Estimate of the number of Campylobacter infections in the Hunter region, NSW, 2004–2007
April R. Roberts-Witteveen A C , David N. Durrheim B , Tony D. Merritt B and Sally A. Munnoch AA OzFoodNet, Hunter New England Area Health Service
B Health Protection, Hunter New England Area Health Service
C Corresponding author. Email: lirpa_r@yahoo.com
NSW Public Health Bulletin 20(12) 187-191 https://doi.org/10.1071/NB09009
Published: 4 February 2010
Abstract
Objectives: Campylobacteriosis is not notifiable in NSW and the number of cases of Campylobacter disease is thus not well described. Methods: De-identified campylobacteriosis records for 2004–2007 were requested from laboratories in the Hunter region of NSW. Based on notifying laboratory, a Salmonella notification weighting was applied to laboratory-confirmed campylobacteriosis cases to provide an overall estimate of Campylobacter disease in the area. Results: The estimated median of the annual number of laboratory-confirmed campylobacteriosis cases was 788 (range 700–1022). The ratio of estimated Campylobacter cases to Salmonella notifications was 5.5 : 1. Conclusion: Campylobacter infection causes considerable disease in the Hunter, and likely in NSW. Regular review of Campylobacter laboratory results may be valuable.
Campylobacteriosis is a bacterial infection that predominantly causes gastrointestinal illness within 2–5 days (range 1–10 days) of exposure to Campylobacter. Symptoms, which include diarrhoea (frequently with bloody stools), abdominal pain, fever, nausea and vomiting, generally persist for up to 7 days. Symptoms can be prolonged or recurrent and the sequelae of infection may include rheumatological disorders, peripheral neuropathies and Guillain-Barre Syndrome.1,2 Without antibiotic treatment, infected individuals can excrete bacteria for up to 7 weeks.1
The reservoir for Campylobacter is domesticated and wild animals and the environment. Campylobacter jejuni causes the majority of human infections and most commonly occurs after ingestion of, or contact with, infected foods of animal origin, particularly poultry.1,3–5 Ingestion of as few as 500–600 Campylobacter bacteria may cause illness.3 In Australia, an estimated 75% of campylobacteriosis is thought to be foodborne.6 Cases of foodborne Campylobacter infection are usually sporadic in nature and point-source foodborne outbreaks are not commonly identified.7,8 Phenotypic methods currently used for distinguishing Campylobacter pathogens are of limited use so public health investigation or control activities occur rarely. In New South Wales (NSW), the inability to detect and control or prevent outbreaks of Campylobacter because of limitations in strain typing is the reason it is not a notifiable disease.8 DNA methods for typing strains, including multi-locus sequence typing and polymerase chain reaction, are under development.9
In all Australian jurisdictions except NSW, confirmed Campylobacter infections are required to be notified to health departments under public health legislation. Campylobacteriosis is the most commonly notified enteric condition in Australia with 17 020 notifications in 2007. Between 2004 and 2007, the overall notification rate reached 120.5 per 100 000 population.10 After campylobacteriosis, salmonellosis is the next most notified enteric disease in Australia. In 2007, there were 9546 notifications of Salmonella infections from all states and territories, with an overall notification rate of 45.4 per 100 000 population. All states and territories that notify both infections had more Campylobacter than Salmonella notifications annually between 2004 and 2007, except for the Northern Territory.11 After accounting for underreporting, it has been estimated that approximately 227 000 Campylobacter infections occur annually in Australia.12
The number and epidemiology of cases of campylobacteriosis in NSW is currently poorly described, in part because it is not notifiable. This study describes the epidemiology of laboratory-confirmed Campylobacter infection in the Hunter region of the Hunter New England Area Health Service (HNEAHS) between 2004 and 2007.
NSW is divided into eight area health services. The Hunter region refers to the south-eastern part of the HNEAHS and includes the city of Newcastle. In the Hunter region three laboratories receive the majority of stool specimens; two private laboratories that service the private health sector and one public laboratory that services the public hospital system and some private medical practices. In 2005, the estimated resident population of the Hunter region was 8.4% of NSW’s population (i.e. 573 525 people).13
Methods
The three laboratories in the Hunter region were approached to participate in the study: the public laboratory and one large private laboratory agreed to participate by providing de-identified records of people whose Campylobacter infection was detected between 1 January 2004 and 31 December 2007. For each positive sample, a laboratory identifier, the person’s date of birth, age, sex, residential postcode and specimen collection date were provided.
