Year in review: health protection in NSW, 2010
Centre for Health ProtectionNSW Department of Health
NSW Public Health Bulletin 22(8) 137-148 https://doi.org/10.1071/NB11020
Published: 20 September 2011
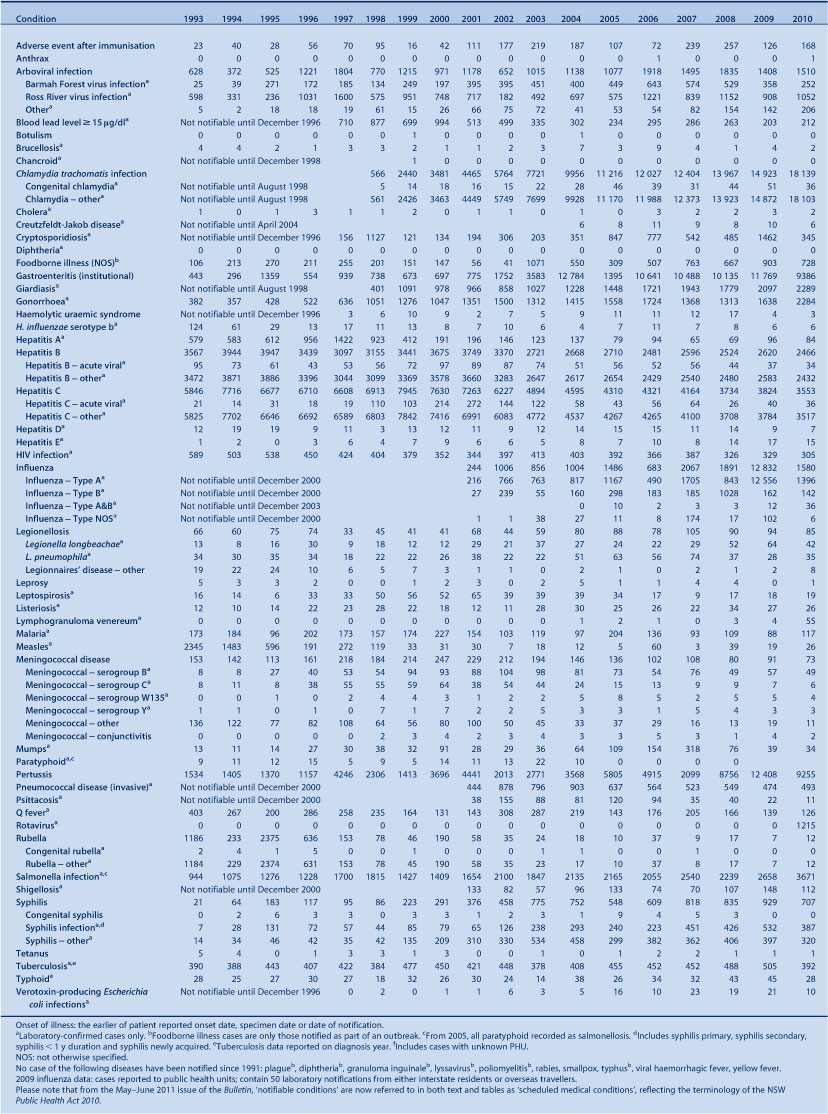
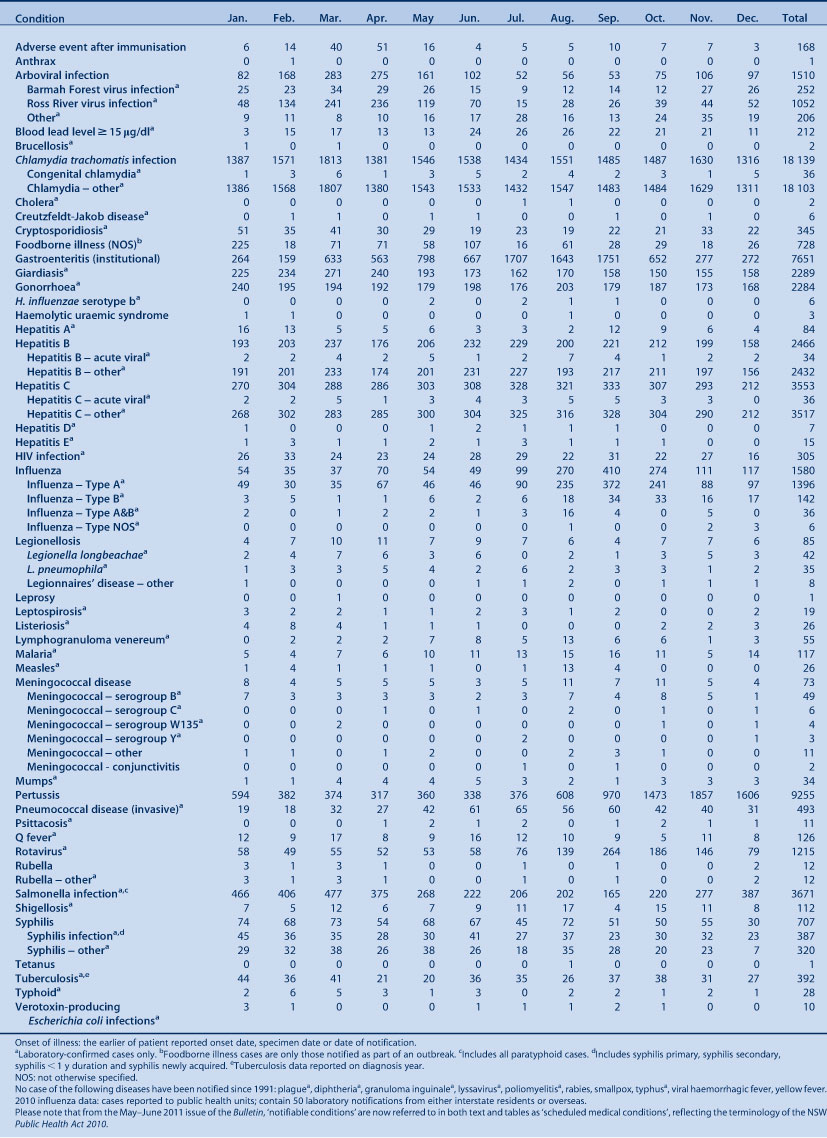
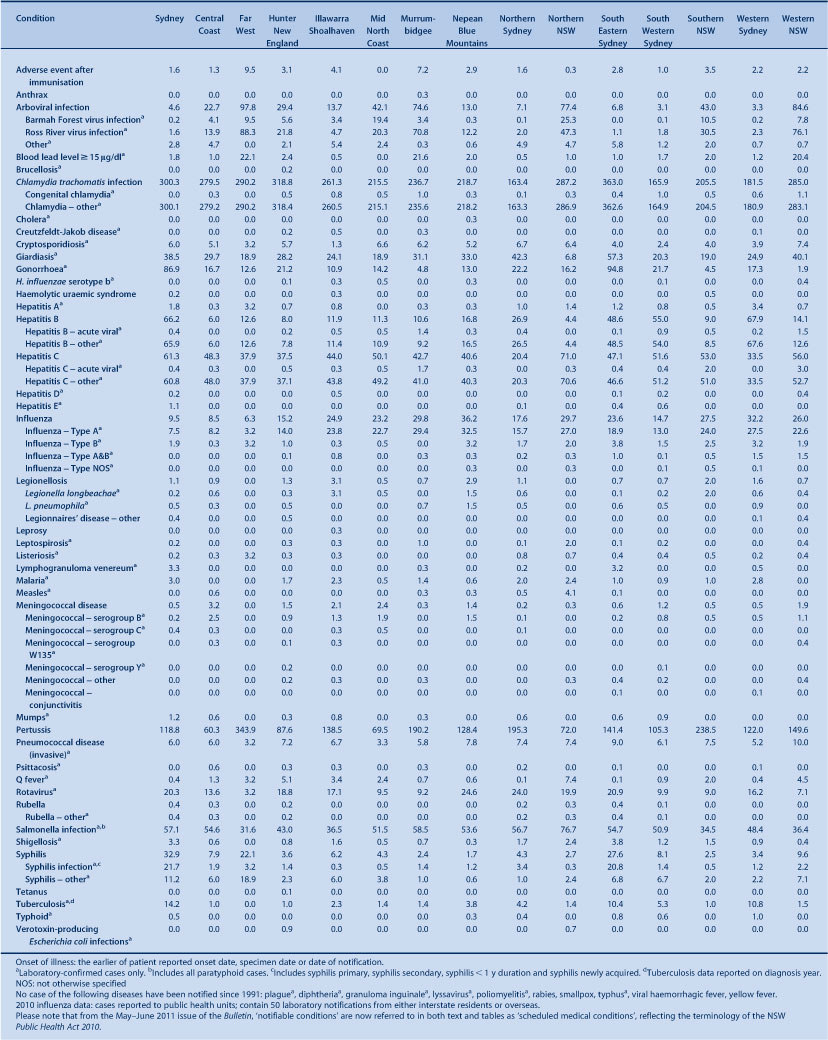
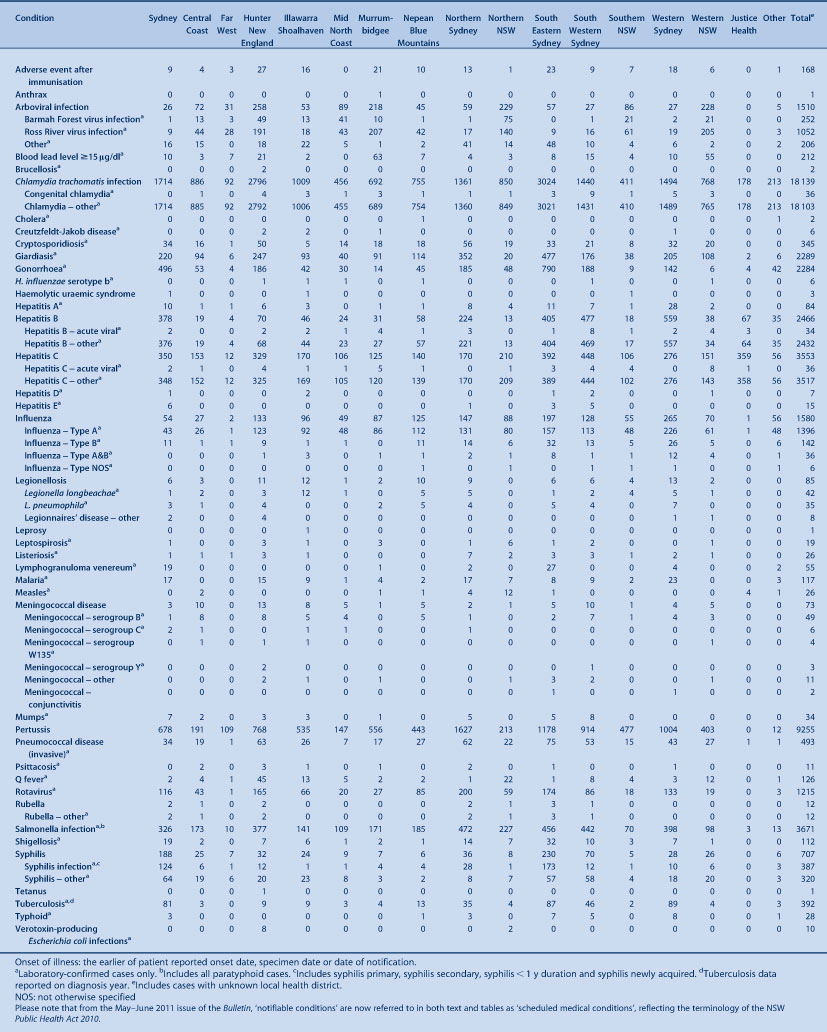
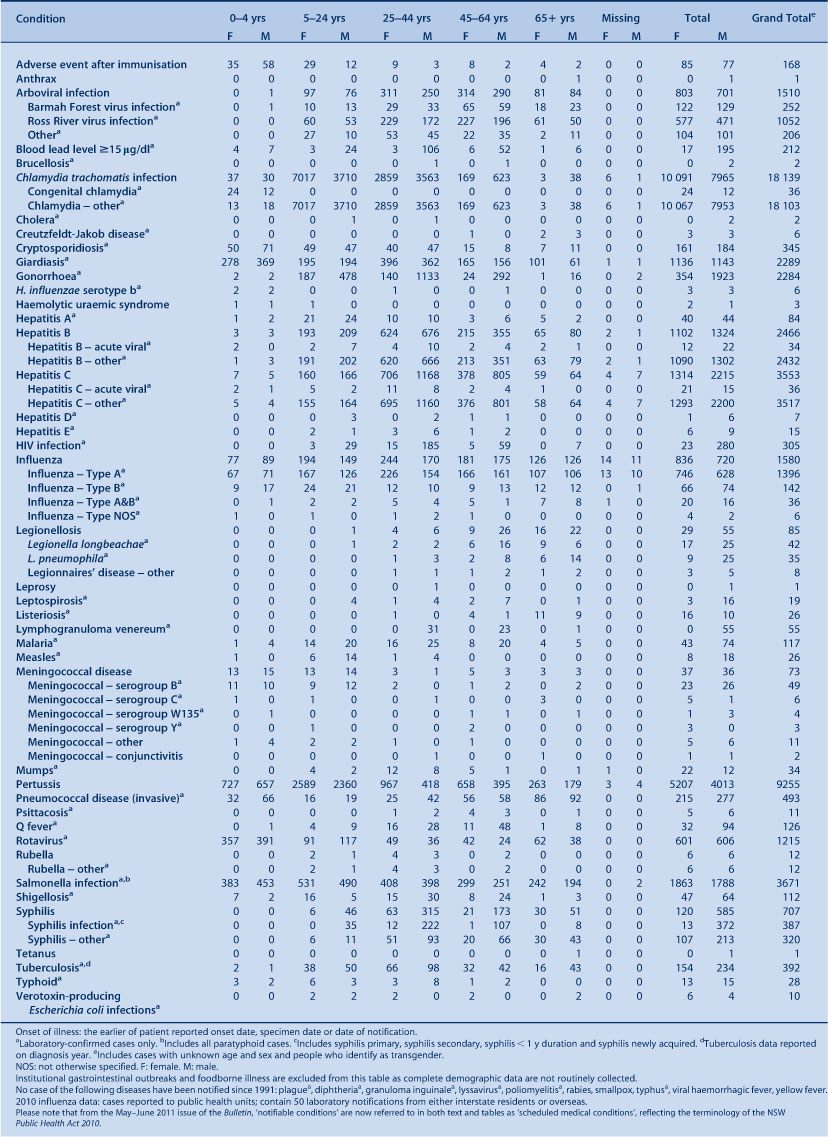
The prevention and control of communicable and environmental threats to health is the work of health protection services around the world. This year we expand the usual year in review of communicable disease surveillance in NSW to highlight some of the work of NSW health protection services in 2010. The annual review of notifications of communicable diseases in NSW is embedded within this report; for detail on surveillance data, refer to Tables 1–5, which show disease-specific data on notifiable conditions* reported by: year of onset of illness; month of onset of illness; local health district; and age group and sex.
|
|
|
|
|
