Communicable Diseases Report, NSW, July–September 2013
Communicable Diseases BranchHealth Protection NSW
NSW Public Health Bulletin 24(4) 180-187 https://doi.org/10.1071/NB13017
Published: 17 June 2014
| This will be the final edition of the Communicable Diseases Report published in the NSW Public Health Bulletin. Further reports and updated data will be available at: www.health.nsw.gov.au/Infectious/reports/Pages/default.aspx. |
Figure 1 and Table 2 show notifications of communicable diseases with onset between July and September 2013 in New South Wales (NSW).

|

|
Enteric infections
Outbreaks of suspected foodborne disease
There were nine outbreaks of foodborne or suspected foodborne disease reported by members of the public or identified through routine surveillance of Salmonella data in the third quarter of 2013, affecting at least 97 people. One outbreak was due to Campylobacter, two were due to norovirus, and the other six were due to unknown pathogens.
Only one foodborne outbreak investigation was able to provide sufficient evidence to identify the source of the infection. This outbreak occurred in a group who attended a wedding reception in July 2013. A cohort study was conducted and 30 of the 50 attendees were interviewed. Seventeen of these people reported illness and the only food with a significant association with illness was a duck liver parfait entree. One stool specimen was collected and was positive for Campylobacter. The NSW Food Authority inspected the premises and reviewed the handling of foods served. No foods were available for sampling but the chefs were advised of the proper cooking method required to render poultry livers free from bacterial pathogens with which they are known to be infected.
Another outbreak associated with a wedding at a restaurant occurred in July 2013. Thirty of the 94 guests were reported to be unwell with symptoms of vomiting, diarrhoea, fever, headache, lethargy and myalgia/arthralgia. One household reported secondary transmission. A cohort study was initiated using an online survey. Two stool specimens were collected and one was positive for norovirus. No one food item showed evidence of being the vehicle for contamination. The premises were inspected by the local council. No food safety issues or reports of gastrointestinal illness in staff were identified by council officers. This was a point source norovirus outbreak likely due to contaminated food, but the introduction mechanism of the pathogen could not be identified. This often occurs during periods of high norovirus activity. Due to the highly infectious nature of the disease, contamination of more than one source is common if a sick food handler does not have stringent hand hygiene standards.
Viral gastrointestinal disease
There were 212 reported outbreaks of (suspected) viral gastrointestinal disease in institutions in the third quarter of 2013. Of these, 106 (50%) occurred in aged-care facilities, 58 (27%) occurred in childcare centres, 40 (19%) in hospitals and eight (4%) in other facilities. The outbreaks affected a total of 3356 people.
In 57% (n = 120) of institutional outbreaks, one or more stool specimens were laboratory tested to identify a possible cause of the outbreak. Norovirus was identified in 56% (n = 67) of these outbreaks and rotavirus was identified in 4% (n = 5). In seven outbreaks, one or more pathogens were detected alongside norovirus (rotavirus in one outbreak, and Clostridium difficile in six outbreaks). Also, in two other outbreaks C. difficile was detected alongside rotavirus. In seven other outbreaks a single stool detected C. difficile (five outbreaks), Campylobacter (one outbreak) and giardia (one outbreak). These results in single stools were thought to be coincidental findings during viral gastroenteritis outbreaks. Of the 120 outbreaks where one or more stool specimens were tested, 34% (n = 41) of all results were negative for any pathogens.
There was also one gastrointestinal illness outbreak in a non-institutional setting. A Public Health Unit was notified that 26 people from a tour group of 40 reported vomiting and abdominal pain with some diarrhoea on a return flight from Santiago, Chile to Sydney, arriving on 1 August 2013. One or more people experienced some abdominal pain prior to boarding the plane with other onsets of illness from 1 to 8 hours into the flight. Illness did not last longer than 24 hours. Fifteen people were taken to emergency departments upon landing in Sydney and one sample was collected which was initially negative for all pathogens. The group had been travelling and eating together, and had staggered onsets of symptoms, so person-to-person spread of a viral pathogen was suspected. The one stool sample collected was sent for toxin testing and tested again for norovirus by polymerase chain reaction; this was negative for bacterial toxins but was positive for norovirus. The finding of norovirus is consistent with the clinical and epidemiological features of the outbreak.
Respiratory infections
Influenza
Influenza activity increased to moderate levels during the third quarter of 2013, with a peak in late August. There was evidence of co-circulation of influenza A(H1N1)pdm2009, influenza A(H3N2), and influenza B strains. The number of influenza cases notified in this quarter was much higher than for the same period in the previous year, which had an earlier start to its influenza season.
