Communicable Diseases Report, NSW, March and April 2010
Communicable Diseases BranchNSW Department of Health
NSW Public Health Bulletin 21(6) 150-155 https://doi.org/10.1071/NB10037
Published: 16 July 2010
Abstract
For updated information, including data and facts on specific diseases, visit www.health.nsw.gov.au and click on Public Health and then Infectious Diseases. The communicable diseases site is available at: http://www.health.nsw.gov.au/publichealth/infectious/index.asp.
Figure 3 and Tables 1 and 2 show reports of communicable diseases received through to the end of March and April 2010 in New South Wales (NSW).

|

|
Enteric infections
Listeriosis
Listeriosis is an infection that causes septicaemia and meningitis, usually in pregnant, immunosuppressed or frail people and is linked to eating contaminated food. Listeriosis has a long incubation period of up to 70 days.
Six cases of listeriosis were reported in NSW in March and April and one death occurred. The ages of the affected people ranged from 50 to 89 years, and three (50%) were men. Five (83%) resided in the Sydney metropolitan area. The number of notifications reported is the same as for the same period in 2009. No common links between cases were identified through local public health unit investigations.
Outbreaks of foodborne disease
Nine outbreaks of suspected foodborne disease were reported in March and April 2010 affecting 68 people. Of these nine outbreaks, six were caused by Salmonella infection. Food vehicles found to be responsible for outbreaks of salmonellosis included tartare sauce prepared with raw egg, chicken mince, fried ice cream, mayonnaise prepared with raw egg, and pork. Other foods suspected to have caused illness included fruit kebabs, sushi and other take away food.
Gastroenteritis in institutional settings
Sixty-seven outbreaks of gastroenteritis in institutions were reported in March and April 2010 affecting 1029 people. Of these, 32 occurred in child-care centres, 29 in aged-care facilities, five in hospitals and one in a residential facility. Sixty-six outbreaks appeared to have been caused by person-to-person spread of a viral illness and one was food borne.
Viral gastroenteritis tends to peak in winter months, with up to 15 outbreaks each week reported in peak months.
Gastroenteritis in the community
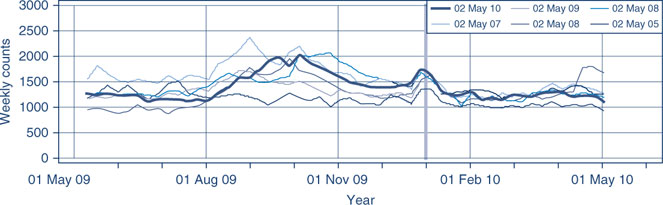
The number of patients presenting with gastrointestinal illness to emergency departments in NSW decreased slightly and remains within the usual range for this time of year (includes data from 56 NSW emergency departments) (Figure 1).
Respiratory infections
Legionnaires’ disease
Legionnaires’ disease is a form of pneumonia caused by infection acquired from environmental sources such as water droplets (Legionella pneumophila) or soil (L. longbeachae).
Seventeen cases of Legionnaires’ disease were reported in NSW in March and April 2010, including nine cases of L. longbeachae and eight cases of L. pneumophila. No common links between cases were identified through local public health unit investigations. For the same period in 2009, 11 cases of L. longbeachae and eight of L. pneumophila were reported.
Influenza
The number of patients presenting with influenza-like illness in NSW remained low (includes information from 56 NSW emergency departments) (Figure 2).
Other infections
Leprosy
A suspected case of leprosy (Hansen disease) was reported in April 2010. A man in his 30s arrived in Sydney on a commercial ship from overseas. In NSW, four cases of leprosy were reported in 2008 and there were no cases of leprosy reported in 2009.
Leprosy is a rare but curable disease. Leprosy is caused by infection with the bacterium, Mycobacterium leprae. The bacterium is very similar in appearance to M. tuberculosis. Leprosy is transmitted through close and prolonged contact with untreated cases. The people most at risk of exposure and resultant infection are people who live in household-like conditions. Casual contact is not a risk for the transmission of leprosy.
Vaccine-preventable diseases
Measles
One case of measles was reported in an unimmunised adult with links to an outbreak in New Zealand. The case had flown while infectious and passengers seated in the surrounding rows were contacted by public health staff to help contain further spread.
Six cases of measles have been reported in NSW this year (five of these had travelled overseas, and one was a contact of a known case). In 2009, seven cases were reported in NSW for the corresponding period.
Most cases of measles in NSW are seen in travellers who return with the infection from countries where measles is endemic and who are exposed to a known case. Many people who were born since 1966 and before the mid 80s are not immune to measles because they have neither acquired the measles infection nor received two doses of a measles vaccine. Measles vaccine is now routinely given to infants at 12 months and at 4 years, and this confers long-lasting immunity.
Meningococcal disease
Ten cases of meningococcal disease were reported in NSW in March and April 2010 including 3 deaths. The ages of the affected people ranged from 1 to 72 years. Six cases (60%) were male and 5 cases (50%) resided in the Sydney metropolitan area. Of the 10 cases, six were due to serogroup B, two cases were due to serogroup W135, one case in an unvaccinated adult was due to serogroup C, and for one case the serogroup was not able to be determined. For the same period in 2009, 13 cases and one death were reported (eight cases due to serogroup B, two cases due to serogroup W135, one case due to serogroup C, and for three cases the serogroup was not able to be determined).
A free vaccine is available for infants at 12 months of age. Consequently, serogroup C meningococcal disease is now mainly seen in adults and in unimmunised children. In NSW in 2009, 80% of cases of meningococcal disease (where serogroup was known) were caused by serogroup B, for which there is no vaccine.
Pertussis (whooping cough)
During March and April, 607 cases of pertussis were reported in NSW. Notifications of pertussis have declined in NSW since a peak in 2009 of 12 567 cases. In total, 1565 cases of pertussis and no deaths have been reported up to 30 April 2010. For the same period in 2009 in NSW, 6819 cases and one death were reported.
During March and April, the greatest number of notifications was in children aged 0–4 years (113, 19%) and 5–9 years of age (133, 22%). Of all cases, 269 (44%) were male and 364 cases (60%) resided in metropolitan areas.
A free vaccine is available for infants at 2, 4 and 6 months (the first dose can be given as early as 6 weeks of age) with a booster dose at 4 years (can be given from 3 years and 6 months of age). Immunisation reduces the risk of infection; however the vaccine does not give lifelong protection, and re-infection can occur. Because pertussis immunity wanes over time, many older children and adults are susceptible to infection and can be the source of new infections in infants. For a limited time, free pertussis (dTpa) vaccine is available for all new parents, grandparents and any other adults who will regularly care for infants less than 12 months of age. Free vaccine will be provided to Year 7 and Year 10 students as part of the NSW School-based Vaccination Program from 2010.
Sexually transmitted infections
Lymphogranuloma venereum
One case of lymphogranuloma venereum (LGV) was reported in metropolitan Sydney. The infection was acquired locally.
Lymphogranuloma venereum is a rare sexually transmitted chlamydial infection that spreads through unprotected vaginal, anal or oral sexual contact, especially if there is trauma to the skin or mucous membranes. Men who have sex with men, especially those who have unprotected anal sex, are at greatest risk. The bacteria that cause lymphogranuloma venereum are rare types of chlamydia, however lymphogranuloma venereum infection is a more aggressive disease than common chlamydia infections. The infection is treated with an extended course of antibiotics.