The Centre for Health Protection aims to reduce the threats to health and the burden of illness posed by communicable diseases and the environment in New South Wales (NSW). It achieves this through the development and application of legislation, regulations, policies and guidelines, through allocation of resources, monitoring of program performance (in non-government, community, education, ambulatory and inpatient settings) and collaboration with public health units, local health districts and other agencies. The Centre has three branches which are responsible for these activities:
-
The Environmental Health Branch facilitates the prevention, assessment and management of environmental factors which can adversely affect human health.
-
The AIDS and Infectious Diseases Branch is responsible for policy and program management activities that seek to prevent and reduce morbidity associated with bloodborne, sexually transmissible and vaccine-preventable diseases.
-
The Communicable Diseases Branch conducts surveillance for notifiable communicable diseases and develops control measures to help prevent their spread.
Vaccine-preventable diseases
Notification data
There were 9900 notifications of vaccine-preventable disease reported in NSW in 2010. This represents a 45% increase compared with the previous 5-year average annual disease count. Highlights in 2010 included:
-
A continued high level of pertussis activity with 9255 notifications, compared with 12 408 in 2009. The number of notifications was highest in children aged 5–9 years (2719 notifications) and 10–14 years (1606 notifications).
-
A continued long-term decline in the number of notifications of meningococcal disease over the past 10 years (73 notifications compared with 91 in 2009). The greatest decline was in notifications of meningococcal disease due to serogroup C disease, with six cases notified in 2010. Free immunisation against meningococcal disease due to serogroup C meningococcal disease commenced in 2003.
-
A small rise in measles notifications with 26 cases notified compared with 19 in 2009. Of the notifications in 2010, 15 were associated with an outbreak on the NSW North Coast (three from correctional facilities) linked to an unimmunised person who acquired the infection overseas.
Prevention activities
Immunisation rates for children and adolescents have improved in some age groups in recent years in NSW, however further work is required to improve coverage rates for 12-month old Aboriginal children.
According to the Australian Childhood Immunisation Register, in 2010 full immunisation was recorded for:
-
91.4% of 12-month old children, a decrease of 0.7% from 2009a
-
92.4% of 2-year old children, a decrease of 0.1% from 2009b
-
87.6% of 5-year old children, an increase of 4.3% from 2009.c
In 2010, full immunisation coverage in Aboriginal children was recorded for:
-
86.6% of 12-month old Aboriginal children, a decrease of 0.4% from 2009a
-
91.9% of 2-year old Aboriginal children, an increase of 1.4% from 2009b
-
82.3% of 5-year old Aboriginal children, an increase of 2.2% from 2009.c
In 2010, the NSW School-Based Vaccination Program vaccinated:
-
70% of Year 7 and 62% of Year 10 children with the diphtheria-tetanus-pertussis vaccine booster
-
77% of Year 7 girls with at least one dose and 67% of Year 7 girls for three doses of human papillomavirus vaccine
-
63% of Year 7 children with at least one dose and 57% of children with two doses of hepatitis B vaccine (hepatitis B vaccination is only offered to children who have not previously received a full course)
-
34% of Year 7 children with varicella vaccine (varicella vaccination is only offered to children without history of infection or vaccination).