The data from both laboratories were merged into a single dataset, which was cleaned and checked for duplicates. A specimen was identified as a duplicate if it was collected from an individual up to 8 weeks after a previous specimen. Only infections in residents of the Hunter region were included in the analyses.
One private laboratory did not participate in the study so the total number of laboratory-confirmed Campylobacter infections diagnosed in the Hunter region for 2004–2007 was estimated. As salmonellosis is notifiable to the NSW Department of Health by all laboratories, internal quality assurance data were used to identify the notifying laboratory for each case of salmonellosis notified in the Hunter between 2004 and 2007. The proportion of salmonellosis notifications received from all laboratories in the region, and the annual median proportion of salmonellosis notifications (2004–2007 data) from the two participating laboratories were determined. The annual median proportion of salmonellosis notifications was applied to the Campylobacter diagnoses to permit an estimate of the total number of cases diagnosed from all laboratories in the area.
We assumed that the proportional distribution of Campylobacter infections and salmonellosis notifications across the three Hunter area laboratories was similar because:
-
both bacteria are detected using stool culture by local laboratories
-
salmonellosis and campylobacteriosis generally have similar transmission modes.1
We further assumed that the proportional distribution was stable throughout the study period.
Hunter region campylobacteriosis cases were described and compared to national descriptive notification data.
Results
There were 2010 isolates of Campylobacter detected by the two participating laboratories between 2004 and 2007. Of these, 357 (18%) were excluded as duplicate records and 91 (4.5%) were excluded as isolates from people who were not resident in the study area. Sixty percent of the remaining 1562 isolates were detected by the public laboratory (n = 944).
The least number of laboratory-confirmed cases of campylobacteriosis occurred in 2004 (n = 346) and the greatest in 2007 (n = 460). The pattern of a yearly increase in the number of cases in the Hunter (except 2006) was also observed in the national data (Figure 1). In the Hunter and nationally, the number of laboratory-confirmed cases peaked between November and January (Figure 2).
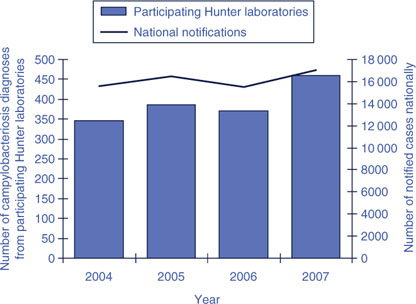
|
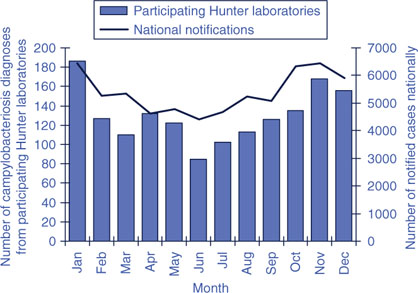
|
Between 2004 and 2007, 54% (844/1562) of laboratory-confirmed Campylobacter infections in the Hunter region were diagnosed in males. For the same period nationally, males comprised 55% of notifications. In the Hunter region, there was a predominance of males in all age groups up to 50 years, after which age case counts in males and females were similar. The median age of diagnosis for males was 31 years (inter-quartile range 16–50 years) compared with 35 years (inter-quartile range 21–58 years) in females. In children aged under 5 years in the Hunter, 99 Campylobacter infections were diagnosed in boys compared with 48 in girls. This gives a boy to girl ratio of 2.1 : 1, compared with a national notification ratio in this age group of 1.5 : 1.
The age distribution of laboratory-confirmed cases of campylobacterosis in the Hunter was similar to that of nationally notified cases (Figure 3), with a high proportion of cases in children aged under 5 years. Secondary peaks in the number of cases occurred in the 15–19-year age group in the Hunter region (10.8%) and 20–24-year age group nationally (9.6%).
