, 45–54, U, E). However, when this validation was not given, participants were disappointed; as answered by one interviewee, ‘But the doctors seem to just brush away my concerns … And whenever that happens, I am sure I can speak for other patients as well. If that happens to us, we will simply just find another doctor’ (M 18–24, U, E). Table 3 shows cross tabulation of survey respondents’ satisfaction with doctors’ response to their requests.
| Number of participants (n) and percentage (%) | |||
|---|---|---|---|
| ‘Yes’ n (%) | ‘No’ n (%) | Total n (%) | |
| How did your doctor respond when you asked for a referral involving a radiological test or procedure? | |||
| He was happy to write a referral but wanted to discuss in detail the test/procedure with me | 28 (53.8) | 6 (75) | 34 (56.7) |
| He was happy to provide a referral without any questions. | 24 (46.2) | 2 (25) | 26 (43.3) |
| Total | 52 (100) | 8 (100) | 60 (100) |
Need
According to the ANM, the most immediate cause of healthcare utilisation is the need for service, that is, the perceived need recognised by patients (Andersen and Newman 2005). These causes were identified in our study as patients’ experience of symptoms and having options to choose alternative doctors.
Most of the survey responses, as well as the thematic analysis of both interview and open-ended questions on surveys, indicated it was patients’ experiences of symptoms that initiated the request. Symptoms associated with a new undiagnosed concern were often linked to patients’ outlook on their health and lifestyle, and initiating a scan was a way of health restoration. One participant with a sore knee explained, ‘It wasn’t the same pain I had before when I had the dislocation’ (F, 26, HS E). Another interviewee participant recalled something learnt from his university days to which he attributed his recent experience, ‘I was getting some chest pain … in university I studied that, with my type of body, I’m prone to developing pneumothorax’ (M, 18–24, U, E).
Descriptive statistics indicated that indeed most participants were concerned about a new/undiagnosed symptom, as shown in Table 4.
| Reasons (n = 60) | n (%) |
|---|---|
| A new, undiagnosed health concern/experiencing recent symptoms | 34 (56.7) |
| A chronic condition | 15 (25.0) |
| A scan to rule out an illness/disease that you read or heard. | 3 (5.0) |
| Own response. | 8 (13.3) |
| Total | 60 (100) |
Participants were asked to select one option that was most applicable.
Some participants even went as far as challenging the doctors’ advice, with one interviewee valuing the opinions of a specialist, ‘That’s what a lot of patients do … they demand to see specialists rather than general practitioners … you know, I’m not sure if you’ve noticed it, but a lot of people demand to see specialists because they find specialists are more knowledgeable about things’ (F, 35–44, U, E). Some interview respondents were keen on requesting a second or third opinion and in fact encouraged it, with one participant seeking different doctors’ expertise, ‘It looks like I’m doctor shopping which is terrible … I don’t have any extensive relationships with any GPs’ (M, 25–34, PG, E).
In assessing for the need element of the ANM, a new undiagnosed condition or symptomatic presentation was the main driver for initiating requests. Although participants had sought expert advice, they were quite firm in indicating that if their perceived need was significant and not met, they would be happy to seek alternative GPs.
Whether these individuals saw their doctors regularly or for the first time, most patients had their request approved, as indicated in Table 5 below. Overall, participants self-reported achieving intended, desired outcomes from their requests for radiological studies.
| Self-reported outcome (n = 60) | n (%) |
|---|---|
| Yes, my request proved useful | 48 (80) |
| No, I did not benefit from my request | 9 (15) |
| Own response | 2 (3.3) |
| I did not have the test as my doctor refused the request. | 1 (1.7) |
| Total | 60 (100) |
Participants were asked to select one option that was most applicable.
Discussion
This study aimed to understand, through cross-sectional surveys and semi-structured interviews, key findings during doctor–patient clinical negotiations when patients request a radiological referral from their doctors in primary care facilities. The results showed that participants were well-informed about their health and desired visual proof of wellness to alleviate their anxiety over new symptoms. The study found that visual proof, predominantly using X-rays and ultrasounds, played a vital role in satisfying patients’ needs. Most participants sourced information from reputable online sites and felt validated by their doctors, indicating that they were not making unnecessary requests. For example, in our study, visual proof through real-time ultrasound technology helped a mother see her baby’s beating heart and provided reassurance. The participant stated that seeing the images on the screen enabled her to visualise in her mind what was happening within her. Participants espoused the view that care has been received, once images were acquired, so both the GP and the participant could assess the cause for concern. This is in contrast to a study on consumer needs by Lee et al. (2015) who found almost half their population reported at least some difficulty locating desired health information (Lee et al. 2015). However, according to Jutel (2017), using online sourced information has several caveats, one of which is in ‘playing Dr Google’, where patients’ incorrectly self-diagnose and potentially influence the doctor’s better judgement (Gransjøen et al. 2018; Docking et al. 2022).