These data do not include children who received these free vaccines from general practitioners (GPs) or other immunisation providers.
In response to increased pertussis and measles notifications, the following initiatives continued in 2010:
-
Information provided for new parents of babies registered with Medicare stressing the importance of vaccinating their baby on time and ensuring other household members are up to date with their pertussis vaccinations.
-
Free pertussis vaccine provided for new parents, grandparents and other adults who regularly care for infants less than 12 months of age to protect infants too young to be vaccinated (233 565 doses distributed to GPs in 2010).
-
Free measles-mumps-rubella vaccine provided to contacts of people with measles to prevent further transmission in the community.
-
Communication with health care workers and the public through the media, the NSW Health website and specific fax streams.
Bloodborne viruses
Notification data
There was an overall slight decrease in bloodborne virus notifications in NSW in 2010. Highlights included:
-
A slight decrease in the total number of hepatitis B notifications, with 2466 reported in 2010 (2620 notifications in 2009). Hepatitis B notifications were predominantly in men and women aged 25–39 years.
-
A slight decrease in undifferentiated hepatitis C notifications, with 3517 reported in 2010 (3784 notifications in 2009). Hepatitis C was most prevalent in men and women aged 25–54 years.
-
Notifications of newly acquired hepatitis B and hepatitis C infection remained stable.
-
A slight decrease in human immunodeficiency virus (HIV) infection notifications, with 305 reported in 2010 (329 notifications in 2009). In 2010, 230 notifications (75%) were reported to be homosexually acquired. The number of HIV infections reported to be heterosexually acquired decreased from 77 in 2009 to 50 in 2010.
Note that because of the chronic nature of hepatitis B and hepatitis C infection, repeat testing and repeat notification of cases is common for these conditions. Recent improvements in methods for cleaning data have resulted in the identification of duplicate notifications for hepatitis B and C cases. This has led to a more accurate count of cases through a reduction in the number of case notifications for previous years, particularly before 2005.
Prevention activities
NSW Health has a range of policies and strategies in place to control the spread of HIV, hepatitis B and hepatitis C, including regular campaigns to promote safe sex, needle and syringe programs to provide sterile equipment to injecting drug users, and support of the management of patients with sexually transmissible infections and hepatitis C. Recent highlights have included:
-
An independent evaluation in 2010 of the NSW HIV/AIDS, Sexually Transmissible Infections and Hepatitis C Strategies 2006–2010, and the supporting Implementation Plan for Aboriginal People. The evaluation found that efforts to prevent these conditions and to provide care for those affected have been effective.
-
The 2008 Review of Hepatitis C Treatment and Care Services1 which recommended that NSW double the number of people on antiviral treatment by 2013. Policy initiatives have been implemented to: increase the capacity of specialist services; strengthen area-wide infrastructure; increase the nursing workforce; and trial the provision of treatment in community settings. Since the review, program initiatives (including establishment of additional clinical and program positions across NSW) have resulted in: a 42% increase (from 1264 people in 2005–2006 to 1800 people in 2008–2009) in the number of public patients treated for hepatitis C; and a 136% increase (from 28 sites in 2005–2006 to 66 sites in 2008–2009) in the number of public sites offering treatment.
-
Ongoing commitment to prevention policies that employ a harm reduction approach, such as the NSW Needle and Syringe Program. According to an evaluation,2 during the period 2000–2009, the Program prevented 23 324 cases of HIV and 31 953 cases of hepatitis C.
-
In 2010, the NSW Needle and Syringe Program comprised 864 outlets (332 public sector outlets, 373 pharmacies and 159 dispensing machines). Approximately 9.5 million needles and syringes were dispensed and over 12 000 referrals were provided to drug treatment services, hepatitis services and other health and welfare agencies for people who inject drugs.
-
In 2010, NSW publicly funded HIV and sexual health clinics provided 77 375 occasions of services to 6472 clients related to HIV treatment, management, and care. This was an increase of 3.2% of clients compared with 2009.
The regulation of skin penetration industries, and the enforcement of prescribed infection control and equipment standards, is an important part of bloodborne virus control in NSW. In 2010 a Skin Penetration Working Group was established to oversee policies and programs implemented through public health units (PHUs). The group aims to initiate a planning process to strengthen the infection control component of TAFE courses for the skin penetration industry.
