The health of Hunter Valley communities in proximity to coal mining and power generation, general practice data, 1998–2010
Tony D. Merritt A D , Michelle A. Cretikos B , Wayne Smith C and David N. Durrheim AA Hunter New England Population Health
B Centre for Epidemiology and Evidence, NSW Ministry of Health
C Environmental Health Branch, Health Protection NSW
D Corresponding author. Email: Tony.Merritt@hnehealth.nsw.gov.au
NSW Public Health Bulletin 24(2) 57-64 https://doi.org/10.1071/NB12109
Published: 7 November 2013
Abstract
Aim: An analysis of general practice data for rural communities in close proximity to coal mining and coal-fired power generation in the Hunter Valley region of NSW was conducted to identify unusual patterns of illness. Methods: Bettering the Evaluation and Care of Health general practice consultation data from the Hunter Valley region for 1998–2010 were compared with data from all other rural NSW residents. Results: There were no significantly higher rates of problems managed or medications prescribed for Hunter Valley region residents compared with the rest of rural NSW. Rates of respiratory problem management in the Hunter Valley region did not change significantly over time, while for all other rural NSW areas these rates significantly decreased. Conclusion: There was no evidence of significantly elevated health issues for residents in the Hunter Valley region of NSW. The diverging trend for respiratory problem management over time is worthy of further exploration.
Coal mining has the potential to impact on the health of nearby residents but there are limited Australian data available.1,2 The rural communities of Singleton, Muswellbrook and Denman are situated in close proximity to extensive and expanding coal mining and coal-fired power generation activities in the Hunter Valley region of New South Wales (NSW). Raw coal production from open cut coal mines in NSW increased by 81% over the period 1999–2011, with the Hunter Valley region accounting for 76% of all open-cut coal production in NSW in 2011 (unpublished data, Coal Services Pty Ltd, 2012).
In response to health concerns raised by the community, NSW Health reviewed existing health data for the region. Patterns of NSW emergency department presentations and hospital admissions, as well as mortality, cancer incidence and self-reported health survey data for these areas were compared with other parts of NSW and an analysis published in May 2010.3 Some regions with exposure to open-cut coal mining and power generation were shown to have higher rates of emergency department attendance for asthma and respiratory disease, and higher rates of hospital admission for asthma, respiratory conditions and cardiovascular disease. There was ongoing community concern that hospital data only represented severe disease.
A complementary analysis of general practice data was conducted to determine whether there were any indications of excessive or unusual patterns of illness in these communities which may not have been detected by the May 2010 study.
Methods
Data were obtained from the Bettering the Evaluation and Care of Health (BEACH) program.4 The BEACH program collects data from approximately 1000 general practitioners (GPs) randomly selected from across Australia each year. Each GP contributes details of 100 consecutive patient encounters, including the problems managed and treatment provided. Additional health data are collected on sub-samples of these encounters.
Problems managed are classified using the International Classification of Primary Care, version 2 (ICPC-2).5 This classification system groups health problems into problem chapters and components, and medications into groups and sub-groups.
BEACH GP consultation data for residents of Singleton, Muswellbrook and Denman were compared with data for all other rural (non-metropolitan) NSW residents for three time periods: 1998–2004 and 2005–2010 inclusive, and for both time periods combined. Additionally, data for residents of Singleton, Muswellbrook and Denman for the period 2005–2010 were compared with data from the 1998–2004 period. This represented all available BEACH data for this region.
Patient postcode of residence was used to define their location. The communities of Singleton (postcode 2330), Muswellbrook (postcode 2333) and Denman (postcode 2328) were combined as the communities of interest in the Hunter Valley region for the purposes of this paper. Rural NSW was defined using the Australian Standard Geographic Classification (ARIA+) system of the Australian Bureau of Statistics.6
For each of the three time periods, the analyses included a crude analysis, with adjustment for clustering at GP level, and weighted analysis, which included individual-level adjustment for:
-
patient sex and age group (0–14, 15–64, and 65 years and over)
-
patient’s Health Care Card status
-
season of encounter date, using four season categories.
Health Care Card status was used as a proxy for socioeconomic status but Veterans’ Card status was not available. The weighting procedure used all other rural NSW postcodes, excluding Singleton, Muswellbrook and Denman, as the reference population.