However, using the ANM to assess clinical requests in office practices, Kravitz et al. (2003) concluded that patients do in fact influence the clinical outcome during consultations. Their results supported the notion that patients’ requests are increasingly pervasive and there is a need to better understand and manage such requests, particularly non-clinically indicated requests. The ANM posits that healthcare use is determined and often weighted by the individuals’ beliefs. For example, the patients’ attitudes about health services, their desire to know about diseases and how they position themselves within the system of healthcare use (Andersen and Newman 2005). Our study indicates that participants are actively seeking resources, notably evidence-based websites, that grant them confidence in requesting certain tests or procedures. Such confidence in a consumeristic patient leads to higher expectations during consultations. Where such expectations involve doctors recognising and validating their requests, and if such acknowledgement is not granted, participants are willing to seek alternate doctors to fulfil their requests.
However, we recognise that granting patient-initiated requests, particularly with non-clinically indicated tests, may be seen as depleting doctors’ valuable time and healthcare resources (Llanwarne et al. 2017). Our study does not highlight the negative impact of patient influence causing unnecessary testing, interventions and possibly delayed diagnosis and poor stewardship of healthcare resources (Le et al. 2018; Walderhaug et al. 2022). Although patients’ expectations for doctors to recognise and validate their requests, particularly for non-clinically indicated tests, seem to be prevalent in our study, employing strategies to discourage unwarranted imaging, such as using a ‘watch and wait’ strategy (Fenton et al. 2021) or suggesting alternatives, may prove beneficial to decrease healthcare costs (Docking et al. 2022) However, doctors’ inclination towards patient satisfaction and practicing defensive medicine may contribute to responding favourably to patient requests (Nilsen and Malterud 2017).
Interestingly, Jerant et al. (2018) undertook a cross-sectional observational study on clinicians denying patient requests on 1319 clinical visits made to 56 doctors by 1141 outpatients. The study found most participants reported their request being fulfilled, n = 1441 (85%), and of the visits within the requested categories, there were 153 (11%) radiological requests. But some participants understood the doctors’ gatekeeping role and tried to remain ‘a patient’ (Kravitz et al. 2003). However, overall, seeing a doctor seems to have become a formality to secure a referral letter, rather than relying on the doctors’ knowledge and guidance (De Silva et al. 2023). This study, albeit small, found that doctors, in competing for patient satisfaction, maintaining relationships and keeping pace with clinical productivity, tend to adopt a default approach of agreeing to patient requests (Sabbatini et al. 2014; Carey et al. 2015).
Thus, in answering our objectives, themes emerging from our study were mapped onto the ANM as ‘predisposing’, ‘enabling’ and ‘need’ elements for patients requesting radiological imaging. The predisposing elements were desire to know, proof in images and health anxiousness. The enabling elements included knowledge source, expert guidance and patient expectations, while the need factors included symptoms and ‘Dr options.’ Our study found that the primary driver for requesting referrals was anxiousness over new undiagnosed illness or experience of symptoms where visual proof was needed mainly through X-rays and ultrasounds. Such visual proof satisfied individuals to pursue goals in restoring their health and wellness. Furthermore, our study supported the idea that participants were satisfied achieving the intended, desired outcomes, and if requests were not met, participants were inclined to choose an alternative doctor who would fulfil their request.
Limitations and strength
This study has several limitations that should be considered when interpreting the results. Firstly, the data was limited to the Australian population and within the context of a health system providing predominantly ‘free’ imaging services to patients. Secondly, it was collected retrospectively relying on participants’ recall, which could introduce bias, affect the accuracy and may tend to allow overinterpretation of findings. Additionally, the study only investigated participants’ views, and it would be valuable to assess doctors’ perspectives to gain a more comprehensive understanding of the issue. Moreover, the recruitment of participants was conducted online using Qualtrics and limited to purposively sampled participants requesting referrals from a GP working in primary care facilities. This could potentially skew the results and limit the generalisability of the findings to the broader Australian population. Our study also did not address whether GP’s performance was reflective of the proportion of tests ordered, which may influence GP’s responses to patients requests.