Sexually transmissible infections
Notification data
Highlights in 2010 included:
-
A decline in the number of infectious syphilis notifications with 387 reported in 2010 (532 notifications in 2009, a peak in recent years).
-
An outbreak of lymphogranuloma venereum (LGV), with 55 notifications reported in 2010, compared with four in 2009. All notifications were reported in men, and most were aged between 30 and 50 years. The number of notifications decreased during November and December 2010. The outbreak in NSW occurred in the global context of increased rates of LGV infection in Europe and North America amongst men who have sex with men. Timely surveillance, early recognition and treatment of this disease are important.
-
A sustained increase in the number of chlamydia notifications, with 18 103 notifications. This represents a 21% increase compared with 2009 when 14 872 notifications were reported. Cases were most commonly reported in women aged 20–29 years.
-
An increase in the number of gonorrhoea notifications, with 2284 notifications. This represents a 39% increase compared with 2009 when 1638 notifications were reported. Cases were most common in men aged 20–39 years.
Overall, notifications of sexually transmissible infections (STIs) in NSW continue to rise. Chlamydia continues to be the most commonly notified STI in NSW. At least some of these increases are likely to be associated with increased screening and case detection.
Prevention activities
In 2010 in NSW, publicly funded sexual health clinics provided 23 900 occasions of services related to STI treatment, management and care. This is an increase of 4.3% compared with 2009. Services were provided to 12 513 clients, an increase of 4.1% compared with 2009.
In 2010, NSW Health led a national response to an increase in syphilis notifications amongst gay men and other men who have sex with men through The National Gay Men’s Syphilis Action Plan.3 The Plan aimed to achieve a sustained reduction in the incidence of infectious syphilis in Australian gay and homosexually active men by 2013. The Plan outlined a range of evidence-based interventions to inform prevention efforts.
In 2010, NSW Health commenced the second phase of the successful 2009 HIV and STI education campaign, Get Tested, Play Safe.4 The aim of the campaign was to reinforce STI awareness, increase testing, and improve safe sex behaviour among young people.
Enteric diseases (infectious, food and water)
Notification data
There were 6665 notifications of enteric disease in 2010, a 27% increase compared with the average annual disease count for the previous 5 years. Highlights included:
-
A large increase in the number of salmonellosis notifications, with 3671 reported in 2010. This represents an increase of 60% compared with the annual average for the previous 5 years and is the largest number of notifications on record in NSW. The increase was in part explained by an ongoing increase of Salmonella enterica serovar Typhimurium PT 170 notifications. This increase has been observed nationally and is the subject of an ongoing investigation.
-
A decrease in reports of probable outbreaks of foodborne disease, with 59 notifications affecting over 728 people reported in 2010. This represents a 15% decline when compared with the 68 notifications affecting 903 people reported in 2009.
-
A decrease in reports of probable outbreaks of viral gastroenteritis in institutions, with 518 notifications affecting 9386 people. This represents a 14% decline when compared with the 600 outbreaks affecting 11 769 people reported in 2009.
-
Eleven point-source outbreaks of Salmonella enterica serovar Typhimurium most likely associated with the consumption of sauces prepared with raw eggs, deep fried ice-cream prepared with raw eggs, and pork rolls.
Prevention activities
Food
NSW Health works with OzFoodNet nationally and the NSW Food Authority (NSWFA) locally to investigate and control Salmonella outbreaks and food contamination incidents.
In 2010, NSW Health and the NSWFA finalised the Investigation of Foodborne Illness Response Protocol – Operations Procedures Manual.
With the Environmental Health Branch the Health Risk Policy Unit assessed a number of potential food contamination issues for the NSWFA in 2010. Risk assessments were conducted for the following public health investigations:
-
High iodine content in soy milk products, resulting in immediate recall of the product.
-
Weight loss products, found to be toxic and harmful to the health of adults and children.
Drinking water
NSW Health is the public health regulator of the major water utilities through operating licences and memoranda of understanding (for Hunter Water Corporation, Sydney Water Corporation and Sydney Catchment Authority). In 2010 the Water Unit and PHUs worked with these utilities to:
-
ensure compliance with relevant guidelines including the Australian Drinking Water Guidelines5 and the Australian Guidelines for Water Recycling6
-
undertake major projects including Sydney Water’s Five-Year Drinking Water Quality Management Plan7 and the Ten Year Review of the Sydney Water Inquiry8
-
monitor the compliance of utilities with the NSW Fluoridation of Public Water Supplies Act 1957.