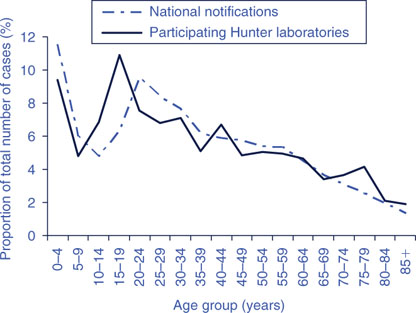
|
The local quality assurance data contained 584 salmonellosis notifications for residents of the Hunter between 2004 and 2007. The median annual proportion of Salmonella notifications processed by the participating laboratories was 48% (range 37–54%). Applying this proportion and range to the number of laboratory-confirmed Campylobacter infections identified by participating laboratories, the estimated median of the annual number of laboratory-confirmed cases of campylobacteriosis in the Hunter region was 788 (range 700–1022) between 2004 and 2007 (Table 1). The ratio of the estimated annual number of Campylobacter infections to salmonellosis notifications in the Hunter ranged between 5.3 and 6.0 : 1, with a median of 5.5 : 1 (Table 2). The lower and upper estimates of the median annual number of Campylobacter diagnoses produced ratios ranging from 4.9 to 7.1 : 1.

|
Discussion
This study estimated that in the Hunter region of NSW, campylobacteriosis is approximately five times more common than salmonellosis. The epidemiology of Campylobacter infection in the Hunter appears to be similar to other temperate areas of Australia in terms of trends in gender distribution, the number of cases occurring each year and seasonality. These similarities in demographics support the validity of this estimation process.
The ratios of annual counts of Campylobacter infection to Salmonella notifications in other Australian jurisdictions range from 5.7 : 1 in Victoria to 0.6 : 1 in the Northern Territory. If the assumptions in the Hunter are valid, the lower estimate of the Campylobacter to Salmonella infection ratio in Hunter residents is similar to that of Victorian residents.
Using Salmonella notification data to help estimate the total number of laboratory-confirmed cases of campylobacterosis is logical given the similarities in laboratory diagnostic methods and the nature of the bacteria. The use of this methodology and the assumptions made are supported by the ratio of Campylobacter to Salmonella cases in other jurisdictions, which has a limited range. We are not aware of any reasons why this should differ in the Hunter region.
Limitations to the validity of this method include the use of quality assurance data, which may have contained some duplicate Salmonella reports. There may also have been some misclassification by laboratories for the Salmonella data. As each case could have been notified by multiple laboratories, we assumed that the laboratory with the earliest notification date initially diagnosed the case. It is possible that specimens from laboratories with slower notification processes are underrepresented, although we detected no evidence of this bias in practice. Furthermore, it is unknown whether the annual variability in the proportion of Salmonella notifications received from participating laboratories was due to inaccuracies in the data, changes in notification processes or other factors.
Age-specific rates, age-standardised rates and the rate of laboratory-confirmed infection with campylobacterosis by smaller geographical area were not calculated because the population of Hunter residents serviced by the two participating laboratories is unknown.
Campylobacterosis causes a considerable morbidity and has potentially serious sequelae, so there is value in monitoring the longer-term trends in infection, particularly to determine the impact of measures implemented to reduce infection rates in humans. Measures have included initiatives in domestic and food production settings, especially in the poultry industry.5,14 Regular review of the demographic details of people in NSW with laboratory-diagnosed Campylobacter infection would provide baseline data against which the effectiveness of control measures could be determined.
Conclusions
This study provides evidence that the number of cases of laboratory-confirmed campylobacteriosis in the Hunter region is considerably greater than the number of notifications of salmonellosis. The trends in the Hunter are likely to be similar to other regions of NSW. Regular review of Campylobacter laboratory results may be valuable over time.
[1]
[2] Nachamkin I. Chronic effects of Campylobacter infection. Microbes Infect 2002; 4 399–403.
| Crossref | GoogleScholarGoogle Scholar | PubMed | (Cited 22 May 2008.)
[11]
[12] Stafford RJ, Schulter P, Kirk M, Wilson A, Unicomb L, Ashbolt R, et al. A multi-centre prospective case-control study of campylobacter infection in persons aged 5 years and older in Australia. Epidemiol Infect 2007; 135 978–88.
| Crossref | GoogleScholarGoogle Scholar | PubMed | CAS | (Cited January 2009.)
[14] Havelaar AH, Mangen MJ, de Koeijer AA, Bogaardt W, Evers EG, Jacobs-Reitsma WF, et al. Effectiveness and efficiency of controlling Campylobacter on broiler chicken meat. Risk Anal 2007; 27 831–44.
| Crossref | GoogleScholarGoogle Scholar | PubMed |