For a more detailed report on respiratory activity in NSW see: http://www.health.nsw.gov.au/PublicHealth/Infectious/influenza_reports.asp
Legionellosis
There were 15 cases of legionellosis due to Legionella pneumophila strains notified in the third quarter of 2013, an increase from the six cases notified for the same period in 2012. No clusters or common sources of infection were identified during public health follow-up. There were also 12 notifications of legionellosis due to L. longbeachae strains, compared with seven in the same period in the previous year.
Vaccine-preventable diseases
Meningococcal disease
Eighteen cases of meningococcal disease were notified in NSW in the third quarter of 2013 (four in July, nine in August and five in September), a decrease from 27 notified for the same period in 2012. The age of the cases ranged from 8 months to 92 years, with five cases aged less than 5 years. Of the 18 notifications, eight (44%) were due to serogroup B (for which there is no vaccine), five (28%) were due to serogroup W135, and four (22%) were due to serogroup Y. No serogroup was detected for the remaining notification.
Immunisation against meningococcal C disease is recommended for all children at the age of 12 months, as well as people at high risk of disease.
Measles
There were eight measles notifications in NSW in the third quarter of 2013 (two in July, one in August and five in September), a decline from the 130 reported in the same period in 2012. Two cases were acquired overseas: one in Europe (measles virus genotype D8) and the other in Bali, Indonesia. One case was linked to an overseas-acquired case and was likely infected at Melbourne airport. Five locally-acquired cases in young adults were reported in inner metropolitan Sydney; four were due to measles virus genotype D9.
Two doses of measles-containing vaccine are recommended for all children at 12 and 18 months age. All young adults planning international travel should ensure they have had two doses of measles-containing vaccine in their lifetime before they travel. Infants aged 9–12 months travelling to an area with ongoing measles transmission should also be vaccinated prior to departure.
Pertussis
There were 560 pertussis cases notified in NSW during the third quarter of 2013 (184 in July, 181 in August and 195 in September). This is less than half of the 1205 notifications for the same period in 2012, and represents the lowest number of notifications for a third quarter since 2002. Most cases were in the 5–9-year age group (n = 128), followed by the 10–14-year (n = 79) and 0–4-year age groups (n = 75).
Direct protection for young infants remains available through free vaccination for pertussis that is administered at 2, 4 and 6 months of age. The first dose can be provided as early as 6 weeks of age, with a booster dose at 3½ to 4 years. Whooping cough vaccination is strongly recommended for adults in contact with young babies too young to be vaccinated. Women planning a pregnancy or in their third trimester are encouraged to receive a whooping cough vaccine on prescription to protect their very young babies.
Sexually transmissible infections and bloodborne viruses
Chlamydia
There were 5088 chlamydia cases notified in NSW during the third quarter of 2013, similar to the number notified in the same period in 2012 (n = 5048). Fifty-four percent of the cases were female. More than half (56%) of all cases were aged 15–24 years and a further 38% were aged 25–44 years.
Gonorrhoea
There were 1060 gonorrhoea cases notified in NSW during the third quarter of 2013, a 2.5% increase compared with the same period in 2012. Just over half (52%) of gonococcal infections were in men aged 25–44 years, and a further 21% were in younger men aged 15–24 years.
Syphilis
There were 252 syphilis cases notified in NSW during the third quarter of 2013, a 10% increase compared with the same period in 2012. Eighty-six percent of the cases were men. Most cases (54%) were aged 25–44 years, followed by 45–64 years (26%).
Lymphogranuloma venereum (LGV)
There were five cases of LGV notified in NSW during the third quarter of 2013, a decrease from nine notified in the same period in 2012. All of the cases were men aged 25–44 years living in inner Sydney.
HIV
In the first 9 months of 2013, 271 people newly diagnosed with HIV infection were notified in NSW. This compares with 308 notifications for the same period in 2012, a decrease in 2013 of 12%. In 2011, there were 263 notifications during the same period. The decrease in the number of new diagnoses to date in 2013 compared to 2012 has occurred in the context of an overall small increase in testing for HIV infection, and increases in testing at publicly funded sexual health clinics and among high-risk groups, suggesting that the lower number of notifications in 2013 is not due to a reduction in testing.
Ninety-four percent of people newly diagnosed with HIV infection in the first three quarters of 2013 were male and 6% were females, a gender breakdown consistent with previous years. Most of the infections reported were in gay and homosexually active men (82%), with heterosexual contact accounting for 15% and injecting drug use for 1% of notifications. This is also similar to previous years.