The Water Unit and PHUs exercise public health oversight of more than 100 water utilities in regional NSW through the NSW Health Drinking Water Monitoring Program,9 which provides guidance on drinking water monitoring and is supported by NSW Health laboratories. In 2010 there was an improvement in regional sampling compliance with:
-
96% of expected microbiological samples taken, compared with 95% in 2009
-
100% of expected chemistry samples taken, up from 98% in 2009.
NSW Health is responsible for reviewing applications from private recycled water or drinking water suppliers for licences under the Water Industry Competition Act 2006. In 2010, the Water Unit and PHUs:
-
reviewed six licence applications for recycled water
-
advised local councils and the NSW Office of Water on more than 30 new and ongoing recycled water schemes regulated under the Local Government Act 1993.
Respiratory disease (infectious and environmental)
Notification data
Highlights in 2010 included:
-
Notifications of pandemic (H1N1) 2009 influenza decreased substantially in 2010 compared with the previous pandemic year. In 2010, notifications were most commonly reported in people aged 15–50 years. In total, 66 people were admitted to intensive care units for treatment and there were eight recorded deaths (although there are likely to be many more hospitalisations and deaths associated with the infection that remained unrecognised).
-
At the time of this report the tuberculosis (TB) data for 2010 remained incomplete, however preliminary analysis indicated that there was a decrease in both the overall number of TB notifications in 2010 (392 notifications) compared with 2009 (505 notifications), and the number of multi-drug resistant tuberculosis (MDR-TB) cases identified (five cases in 2010 and 10 in 2009).
-
One case of extensively drug-resistant tuberculosis (XDR-TB) was identified in a NSW resident who had been treated previously for TB overseas. XDR-TB (TB that is resistant to isoniazid and rifampicin, plus resistant to any fluoroquinolone and at least one of three injectable second-line drugs) is a rare event in Australia and this is the second case identified.
-
An overall decrease in the number of Legionnaires’ disease notifications with 85 reported in 2010 compared with 94 in 2009. A slight increase in the number of notifications of Legionella pneumophila, with 35 reported in 2010 compared with 28 in 2009. Notifications of L. longbeachae were lower in 2010 (42 notifications) compared with 2009 (64 notifications).
Prevention activities
Pandemic control activities
In 2010, NSW public health services continued to promote vaccination against pandemic (H1N1) 2009 influenza and to prepare for a possible second pandemic wave. A thorough review of the pandemic influenza response in 2009 led to the development of the following documents in 2010:
-
Key recommendations on pandemic (H1N1) 2009 influenza.10 This is a summary report of the principle lessons learned with recommendations for future pandemic planning and response.
-
NSW Health influenza pandemic plan, Version 2.0.11 This is a major revision of the NSW pandemic plan for the health sector which acknowledges the need for greater flexibility in response options for pandemic influenza strains of varying severity. It also reinforces the key elements of pandemic influenza preparedness and response.
TB prevention and control activities
In NSW, a network of public health services provide free and confidential screening, diagnostic, treatment and management services for persons identified with tuberculosis and the general community.
Legionella control activities
In 2010 a statewide survey of cooling towers was undertaken to assess compliance with guidelines for testing of cooling towers for Legionella.
Vectorborne diseases
Notification data
Highlights in 2010 included:
-
The total number of notifications of vectorborne diseases in 2010 (1632 notifications) was similar to 2009 (1502 notifications). The most commonly notified vectorborne disease in 2010 was Ross River Virus with 1052 notifications received, a 16% increase compared with 2009 (908 notifications), but a similar number to the median number of notifications for the years 2006–2009 (1033 notifications). Barmah Forest Virus infection was the second most commonly notified vectorborne disease (252 notifications), a decrease of 30% compared with 2009 (358 notifications), and a decrease of 55% compared with the median number of notifications for the years 2006–2009 (554 notifications).
-
A 43% increase in the number of dengue notifications with 194 notifications reported compared with 136 notifications in 2009. While there is no local transmission of dengue in NSW, globally it is the most common mosquito-borne viral disease of humans and in recent years has become a major international public health concern. With increasing international travel and migration, mosquito-borne diseases such as dengue, malaria and chikungunya may become increasingly common among travellers returning to NSW.
Prevention activities
The Environmental Health Branch administers the NSW arbovirus surveillance program. This program encompasses mosquito trapping and monitoring of virus activity in mosquito populations, and monitoring for antibody seroconversion of sentinel chicken flocks that are located in a number of strategic sites throughout rural NSW. The trapping and surveillance program is designed to cover the period of seasonal increase and decrease in the populations of the major arbovirus vectors, from mid-spring to mid-autumn, and also to cover the period for natural activity and transmission of arbovirus infections.
