Typhoid fever, NSW, 2005–2011
Praveena Gunaratnam A C D , Sean Tobin B , Holly Seale C and Jennie Musto BA NSW Public Health Officer Training Program, NSW Ministry of Health
B Health Protection NSW
C School of Community and Public Health Medicine, The University of New South Wales
D Corresponding author. Email: pguna@doh.health.nsw.gov.au
NSW Public Health Bulletin 24(2) 87-91 https://doi.org/10.1071/NB12125
Published: 7 November 2013
Abstract
Aim: To examine trends in the incidence of typhoid fever in NSW to inform the development of prevention strategies. Methods: Typhoid fever case notification data for the period 2005–2011 were extracted from the NSW Notifiable Conditions Information Management System. Population incidence rates were calculated and analysed by demographic variables. Results: There were 250 case notifications of typhoid fever in NSW from 2005 to 2011, of which 240 are likely to have been acquired overseas. Case notifications remained relatively stable over the review period with the highest rates in Western Sydney Local Health District (10.9 per 100 000 population). Two-thirds (66.4%) of all case notifications are likely to have been acquired in South Asia, and about half of overseas-acquired case notifications were most likely to have been associated with travel to visit friends and relatives. Hospitalisation was required for 79.6% of cases where hospitalisation status was known. Prior typhoid vaccination was reported in 7% of cases in 2010 and 2011 where vaccination status was known. Conclusion: While typhoid fever rates remain low in NSW, case notifications of this preventable infection continue to be reported, particularly in travellers visiting friends and relatives in South Asia. Further research to better understand barriers to the use of preventive measures may be useful in targeting typhoid fever prevention messages in high-risk groups, particularly South Asian communities in NSW.
Typhoid fever is a systemic bacterial infection caused by the Salmonella enterica subsp. enterica serovar Typhi (commonly S. Typhi) and is primarily spread by the faecal-oral-route.1 Typhoid fever typically presents as sustained fever, abdominal pain and headaches, with complications such as gastrointestinal bleeding occurring in 10–20% of untreated patients. The case fatality rate is less than 1% with appropriate antibiotic treatment.2 Up to 10% of untreated patients continue to excrete S. Typhi for 3 months after symptoms resolve, and 1–4% of untreated patients continue to excrete S. Typhi for over 12 months and become chronic carriers.1 Ongoing S. Typhi excretion is an important public health issue, particularly if the person works in an occupation associated with higher risk of transmission, such as food preparation.
S. Typhi causes a considerable burden of disease worldwide, particularly in low and middle income countries. The global annual incidence of typhoid fever in 2004 was estimated at 22 million cases, with 220 000 deaths.3 The incidence of typhoid fever in developed countries has steadily declined over the past 50 years due to improved water quality and sanitation, with annual incidence rates of typhoid fever ranging from 0.13 to 1.2 cases per 100 000 population and almost all case notifications associated with international travel.4 In Australia in 2011 there were 135 typhoid fever case notifications reported, equivalent to 0.6 per 100 000 population.5
People who travel to typhoid-endemic countries – such as India, Sri Lanka, Pakistan, Bangladesh and Nepal – to visit friends and relatives (VFR) have been shown to be at particular risk of acquiring typhoid fever infection.6–8 These travellers are more likely to travel to rural areas that have poor sanitation, to stay for longer periods of time, and are less likely to adopt safe food and water practices.4 A UK study considering both typhoid and paratyphoid fever found 88% of travel-associated case notifications involved VFR travel, and of these 89% were travellers of Indian, Pakistani or Bangladeshi ethnicity.9
Food and water precautions (such as not eating uncooked foods and only drinking boiled and bottled water) and personal hygiene (such as hand washing) are essential to prevent typhoid fever.2,10 The Australian Technical Advisory Group on Immunisation also recommends vaccination for all people aged over 2 years who are travelling to an endemic region.11
International travel by New South Wales (NSW) residents is increasing. In 2011, there were 2.7 million short-term departures, an increase of 50% since 2005. VFR travel was the reason for almost one-quarter (23.5%) of these departures.12 In this context, the present study examined trends in the incidence of typhoid fever in NSW from 2005 to 2011, and the importance of country of birth, place of travel, and vaccination status, in order to develop appropriately targeted prevention strategies.