A summary of HIV notification data for the third quarter of 2013 is available at: www.health.nsw.gov.au/endinghiv/Pages/tools-and-data.aspx
Arboviral infections
Ross River virus
There were 85 cases of Ross River virus infection notified in NSW in the third quarter of 2013, an increase from the same period in 2012 (n = 65). Notifications of Ross River virus infection continued to be highest in coastal regions, particularly along the north coast of NSW.
Barmah Forest virus
There were 75 cases of Barmah Forest virus infection notified in NSW in the third quarter of 2013, an increase from the same period in 2012 (n = 59). However, there continue to be concerns about false-positive laboratory reports for Barmah Forest virus and so the figures for 2013 should be interpreted with caution.
Dengue virus
There were 82 cases of dengue virus infection notified in NSW in the third quarter of 2013, an increase from the same period in 2012 (n = 57). All cases were overseas-acquired infections; 43% of all cases are believed to have acquired the infection in Indonesia, and 21% of all cases are believed to have acquired the infection in Thailand.
NSW Denominator Data Project
Notifications of positive laboratory results for notifiable conditions provide information about the number of new cases of disease. Data on the level of testing is useful to indicate whether an apparent increase in notifications may be due to increased testing.
The NSW Denominator Data Project commenced in January 2012 to collect the total number of tests performed per month (the denominator data) for 10 selected notifiable conditions for which the testing rate might impact the notification rate. Data provided each month from 14 public and private laboratories in NSW is collated to give monthly aggregated data per condition. No demographic information is provided.
The positivity rate for all conditions from January 2012 to September 2013 ranged from 0.07% (shigellosis) to 5.52% (chlamydia) (Table 1). Notifications for chlamydia and gonorrhoea were well correlated with testing, while the incidence of enteric conditions suggests that seasonal factors rather than testing patterns influence notification rates.
Trends in testing and notification are best identified by comparing similar periods to avoid seasonal variation. For the third quarter (July–September 2013), the positivity rates overall were similar to the same period in 2012, and ranged from 0.07% (shigellosis) to 5.24% (chlamydia). Exceptions for this period were Ross River virus (up to 2.55% from 1.87% in 2012) and pertussis (down to 1.56% from 2.66% in 2012). Pertussis has shown a generally downward trend in both notifications and positivity since 2012.
Seeing spots: does a poster displayed at an airport raise awareness of measles among incoming travellers?
Johanne E. CochraneA,B,C, Paula J. SpokesA, and Jeremy M. McAnultyA
AHealth Protection NSW
BPublic Health Unit, Sydney and South Western Sydney Local Health Districts
CCorresponding author. Email: Johanne.Cochrane@sswahs.nsw.gov.au
Measles vaccination has been available in Australia since 1969, but some groups remain at risk through inadequate vaccination. There were 90 measles notifications in New South Wales (NSW) in 2011, of which 10% were imported from overseas; the remainder were either linked to these cases or locally acquired. The number of cases recorded was the highest since 1998, the year of the Australian Measles Control Campaign.1 Lack of awareness of measles among both the public and clinicians can lead to delayed presentation and diagnosis, increasing the transmission risk.2 We sought to evaluate whether the awareness of incoming travellers of the risk of measles was increased by using a poster campaign at Sydney International Airport.
Methods
A poster (0.57 m × 0.97 m) was placed in a rotating display (as one of three different posters each displayed for 10 seconds at a time) for 4 weeks in October 2011 above the baggage collection carousels at Sydney International Airport. All international arrivals could view the poster, including travellers returning from New Zealand, which was experiencing measles outbreaks at the time.3 The poster was eye-catching (brightly coloured, showing a human figure covered with red spots) with six key messages about measles, including: alerting the public to the presence of the disease and the serious risk to health posed by measles, risk to travellers, typical symptoms, advice to phone ahead before visiting a doctor, and to tell your doctor of your overseas travel. The cost of displaying the poster for 4 weeks was approximately $12 000.
Two interviewers conducted a survey of travellers at the public arrivals gate for 2 hours on a mid-week morning, using a brief questionnaire to assess recall of the poster. Travellers were chosen by alternating genders, at the two international arrival gates, until a sufficient sample was collected. Travellers were asked if they saw any health messages, and were prompted once about the measles poster. Those who recalled the poster were asked if they remembered any of the messages. The interviewers recorded the gender and approximate age of the interviewees (18–30, 31–65 and over 65 years). People with limited spoken English were excluded.
Results
Ninety-six people were approached; 83 (86%) agreed and were eligible to participate (Table A).