All direct encounters with a GP for both new and existing problems managed were included. The analysis examined the problems managed as recorded by the GP, presented as a rate per 100 encounters, with 95% confidence intervals (CI), for all conditions and diagnostic chapter headings. The analysis also examined the medications prescribed or supplied by the GP per 100 problems managed, with 95% CIs, presented by medication group and sub-group. The medication analysis used problems managed for the denominator because more than one problem could be managed per encounter and the number of problems managed per encounter increased over time. All CI calculations accounted for the clustered sample design.
All available BEACH data were considered. Respiratory and cardiovascular disease, malignancy and mental health issues were of particular interest on the basis of known potential impacts from particulate pollution and local community concerns.
Differences between the Hunter Valley region and rural NSW (excluding the Hunter Valley region) were considered significant when there was no overlap of the 95% CIs between the regions. The clustered sample design and nature of the data prevented further significance testing.
Spearman’s rank correlation test was used to detect differences in the ranking of rates of problems managed and medications prescribed between the weighted Hunter Valley region data and the comparison rural NSW data. A p < 0.05 was used to reject the null hypothesis (that the rank orders were independent) and indicated that there was no significant difference in the ranking of problems managed or medications prescribed between the two groups.
Individual-level smoking status was not available for all GP encounters, and therefore could not be used to adjust results at individual level. Instead, the sub-sample of BEACH encounters with smoking status information (approximately 33% of encounters) was used to estimate the prevalence of current, previous and never smoked status for residents in the Hunter Valley region and in the rest of rural NSW for the time periods of interest.
The number of different GPs and general practices in the Hunter Valley region that contributed BEACH data during 1998–2010 was examined, as was the proportion of encounters provided by each participating GP.
Ethics approval was not required for this review. The BEACH program provided aggregate de-identified data.
Results
Patient characteristics
During the period April 1998–July 2010, the BEACH survey program included records of 2286 encounters and 3448 problems managed for Hunter Valley region residents. No BEACH data were available for this region prior to 1998. The unweighted Hunter Valley region sample had more patients in the 0–15 and 15–64-year age groups, and fewer Health Care Card holders than the comparison rural NSW sample (Table 1).
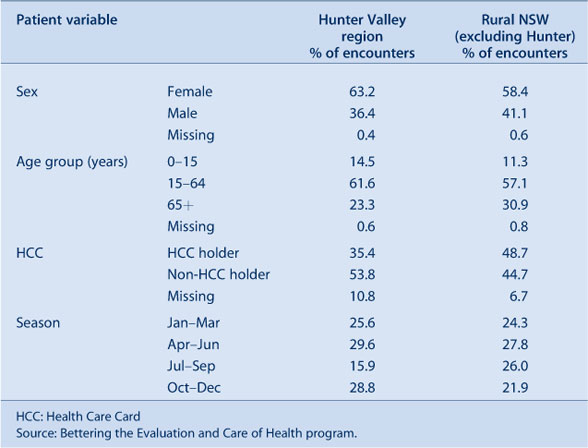
|
Eighteen different GPs from seven general practices contributed data in the Hunter Valley region. The median proportion of encounters with Hunter Valley region residents provided by each GP was 3.9% (range: 1.3–11.4%). Ninety-one percent of consultations for Hunter Valley region residents occurred in the Hunter region.
There were 89 614 encounters and 140 645 problems managed for residents in the remainder of rural NSW during this period.
Problems managed
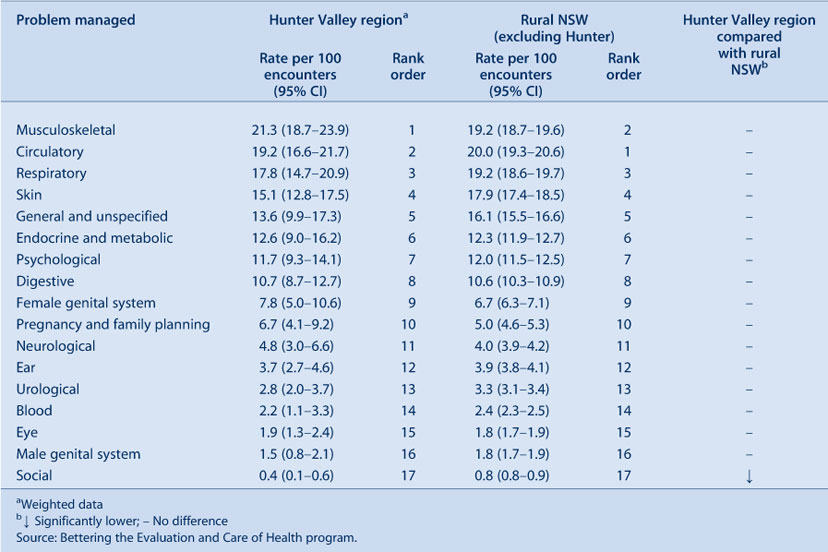
When grouped by ICPC-2 chapter, no problem groups were managed at significantly higher rates in the Hunter Valley region (Table 2). Social chapter problems were managed at a significantly lower rate.