Methods
Under the NSW Public Health Act 2010, hospitals and laboratories must notify cases of typhoid fever to NSW Health. Public Health Units investigate all case notifications of typhoid to: collect relevant risk information, identify the likely source of infection, and instigate control measures if necessary. Laboratory confirmation through isolation of S. Typhi in blood, urine, faeces or other clinical specimens is required before a case notification can be classified as typhoid.13 Confirmed case notifications are entered onto the NSW Notifiable Conditions Information Management System (NCIMS). Data describing typhoid fever cases were extracted from NCIMS for the period 1 January 2005–31 December 2011, and cleaned and analysed using Microsoft Excel 2007. Missing data fields were reviewed, and fields related to travel and likely country of disease acquisition were completed by cross-referencing with free text information recorded in the ‘Notes’ field where available. Where travel to more than one country was recorded, country of likely disease acquisition was the typhoid-endemic country in which the case spent the most time.
A case was classified as overseas acquired where recent travel was reported prior to onset of illness, noting the incubation period for typhoid fever can be longer than 60 days.13 These case notifications were assigned to one of six categories:
-
‘Confirmed VFR travel’: the record clearly indicated the case travelled to the country of likely disease acquisition to visit friends and relatives.
-
‘Probable VFR travel’: the case’s country of birth was the same as the country of likely disease acquisition.
-
‘Possible VFR travel’: the case’s name had plausible associations to the country of likely disease acquisition, though the country of birth was different or unknown.
-
‘Non-VFR travel’: the record clearly indicated the case travelled to the country of likely disease acquisition for a purpose other than visiting friends and relatives.
-
‘Immigrant’: the record clearly indicated the case recently immigrated to Australia from the country of likely disease acquisition.
-
‘Unknown’: the reason for recent travel was unknown.
Data describing country of birth and country of disease acquisition were grouped into regions using the World Bank classification system, with Australia and New Zealand extracted as a separate category.14 Annual notification rates by age group and Local Health District (LHD) were calculated using the year-end estimated population for LHDs and NSW as a whole, obtained from the 2006 Australian Census of Population and Housing and downloaded from the NSW Health Outcomes Information Statistical Toolkit (HOIST).
Descriptive analyses were performed for demographic variables (age, sex, country of birth), recent travel, country of likely disease acquisition, vaccination status and reasons for not being vaccinated, and hospitalisation status. Vaccination data were only available for 2010 and 2011, as vaccination status was not systematically recorded in the database before this.
Results
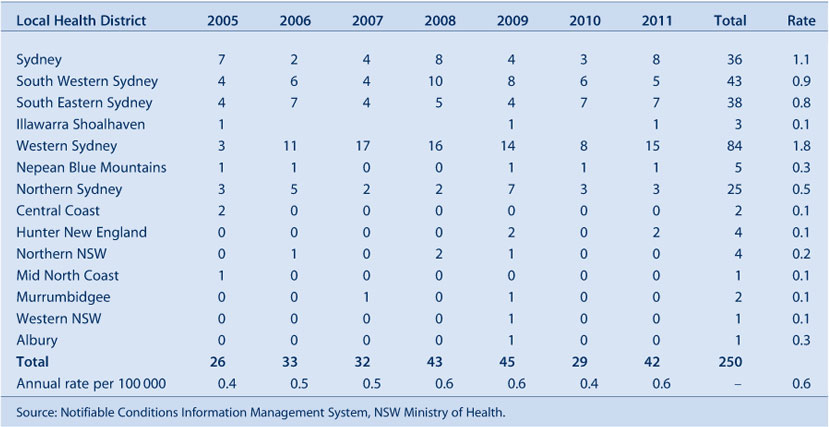
Annual case notifications and rates per 100 000 population by LHD are presented in Table 1. In NSW, there were 250 notifications of typhoid fever from 2005 to 2011. Annual rates remained stable, ranging from 0.4 per 100 000 population to 0.6 per 100 000 population. The highest numbers and rates of notifications were found in metropolitan Sydney, particularly in Western Sydney LHD.
|
The age distribution of cases is presented in Table 2. The average age of cases remained relatively stable over the period, ranging from 24 years in 2007 to 30 years in 2009. Three age groups (0–4 years, 20–24 years and 25–29 years) accounted for almost half (47.2%) of the total number of cases. Males accounted for 53.6% of notifications overall.