|
Nine interviewees (11%) recalled seeing the poster; five (6%) could recall any messages, and the maximum number of messages recalled was two out of six. Fifty percent of those who recalled seeing the poster recalled the poster title, ‘measles is about’. No-one recalled the advice to phone ahead if developing symptoms, important in minimising spread to others. One person recalled a message not on the poster (‘no spitting’). No interviewees aged over 65 years recalled the poster.
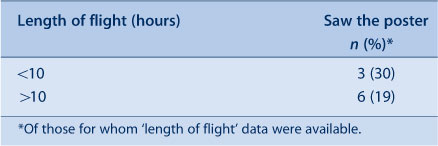
Likelihood of seeing the poster was increased with shorter flights but this difference was not statistically significant (RR 1.5 (CI 0.5–4.7)) (Table B). The likelihood of having seen the poster did not differ by gender (M:F) RR 1.1 (CI 0.6–2.0).
|
Discussion
Posters are used to provide health alerts as well as health information. Previous evaluations have shown that posters have varying success in conveying health messages.4–6 The setting and length of time between seeing the poster and acting on the messages, as well as the length of time the poster is displayed, appear to affect recall and behaviour change. Posters have been less successful than other media in multimedia campaigns.7–9
Our survey found that a low percentage of people remembered a poster about measles located above the baggage collection carousels at Sydney International Airport, even shortly after exposure. It is possible that the distraction of identifying and collecting luggage, and fatigue, reduced receptivity to the information, as well as the rotation of the poster with two other unrelated posters. Limitations of the survey method include using a convenience sample: for instance, recall and age of arrivals could have been different at other times of the day, or on other days of the week. The questionnaire was deliberately brief to increase participation but this limited the information collected.
Conclusion
Posters displaying health alerts to incoming airline passengers did not appear to be an effective method for increasing awareness of the risk of measles.
Acknowledgment
We thank Stephanie Zbik, NSW Health, for assisting with the survey.
References
[1] Centre for Health Protection Year in review: health protection in NSW, 2011. N S W Public Health Bull 2012; 23 129–41.| 23043745PubMed |
[2] Weston KM, Dwyer DE, Ratnamohan M, McPhie K, Chan SW, Branley JM, et al. Nosocomial and community transmission of measles virus genotype D8 imported by a returning traveller from Nepal. Commun Dis Intell 2006; 30 358–65.
[3] The Institute of Environmental Science and Research Ltd. Notifiable and other Diseases in New Zealand: Annual Report 2011. Porirua, New Zealand; pp. 38–40. Available at: https://surv.esr.cri.nz/PDF_surveillance/AnnualRpt/AnnualSurv/2011/2011AnnualSurvRpt.pdf (Cited 10 January 2014).
[4] Soler RE, Leeks KD, Buchanan LR, Brownson RC, Heath GW, Hopkins DH, et al. Point-of-decision prompts to increase stair use. A systematic review update. Am J Prev Med 2010; 38 S292–300.
| Point-of-decision prompts to increase stair use. A systematic review update.Crossref | GoogleScholarGoogle Scholar | 20117614PubMed |
[5] Ward K, Hawthorne K. Do patients read health promotion posters in the waiting room? A study in one general practice. Br J Gen Pract 1994; 44 583–5.
| 1:STN:280:DyaK2M3mslGksw%3D%3D&md5=1a5331d6fc647f7aaa82e6c3293d6051CAS | 7748670PubMed |
[6] Wicke DM, Lorge RE, Coppin RJ, Jones KP. The effectiveness of waiting room notice-boards as a vehicle for health education. Fam Pract 1994; 11 292–5.
| The effectiveness of waiting room notice-boards as a vehicle for health education.Crossref | GoogleScholarGoogle Scholar | 1:STN:280:DyaK2M7ksFynsQ%3D%3D&md5=857fff0e8205567e703efa21ef443407CAS | 7843520PubMed |
[7] John-Leader F, Van Beurden E, Barnett L, Hughes K, Newman B, Sternberg J, et al. Multimedia campaign on a shoestring: promoting ‘Stay Active – Stay Independent' among seniors. Health Promot J Austr 2008; 19 22–8.
| 18481928PubMed |
[8] Pless IB, Hagel B, Patel H, Leduc D, Magdalinos H. Preventing product-related injuries: a randomized controlled trial of poster alerts. Can J Public Health 2007; 98 271–5.
| 17896734PubMed |
[9] Oakman T, Byles-Drage H, Pope R, Pritchard J. Beat the Heat: don't forget your drink – a brief public education program. Aust N Z J Public Health 2010; 34 346–50.
| Beat the Heat: don't forget your drink – a brief public education program.Crossref | GoogleScholarGoogle Scholar | 20649772PubMed |