|
There was no significant difference in the ranking of problem chapters (Spearman’s rho = 0.998, p < 0.0001).
When the most frequently managed problems were compared, none were managed at significantly higher rates in the Hunter Valley region (Table 3). The rate for general check-ups was significantly lower in the Hunter Valley region.

|
There were no significant differences in management rates of asthma, acute or chronic respiratory tract conditions, depression or anxiety.
There were no significant differences in the ranking of all tabulated problems or for the top 10 problems managed (Spearman’s rho = 0.86 (p < 0.0001) and 0.71 (p < 0.02) respectively) (Table 3).
Medications prescribed or supplied
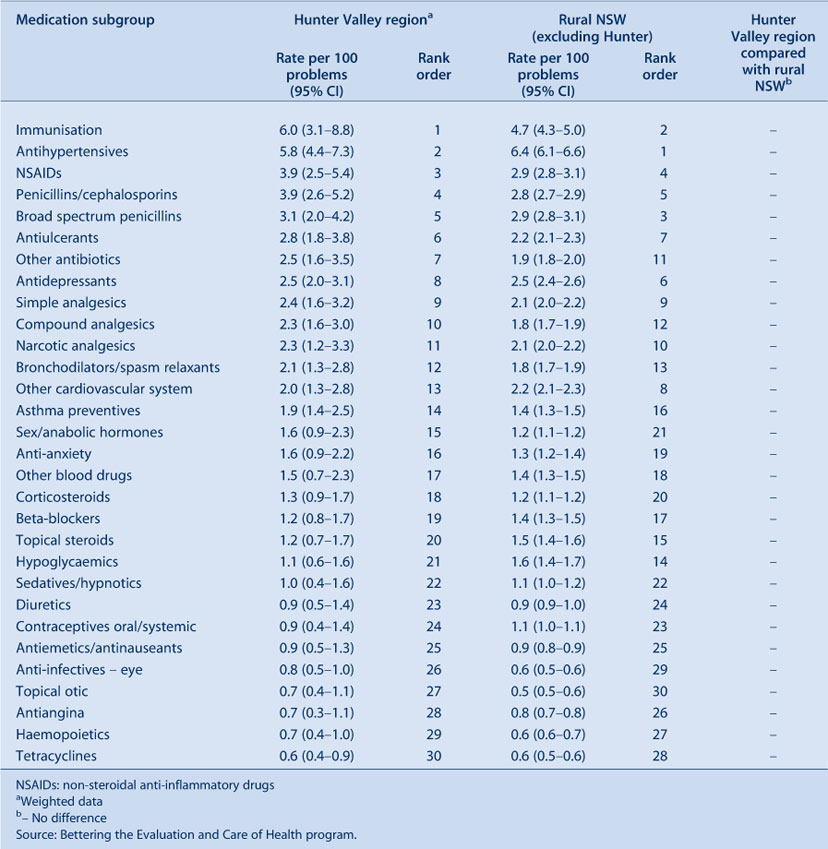
No medication groups were prescribed or supplied at significantly higher or lower rates in the Hunter Valley region (Table 4).

|
The rank order was very similar for the two groups (Spearman’s rho = 0.98, p < 0.0001, Table 4).