Our study did employ a mixed method approach, which provided valuable insights into patients’ perspectives. The quantitative component was employed to bring a broad approach to the research question while using the interview responses to gain more depth. Additionally, further research could confirm these results, and investigate full paying patients who are not covered under Australian Government’s Medicare health insurance rebate to determine if frequency of requests would be different to those who absorb little to no costs. Moreover, further investigation could determine if responses from GPs would be similar to those of our study.
Conclusion
This paper identifies several elements that are involved in clinical negotiations between patients and doctors. The ANM was used in the study as a way of explaining the use of health care within the Australian population, in particular, where patients request imaging referrals from their GPs in a primary care setting. Our findings suggest that patients are more informed than ever before and are confident in their knowledge of the types of radiological scans and interventions they require. Patients also found comfort in seeing what was happening inside their bodies, particularly during obstetric imaging, and wanted their doctors to validate their concerns by complying with their requests for imaging referrals. While our study did not highlight the importance of appropriate use of imaging, particularly for non-clinically indicated tests, it recognised the increasing involvement of patients as healthcare participants. Overall, our study provides some new insights into the evolving patient–doctor dyadic relationship in radiological services.
References
Alamri AF, Khan I, Baig MIA, Iftikhar R (2014) Trends in ultrasound examination in family practice. Journal of Family and Community Medicine 21, 107-111.
| Crossref | Google Scholar |
Andersen RM (1995) Revisiting the behavioral model and access to medical care: does it matter? Journal of Health and Social Behavior 36, 1-10.
| Crossref | Google Scholar |
Andersen R, Newman JF (1973) Societal and individual determinants of medical care utilization in the United States. The Milbank Memorial Fund Quarterly. Health and Society 51, 95-124.
| Crossref | Google Scholar |
Andersen R, Newman JF (2005) Societal and individual determinants of medical care utilization in the United States. The Milbank Quarterly 83, 1-28.
| Crossref | Google Scholar |
Benetoli A, Chen TF, Aslani P (2018) How patients’ use of social media impacts their interactions with healthcare professionals. Patient Education and Counseling 101, 439-444.
| Crossref | Google Scholar |
Bradley EH, McGraw SA, Curry L, Buckser A, King KL, Kasl SV, Andersen R (2002) Expanding the Andersen model: the role of psychosocial factors in long-term care use. Health Services Research 37, 1221-1242.
| Crossref | Google Scholar |
Carey M, Turon H, Goergen S, Sanson-Fisher R, Yoong SL, Jones K (2015) Patients’ experiences of the management of lower back pain in general practice: use of diagnostic imaging, medication and provision of self-management advice. Australian Journal of Primary Health 21, 342-346.
| Crossref | Google Scholar |
De Silva L, Baysari M, Keep M, Kench P, Clarke J (2023) Patient requests for radiological services: an Australian study of patient agency and the impact of online health information. Health Promotion Journal of Australia 34, 437-442.
| Crossref | Google Scholar |
Docking S, Haddock R, Buchbinder R (2022) Australian health policies related to diagnostic imaging: too much of a good thing? Australian Health Review 46, 635-638.
| Crossref | Google Scholar |
Esen E, Aslan M, Sonbahar BÇ, Kerimoğlu RS (2019) YouTube English videos as a source of information on breast self-examination. Breast Cancer Research and Treatment 173, 629-635.
| Crossref | Google Scholar |
Fenton JJ, Franks P, Feldman MD, Jerant A, Henry SG, Paterniti DA, Kravitz RL (2015) Impact of patient requests on provider-perceived visit difficulty in primary care. Journal of General Internal Medicine 30, 214-220.
| Crossref | Google Scholar |
Fenton JJ, Jerant A, Franks P, Gosdin M, Fridman I, Cipri C, Weinberg G, Hudnut A, Tancredi DJ (2021) Watchful waiting as a strategy to reduce low-value spinal imaging: study protocol for a randomized trial. Trials 22, 167.
| Crossref | Google Scholar |
Fiksdal AS, Kumbamu A, Jadhav AS, Cocos C, Nelsen LA, Pathak J, McCormick JB (2014) Evaluating the process of online health information searching: a qualitative approach to exploring consumer perspectives. Journal of Medical Internet Research 16, e224.
| Crossref | Google Scholar |
Gransjøen AM, Wiig S, Lysdahl KB, Hofmann BM (2018) Barriers and facilitators for guideline adherence in diagnostic imaging: an explorative study of GPs’ and radiologists’ perspectives. BMC Health Services Research 18, 556.