|
Two hundred and forty cases had recently travelled; all of these people were assumed to have acquired their infection overseas. Ten cases were locally acquired; six of these were contacts of another known or possible case, three were chronic carriers, and one worked in a laboratory and could have been exposed to the S. Typhi isolate at work. For the six cases who were contacts, it was not clear from their record if their contact was with a case who acquired the disease overseas or not.
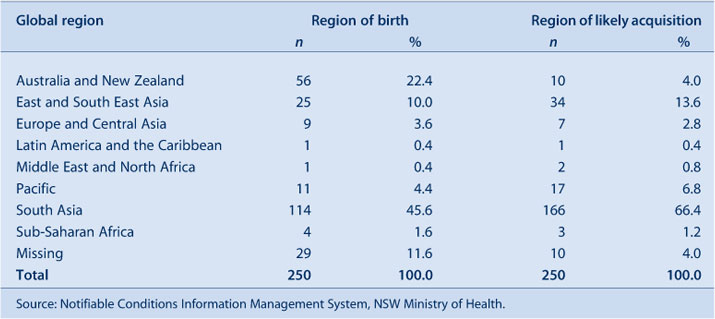
Information describing country of birth was available for 221 (88.4%) typhoid fever cases (Table 3). Overall, 45.6% of cases were born in South Asia; this figure increases to 47.1% when locally-acquired case notifications are excluded. The country of likely disease acquisition was available for 230 of the 240 overseas-acquired case notifications (Table 3). Two-thirds (66.4%) of all typhoid fever case notifications were believed to have been acquired in South Asia: India (47.5%), Bangladesh (12.9%), and Pakistan (6.3%). Travel to Samoa was reported by 5.0% of cases.
|
Reason for travel could be classified for 204 (85.0%) overseas-acquired case notifications. Only one case (0.4%) was confirmed VFR travel, 116 (48.3%) were probable VFR travel, 68 (28.3%) were possible VFR travel and 11 (4.6%) were recent immigrants from typhoid-endemic countries. The other eight cases (3.3%) were non-VFR travel. Almost all cases in the 0–4-year age group could be classified as probable (n = 7, 24.1%) or possible (n = 19, 65.5%) VFR travel.
Hospitalisation status was recorded for 90.4% (n = 226) of all typhoid fever cases, with 79.6% (n = 199) of all cases requiring hospitalisation. No deaths were recorded. Vaccination status was reported for 55 (77.5%) of the 71 cases in 2010 and 2011. For five cases (7.0%), either the patient or their general practitioner reported that the patient had been vaccinated for typhoid; 50 cases (70.4%) reported they had not been vaccinated. Reasons for not being vaccinated were recorded for 30 (60%) of the 50 unvaccinated cases. The most common reasons cited were: choosing not to (n = 10), not considering (n = 9) or not knowing about vaccination (n = 5), and not believing there would be a risk staying with friends and family (n = 2).
Discussion
Consistent with estimates in other high income countries,4,10 the incidence rate of typhoid fever in NSW is low and remained stable from 2005 to 2011 despite increased international travel during this period. Typhoid fever has serious implications, as evidenced by the high rates of hospitalisation amongst cases. Despite moderate vaccine efficacy,15 some of these case notifications could have been prevented through vaccination, as only 7% of typhoid cases in 2010 and 2011 reported receiving vaccination prior to travel.