Similarly, no medication subgroups were prescribed or supplied at significantly higher or lower rates in the Hunter Valley region (e.g. bronchodilators, asthma preventives, anti-anxiety and antidepressant medicines). The rank order was similar for the two groups (Spearman’s rho = 0.95, p < 0.0001) (Table 5).
|
Smoking
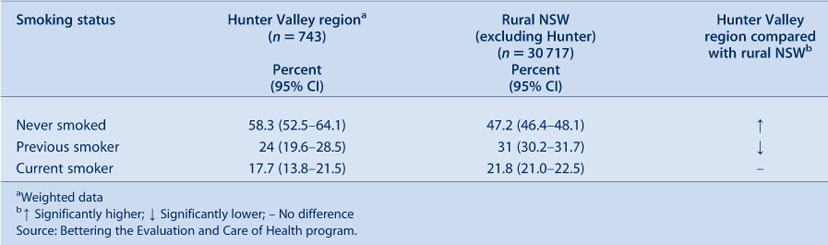
In the sub-sample (n = 743) with smoking data recorded, a significantly higher proportion of people had never smoked and a significantly lower proportion of people were previous smokers in the Hunter Valley region than in rural NSW (n = 30 171). The prevalence of current smoking was not significantly different (Table 6).
|
Additional analysis by time period
In addition to the analysis of aggregated data for the period 1998–2010, data were considered separately for the time periods April 1998–March 2004 and April 2004–June 2010. Comparison of Hunter Valley region weighted data with rural NSW for each period separately did not identify any information that differed substantially from the analysis presented for the combined period.
When weighted Hunter Valley region data for the two periods were compared, the only significant increase over time was in the rate of management of benign/uncertain neoplasms and malignant neoplasms, an increase that was also seen over this time period in the remainder of rural NSW.
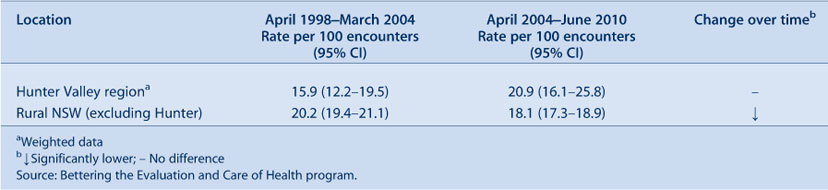
The rate of management of respiratory chapter problems in the Hunter Valley region did not change significantly over time. By comparison, the rate for the respiratory chapter problem group was significantly lower during the later period in the remainder of rural NSW (Table 7).
|
Discussion
Community members in the Hunter Valley region have expressed a broad range of health concerns, particularly in relation to perceived negative impacts of industrial activity, coal mining and power generation on respiratory and mental health.
Our analysis of general practice data found no evidence of significantly higher rates of any particular problems managed or medications prescribed or supplied for Hunter Valley region residents compared with the rest of rural NSW during the period 1998–2010.
Consistent with this, when rates of problems and medications were ranked, all rank tests were highly correlated (rho > 0.85) except for the top 10 problems managed, which were moderately correlated (rho = 0.71). All tests of independence of ranking between the weighted Hunter Valley region and rural NSW data were rejected, indicating no significant difference in ranking between these regions.
If the Hunter Valley region sample had been larger it is possible that significant differences in rates of management between the two regions may have been identified. However, the analysis included 12 years of data from the BEACH program, which were all the data available at the time of the analysis, and represents the only source of data for general practice activity in NSW available for this purpose.
The nature of the BEACH data constrains the statistical options available for further comparison of these groups. Identification of differences relied on the comparison of confidence intervals that take account of the clustering inherent in the data sample and the nature of the underlying data. The rates presented in Tables 2–5 and 7, for example, cannot be considered as proportions, as one encounter or problem can contribute multiple counts within the specific rate under consideration.
It is of interest that comparison of the management rates of respiratory problems (as a group) during the period 2005–2010 with those for 1998–2004 demonstrated no significant change in the Hunter Valley region despite a significant decrease for the remainder of rural NSW over this period. Again, if the Hunter Valley region sample were larger, a significant difference may have been identified.
A recent review of emergency department data found higher rates for asthma and respiratory disease presentations in this region when compared with Sydney residents, however higher rates were also noted for a number of rural communities with no potential mining or power generation exposures.3 A number of these communities have been affected by drought and the contribution of agricultural activity, meteorological conditions and wood-smoke have all been implicated.7
There were no significant differences in management rates of mental health conditions in the Hunter Valley region compared with the rest of rural NSW. Management rates of depression and anxiety were not higher, nor were prescription rates of antidepressants.
