The economics of HIV prevention strategies in NSW
James R. HalesNSW Public Health Bulletin 21(4) 61-64 https://doi.org/10.1071/NB10010
Published: 27 May 2010
Abstract
HIV in Australia was first diagnosed in NSW in the early 1980s, and has had a significant effect on public health. The NSW Government commenced its investment in HIV/AIDS in 1984 and the investment now encompasses research, primary and secondary prevention, and care, treatment and support for people living with HIV/AIDS. A recent study examined the historical impact of the HIV/AIDS epidemic and projected its future impact in NSW. The analysis indicates that the NSW HIV/AIDS investment program has been highly effective in reducing HIV transmission, and has also been cost effective in: avoiding future health-care costs; life years saved; and quality of life benefits. The analysis also indicates that any scaling back of prevention initiatives would result in an increase in the number of people living with HIV.
Human immunodeficiency virus (HIV) in Australia was first diagnosed in New South Wales (NSW) in the early 1980s. Since then, it has had a significant effect on public health; by the end of 2008, there had been 28 330 diagnoses of HIV infection, 10 348 diagnoses of acquired immunodeficiency syndrome (AIDS) and 6765 deaths following AIDS in Australia.1 Within Australia, approximately 56% of total HIV diagnoses have been reported in NSW.1
The NSW Government commenced its investment in HIV/AIDS in 19842 and it now encompasses research, primary and secondary prevention, and care, treatment and support for people living with HIV and AIDS. The investment program identifies priorities for reducing future infections among those populations considered at highest risk: gay men, people from culturally and linguistically diverse (CALD) backgrounds, Aboriginal people, people who inject drugs and sex workers. It also identifies priorities for improving the health of people living with HIV/AIDS, through population-level programs, individual clinical services, research and service development.
A recent study, funded by the NSW Department of Health, examined the historical impact of the HIV/AIDS epidemic and projected its future impact in NSW.3 This encompassed an analysis of the NSW investment in the public health response to HIV/AIDS, the morbidity and mortality arising from HIV/AIDS, and the economic impact of the epidemic in regard to clinical care costs, life years saved and quality of life outcomes. The National Centre in HIV Epidemiology and Clinical Research (NCHECR) undertook the epidemiological analysis, and Health Outcomes International (HOI) undertook the economic analysis. The methodology was based on that used in a previous cost-effectiveness study of needle and syringe programs in Australia.4 This article introduces some of the findings of the study. Copies of the full study are available on the NSW Department of Health website at: http://www.health.nsw.gov.au/resources/publichealth/sexualhealth/ImpactStatement_pdf.asp.
Epidemiological model
The study examined four identified population groups: homosexual men, injecting drug users, the general heterosexual population, and sex workers. For each group, historical trends in HIV transmission and the risk factors that affect transmission were studied. Models were then developed that compared a baseline scenario that reflected HIV transmission rates to date with preventive strategies in place with modelled alternative scenarios that assumed that no intervention strategies were in place other than antiretroviral therapy. Projections were then made that estimated the number of people living with HIV/AIDS under each scenario from 2005 to 2090, by which time those having HIV were estimated to have died. In scenarios where intervention measures for sexual transmission of HIV were absent, it was assumed that the absence of intervention measures accounted for 50% of the estimated change in levels of risk. For injecting drug users, the model assumed only the presence or absence of needle and syringe programs for its estimation of effect. Results of this analysis are presented in Table 1.

|
The total number of cases of HIV avoided between 1980 and 2005 was estimated at approximately 44 500 cases. This number represents an estimated 80% reduction in the number of new cases of HIV that would otherwise have occurred during this period. Injecting drug users comprised 75% of the total cases avoided, with homosexual men comprising 22%.
Separate projections were prepared for the period between 2006 and 2016 to assess the likely impact of terminating prevention initiatives from 2005 (Table 2). In these projections, it was assumed that 50% of the estimated benefits in terms of changes in levels of sexual risk behaviour still occur without the intervention.