Also similar to previous studies,9,10 this review shows typhoid cases in NSW are strongly associated with travel to the South Asia region. In about half of cases, the most likely reason for travel is visiting friends and relatives. This group has been shown to face particular barriers in accessing pre-travel advice and taking precautions, including being unaware of the potential risks to their health in returning to their country of origin, language constraints, and financial considerations in accessing health care in Australia.16 In particular, the associated out of pocket costs and short duration of immunity (3 years) may be disincentives to typhoid vaccination among at-risk groups.11 Estimates of typhoid vaccine uptake amongst Australian travellers are not available, but studies from other developed countries also suggest uptake rates are low, especially among VFR travellers.17
The highest rates of typhoid fever were found in metropolitan Sydney LHDs, particularly Western Sydney LHD. Typhoid fever cases in this LHD have been analysed in greater depth in a separate review.18 The higher rates in metropolitan LHDs most likely reflect the proportion of the population in these areas with links to typhoid-endemic countries. Targeted approaches to promoting typhoid fever prevention could be trialled and evaluated with these communities. Measures could include health professionals providing advice during routine health checks and working with multicultural health services to develop culturally and linguistically appropriate resources. Recent research indicates that community-based initiatives which use multicultural media and events can be an effective way to provide health education messages.19
Young adults appear to be at particular risk, which may reflect higher rates of international travel among this group.20 The relatively large number of cases in children aged under 5 years – most of whom have VFR as a probable or possible reason for travel – underscores the need to promote typhoid fever prevention to parents.
Limitations to this study include the amount of missing data on variables such as country of birth and vaccination status, reliance on self or general practitioner reporting of vaccination status, and lack of definitive information on the reason for travel. Classification as a ‘possible’ VFR case based on last name was particularly subjective. Severe cases are more likely to be identified and investigated, which may have resulted in an overestimation of the hospitalisation rate in this group.
Conclusion
This study confirms that typhoid fever is an important public health problem, particularly for people of South Asian ethnicity who may be returning to the region to visit friends and relatives. Further research, including surveys of high-risk communities to better understand barriers to seeking pre-travel advice, and in the use of preventive measures, may be useful to inform targeted prevention strategies and further reduce the incidence of typhoid fever in NSW. Increasing adherence to food and water precautions and personal hygiene measures would have the added benefit of reducing the risk of other predominantly travel-related enteric infections such as paratyphoid fever, hepatitis A, hepatitis E, and shigellosis.
Acknowledgments
This work was completed while Praveena Gunaratnam was a trainee on the NSW Public Health Officer Training Program, funded by the NSW Ministry of Health. She undertook this work while based at the Communicable Diseases Branch, Health Protection NSW.
Thanks to Vicky Sheppeard (Director, Communicable Diseases Branch, Health Protection NSW) and Jeremy McAnulty (Director, Health Protection NSW) for offering comments on the paper.
References
[1] Heymann DL, ed. Control of Communicable Diseases Manual. 19th ed. Washington: American Public Health Association; 2008.[2] Mandell G, Bennett J, Dolin R, eds. Mandell, Douglas and Bennett’s Principles and Practice of Infectious Diseases. 7th ed. London: Churchill Livingstone; 2010.
[3] Crump JA, Luby SP, Mintz ED. The global burden of typhoid fever. Bull World Health Organ 2004; 82 346–53.
| 15298225PubMed |
[4] Connor BA, Schwartz E. Typhoid and paratyphoid fever in travellers. Lancet Infect Dis 2005; 5 623–8.
| Typhoid and paratyphoid fever in travellers.Crossref | GoogleScholarGoogle Scholar | 16183516PubMed |
[5] Australian Government Department of Health and Ageing. National Notifiable Diseases Surveillance System. Typhoid Notifications. Available at: http://www9.health.gov.au/cda/Source/CDA-index.cfm (Cited 3 May 2012).