It was not possible to adjust for the influence of smoking at individual level during the analysis as this information was only available for 33% of patients. However, smoking prevalence is unlikely to explain any relative increase in the rate of respiratory disease managed in the Hunter Valley region as there was a significantly higher prevalence of adults who had never smoked and significantly fewer adults who were previous smokers compared with the rest of rural NSW.
We note a number of limitations of the data used for this analysis. The Hunter Valley region sample had a higher proportion of younger patients and fewer Health Care Card holders than the comparison group. These differences were accounted for in the weighting applied to the Hunter Valley region data used in the analysis. The lower rate of general check-ups for Hunter Valley region patients potentially reflects differences in health care utilisation. We are not aware of any other likely systematic differences between these groups.
The BEACH data used in this analysis necessarily rely on a sample of patient encounters from a sample of randomly selected GPs. However, the inclusion of data from 18 GPs representing seven practices suggests the Hunter Valley region data should not be unduly influenced by different diagnostic and prescribing practices of individual participating GPs.
Conclusion
There was no evidence of a significant difference in problems managed or medications prescribed by GPs for residents of communities potentially affected by heavy industrial activity (coal mining and power generation) in the Hunter Valley region of NSW compared with residents in the remainder of rural NSW during the period 1998–2010. The diverging trend for respiratory problem management over time is worthy of further exploration.
Acknowledgments
We thank Helena Britt for her assistance in obtaining the BEACH data used in this analysis and for reviewing the draft manuscript. The BEACH program is conducted by and the data were analysed by the Family Medicine Research Centre, The University of Sydney.
During the data years reported in this paper, the BEACH program was funded by financial contributions from: The Australian Government Department of Health and Ageing; AstraZeneca Pty Ltd (Australia); Janssen-Cilag Pty Ltd; Merck, Sharp and Dohme (Australia) Pty Ltd; Pfizer Australia; Abbott Australasia Pty Ltd; Sanofi-Aventis Australia Pty Ltd; Wyeth Australia Pty Ltd (2008–2010); Novartis Pharmaceuticals Australia Pty Ltd; GlaxoSmithKline Australia Pty Ltd; National Prescribing Service Ltd; Roche Products Pty Ltd; Aventis Pharma Pty Ltd; Australian Government Department of Veterans’ Affairs; National Occupational Health and Safety Commission; The Office of the Australian Safety and Compensation Council; and the Department of Employment and Workplace Relations.
References
[1] Castledon WM, Shearman D, Crisp G, Finch P. The mining and burning of coal: effects on health and environment. MJA 2011; 195 333–5.[2] Higginbotham N, Freeman S, Connor L, Albrecht G. Environmental injustice and air pollution in coal affected communities, Hunter Valley, Australia. Health Place 2010; 16 259–66.
| Environmental injustice and air pollution in coal affected communities, Hunter Valley, Australia.Crossref | GoogleScholarGoogle Scholar | 19884036PubMed |
[3] NSW Department of Health. Respiratory and cardiovascular diseases and cancer among residents in the Hunter New England Area Health Service. Available at: http://www.health.nsw.gov.au/pubs/2010/hne_respi_cardio.html (Cited 5 September 2012).
[4] Britt H, Miller GC, Charles J, Henderson J, Bayram C, Pan Y et al. General practice activity in Australia 2009–10. General practice series no 27. Cat. No. GEP 27. Canberra: Australian Institute of Health and Welfare; 2010.
[5] Classification Committee of the World Organisation of Family Doctors. ICPC-2. International Classification of Primary Care. 2nd ed. Oxford: Oxford University Press; 1998.
[6] Australian Bureau of Statistics. Census Paper 03/01. ASGC Remoteness Classification: Purpose and Use. Available at: http://www.abs.gov.au/websitedbs/d3110122.nsf/0/f9c96fb635cce780ca256d420005dc02/$FILE/Remoteness_Paper_text_final.pdf (Cited 5 September 2012).
[7] Centre for Inland Health. Particulate matter and air pollution in a NSW regional centre: A review of the literature and opportunities for action. Wagga Wagga: Charles Sturt University; 2011.