|
Under the assumptions regarding the impact of cessation of these initiatives on risk behaviours among the various population groups, HIV incidence increased among all groups, particularly injecting drug users. In these projections, an additional 9100 cases of HIV were estimated to occur from 2006 to 2016 if the current prevention initiatives were to cease at the end of 2005. This would result in an additional 9000 people living with HIV in 2016, with an associated increase in clinical care costs for the remainder of their lifetimes.
Economic model
The economic analysis examined the investment made in HIV/AIDS by the NSW Department of Health since 1981, including funds allocated to preventive and clinical care services, together with the direct clinical care costs avoided as a result of the reduced incidence of HIV associated with the preventive activities.
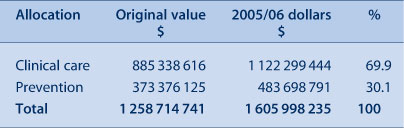
The NSW Department of Health provided data on funds allocated under the program from 1981/82 to 2005/06. Total program funding was then apportioned between clinical care and prevention (where the category was the primary function of the funding) (Table 3).
|
In total, an estimated $1259 million was allocated under the program from 1981/82 to 2005/06 ($1606 million in 2005/06 prices), with 70% allocated to clinical care and 30% to prevention activities. Prevention funds were then apportioned to the various target populations, based on analyses undertaken by the NSW Department of Health, with $355 million (2005/06 prices) allocated across the four study population groups.
The analysis of the return on the investment in preventive activities considered two aspects:
-
The financial value of the direct lifetime costs of clinical care of HIV avoided by the NSW Department of Health. The model applied standard unit clinical care costs to the 44 545 cases estimated as having been avoided to the end of 2005, until that cohort died. Direct clinical care costs were based on the previous study by Health Outcomes International and NCHECR, adjusted to 2005/06 prices.4 The analysis included a Net Present Value analysis which compared the funds invested with the returns from that investment, and applied a common discount rate to the various cashflows that relate to the activities associated with the investment. Under this approach, a project is potentially worthwhile (or viable) if the Net Present Value is greater than zero; i.e. the total discounted value of benefits is greater than the total discounted costs.
-
The life years and quality adjusted life years saved as a result of the preventive activities. The values used in this study were based on those used in the previous study of needle and syringe programs by Health Outcomes International and NCHECR, which were drawn from the extant literature.4–6
For an investment of $355 million between 1981 and 2005, a total of $18 027 million in clinical care costs would be avoided over the lifetime of those people who did not acquire HIV because of the preventive programs. The Net Present Value of these savings at a discount rate of 3% is $4629 million for the program as a whole. The Net Present Value is positive for three of the four components (homosexual contact, injecting drug use and heterosexual contact), but is negative (−$0.8 million) for sex worker contact. The negative result for sex worker contact is due to the relatively small number of cases avoided (Table 4). These results also hold true for alternative discount rates of 5% and 7%.

|
The second component of the economic model examined the life years and quality-adjusted life years saved as a result of the investment in preventive initiatives. A total of approximately 394 000 life years were expected to be gained over the lifetime of people avoiding HIV. Of the total life years saved, 55% relate to injecting drug users, with 38% attributed to homosexual men. Life year gains among heterosexual people account for a further 6%.
In regard to the impact on quality of life, an estimated 863 000 quality-adjusted life years (QALYs) are expected to be gained over the lifetime of people who would otherwise have acquired HIV. The distribution of these two outcomes over the lifetime of people avoiding HIV is illustrated in Figure 1.
A rudimentary comparison of these results with those for several other public health preventive initiatives aimed at reducing tobacco consumption and reducing coronary heart disease indicates that the HIV/AIDS investment program compares very favourably in regard to direct health care costs saved and total benefits derived relative to the funds invested.7 For example, the ratio of clinical care costs saved to funds invested in the HIV/AIDS program is estimated at 13:1 compared to 2:1 for tobacco reduction strategies, while the ratio of total benefits to funds invested for HIV/AIDS is 189:1 compared to 49:1 for tobacco reduction strategies. These results are also consistent with the recent study on the cost effectiveness of needle and syringe programs in Australia.8
Conclusion
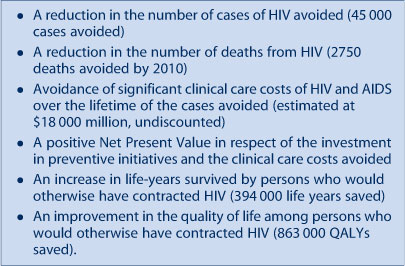
The NSW Government investment program in HIV/AIDS has been a major public health initiative, and has been in place since the early 1980s. It has sought to achieve a balance in funding allocations between clinical care and treatment services and preventive activities. The analysis of the effectiveness of the program indicates that it has been highly successful (see Box 1). The analysis also indicates that continued investment in the preventive initiatives of the program can be expected to continue to provide benefits in each of these areas into the future.
|
[1]
[2] Stewart K, Penny R. Containing HIV in NSW: a world class success. NSW Public Health Bull 2003; 14(3): 57–9.
| Crossref | GoogleScholarGoogle Scholar | (Accessed 8 March 2010.)
[4]
[5] Tengs TO, Wallace A. One thousand health-related quality-of-life estimates. Med Care 2000; 38(6): 583–637.
| Crossref | GoogleScholarGoogle Scholar | PubMed | CAS |

[6] Holtgrave DR, Pinkerton SD. Updates of cost of illness and quality of life estimates for use in economic evaluations of HIV prevention programs. J Acquir Immune Defic Syndr Hum Retrovirol 1997; 16 54–62.
| PubMed | CAS |

[7]
[8]