[6] Kidenya V, Ferson M. Typhoid and paratyphoid fever in south-eastern Sydney, 1992–1997. Commun Dis Intell 2000; 24 233–6.
| 1:STN:280:DC%2BD3cvmvVGksg%3D%3D&md5=8a0cb1dd2175ae11c066d9ccaa5f5375CAS | 11022389PubMed |
[7] Wilson ME, Weld LH, Boogild A, Keystone JS, Kain KC, von Sonnenburg F, et al. Fever in returned travellers: results from the GeoSentinel Surveillance Network. Clin Infect Dis 2007; 44 1560–8.
| Fever in returned travellers: results from the GeoSentinel Surveillance Network.Crossref | GoogleScholarGoogle Scholar | 17516399PubMed |
[8] Basnyat B, Maskey AP, Zimmerman MD, Murdoch DR. Enteric (typhoid) fever in travelers. Clin Infect Dis 2005; 41 1467–72.
| Enteric (typhoid) fever in travelers.Crossref | GoogleScholarGoogle Scholar | 16231259PubMed |
[9] UK Health Protection Agency. Foreign travel-associated illness – a focus on those visiting friends and relatives. 2008 report. Available at: http://www.hpa.org.uk/Publications/InfectiousDiseases/TravelHealth/0812Foreigntravelassociatedillness/ (Cited 3 May 2012).
[10] Crump JA, Mintz ED. Global trends in typhoid and paratyphoid fever. Clin Infect Dis 2010; 50 241–6.
| Global trends in typhoid and paratyphoid fever.Crossref | GoogleScholarGoogle Scholar | 20014951PubMed |
[11] Australian Government Department of Health and Ageing and National Health and Medical Research Council. The Australian Immunisation Handbook. 9th edition. Available at: http://www.health.gov.au/internet/immunise/publishing.nsf/Content/Handbook-home (Cited 3 May 2012).
[12] Australian Bureau of Statistics. Overseas Arrivals and Departures – Customised Data Report. 12 March 2012.
[13] NSW Health. Typhoid response protocol for NSW Public Health Units. Sydney; 2004.
[14] World Bank Country and Lending Groups. Available at: http://data.worldbank.org/about/country-classifications/country-and-lending-groups (Cited 3 May 2012).
[15] Whitaker JA, Franco-Paredes C, del Rio C, Edupuganti S. Rethinking typhoid fever vaccines: implications for travelers and people living in highly endemic areas. J Travel Med 2009; 16 46–52.
| Rethinking typhoid fever vaccines: implications for travelers and people living in highly endemic areas.Crossref | GoogleScholarGoogle Scholar | 19192128PubMed |
[16] Leder K, Tong S, Weld L, Kain KC, Wilder-Smith A, von Sonneburg F, et al. Illness in travellers visiting friends and relatives: a review of the GeoSentinel surveillance network. Clin Infect Dis 2006; 43 1185–93.
| Illness in travellers visiting friends and relatives: a review of the GeoSentinel surveillance network.Crossref | GoogleScholarGoogle Scholar | 17029140PubMed |
[17] Angell SY, Cetron MS. Health disparities among travelers visiting friends and relatives abroad. Ann Intern Med 2005; 142 67–72.
| Health disparities among travelers visiting friends and relatives abroad.Crossref | GoogleScholarGoogle Scholar | 15630110PubMed |
[18] Blackstock SJ, Sheppeard VK, Paterson JM, Ralph AP. Typhoid and paratyphoid fever in Western Sydney Local Health District, NSW, January–June 2011. N S W Public Health Bull 2012; 23 148–52.
| Typhoid and paratyphoid fever in Western Sydney Local Health District, NSW, January–June 2011.Crossref | GoogleScholarGoogle Scholar | 23043747PubMed |
[19] Leder K, Lau S, Leggat P. Innovative community-based initiatives to engage VFR travelers. Travel Med Infect Dis 2011; 9 258–61.
| Innovative community-based initiatives to engage VFR travelers.Crossref | GoogleScholarGoogle Scholar | 1:STN:280:DC%2BC3MbivVSmug%3D%3D&md5=91e2bd4131b4d1871c2c0415721d987bCAS | 21968465PubMed |
[20] Australian Bureau of Statistics. Overseas Arrivals and Departures, Australia, Dec 2011. Cat No 3401.0.