| Crossref | Google Scholar |
Groß D, Schmidt M (2018) E-Health und Gesundheitsapps aus medizinethischer Sicht. Bundesgesundheitsblatt - Gesundheitsforschung - Gesundheitsschutz 61, 349-357.
| Crossref | Google Scholar |
Hodyl NA, Hogg K, Renton D, von Saldern S, McLachlan R (2020) Understanding the preferences of Australian men for accessing health information. Australian Journal of Primary Health 26, 153-160.
| Crossref | Google Scholar |
Hogue M-CB, Doran E, Henry DA (2012) A prompt to the web: the media and health information seeking behaviour. PLoS ONE 7(4), e34314.
| Crossref | Google Scholar |
Hsieh H-F, Shannon SE (2005) Three approaches to qualitative content analysis. Qualitative Health Research 15, 1277-1288.
| Crossref | Google Scholar |
Jerant A, Fenton JJ, Kravitz RL, Tancredi DJ, Magnan E, Bertakis KD, Franks P (2018) Association of clinician denial of patient requests with patient satisfaction. JAMA Internal Medicine 178, 85-91.
| Crossref | Google Scholar |
Jutel A (2017) “Dr. Google” and his predecessors. Diagnosis 4(2), 87-91.
| Crossref | Google Scholar |
Kravitz RL, Bell RA, Azari R, Kelly-Reif S, Krupat E, Thom DH (2003) Direct observation of requests for clinical services in office practice: what do patients want and do they get it? Archives of Internal Medicine 163, 1673-1681.
| Crossref | Google Scholar |
Le HH, DeCamp M, Bertram A, Kale M, Berger Z (2018) Influences on primary care provider imaging for a hypothetical patient with low back pain. Southern Medical Journal 111, 758-762.
| Crossref | Google Scholar |
Lee K, Hoti K, Hughes JD, Emmerton L (2014) Dr Google and the consumer: a qualitative study exploring the navigational needs and online health information-seeking behaviors of consumers with chronic health conditions. Journal of Medical Internet Research 16, e262.
| Crossref | Google Scholar |
Lee K, Hoti K, Hughes JD, Emmerton LM (2015) Consumer use of “Dr Google”: a survey on health information-seeking behaviors and navigational needs. Journal of Medical Internet Research 17, e288.
| Crossref | Google Scholar |
Llanwarne N, Newbould J, Burt J, Campbell JL, Roland M (2017) Wasting the doctor’s time? A video-elicitation interview study with patients in primary care. Social Science & Medicine 176, 113-122.
| Crossref | Google Scholar |
Nilsen S, Malterud K (2017) What happens when the doctor denies a patient’s request? A qualitative interview study among general practitioners in Norway. Scandinavian Journal of Primary Health Care 35, 201-207.
| Crossref | Google Scholar |
Palanica A, Flaschner P, Thommandram A, Li M, Fossat Y (2019) Physicians’ perceptions of chatbots in health care: cross-sectional web-based survey. Journal of Medical Internet Research 21, e12887.
| Crossref | Google Scholar |
Paterniti DA, Fancher TL, Cipri CS, Timmermans S, Heritage J, Kravitz RL (2010) Getting to “no”: strategies primary care physicians use to deny patient requests. Archives of Internal Medicine 170, 381-388.
| Crossref | Google Scholar |
Petrovic K, Blank TO (2015) The Andersen-Newman Behavioral Model of Health Service Use as a conceptual basis for understanding patient behavior within the patient-physician dyad: the influence of trust on adherence to statins in older people living with HIV and cardiovascular disease. Cogent Psychology 2, 1038894.
| Crossref | Google Scholar |
Sabbatini AK, Tilburt JC, Campbell EG, Sheeler RD, Egginton JS, Goold SD (2014) Controlling health costs: physician responses to patient expectations for medical care. Journal of General Internal Medicine 29, 1234-1241.
| Crossref | Google Scholar |
Strain LA (1990) Physician visits by the elderly: testing the andersen-newman framework. Canadian Journal of Sociology 15, 19-37.
| Crossref | Google Scholar |
Walderhaug KE, Nyquist MK, Mjølstad BP (2022) GP strategies to avoid imaging overuse. A qualitative study in Norwegian general practice. Scandinavian Journal of Primary Health Care 40, 48-56.
| Crossref | Google Scholar |