Environmental exposures and risk assessment
Air pollution
Air pollution arises from many sources including bushfires, car engines, wood-burning heaters, power stations, mining and other industries. The Environmental Health Branch is involved in a range of activities to improve air quality and in 2010 represented NSW Health in a multi-agency senior advisory group on coal mining. In collaboration with local PHUs, the Branch engaged in a number of activities to address concerns raised by the local community in relation to air quality associated with coal mining and power stations in the Upper Hunter Region. For example:
-
Hunter New England Health Study,12 including analysis of emergency department presentations, hospital separations, cancer and death register data
-
Initiation of a cancer cluster investigation13 and independent review that found the cluster was a chance occurrence
-
The establishment of the Expert Advisory Committee on Air Pollution that found that there were indications that asthma may be a more important issue in the Upper Hunter region14
-
An analysis of general practitioner presentations, treatments and diagnoses to examine the potential health effects of the mining industry and other exposures in Singleton, Muswellbrook and Denman.15
Major development assessment
Historically, mining activity has contributed to the presence of lead in the environment of the Broken Hill community. In 2010, NSW Health evaluated the impact of the re-opening of the Broken Hill lead mine on community blood levels. An evaluation of the health risk assessment undertaken by the company was completed. The evaluation recommended that a program of blood lead monitoring be instituted as part of the mine’s conditions of approval.
In 2010, the Environmental Health Branch represented NSW Health in a multi-agency senior advisory group on coal-seam gas issues.
Aboriginal health
Housing for Health
Housing for Health is an evidence-based housing repair and maintenance program that focuses on improving the safety and health of residents in those homes.16
-
Since 1998, over 11 500 Aboriginal people living in 2771 houses in 72 Aboriginal communities have benefited from the Housing for Health program.
-
Approximately 70 000 items have been fixed that specifically relate to improved safety and health through the program.
-
An evaluation of the NSW Housing for Health program found that populations exposed to the program were 40% less likely to be hospitalised with infectious diseases compared with the rest of the rural NSW Aboriginal population.17 These findings demonstrate the importance of social determinants in improving health outcomes for Aboriginal people.
In 2010 the Housing for Health program was involved in the following activities:
-
Completion of projects in Glenn Innes, Toomelah/Boggabilla, Narrabri/Wee Waa, Goodooga, Dorrigo, Tabulam and Tingha/Inverell.
-
New projects in Bourke, Enngonia, Wilcannia and La Perouse.
-
A trial project with the Aboriginal Housing Office Backlog Maintenance Program in Coffs Harbour.
The Aboriginal Communities Water and Sewerage Program
Clean water and functioning sewerage systems are a prerequisite for good health. Widespread availability of these essential services will improve outcomes by reducing communicable diseases such as skin infections and diarrhoeal illness.
The Aboriginal Communities Water and Sewerage Program is a joint partnership between the NSW Government and the NSW Aboriginal Land Council.18 The Program aims to ensure adequate operation, maintenance and monitoring of water supplies and sewerage systems in more than 60 Aboriginal communities in NSW. NSW Health is involved in the development and roll-out of the Program across the state.
-
31 Aboriginal communities with a population of 3000 people are now receiving improved water and sewerage services. This includes 17 new communities in 2010, servicing a population of around 1800 people.
-
PHUs are working with communities, the NSW Office of Water, local water utilities and service providers to implement Risk-Based Water and Sewerage Management Plans.
The Aboriginal Environmental Health Officer Training Program
The Aboriginal Environmental Health Officer Training Program aims to increase opportunities for workforce participation by Aboriginal people and enhance the involvement of Aboriginal people in improving environmental health outcomes. Since 1998, 11 Aboriginal Environmental Health Officers have graduated from the Program. Six Aboriginal Environmental Health Officer Trainees were participating in the Program in 2010. The percentage of Aboriginal people employed within the NSW Health Environmental Health workforce increased from 0% in 1998 to over 17% in 2008.
Program activities
-
In 2010, two new trainee positions were created under funding agreements between the Aboriginal Environmental Health Unit and the former area health services.
-
One trainee position was created under an agreement between the Aboriginal Environmental Health Unit, the Sydney South West PHU and Camden Council. Negotiations are in place to expand the Program further.
Acknowledgments
Protecting the health of the community is a collaborative effort, involving public health units, clinicians, laboratory scientists, affected communities, and other government and community-based organisations. We thank all those involved for the role they played in NSW in 2010.
References
[1] NSW Department of Health. Review of Hepatitis C Treatment and Care Services. Available from: http://www.health.nsw.gov.au/pubs/2008/080200_hep_c_report.html (Cited May 2011.)[2] Wilson D and Australian Government Department of Health and Ageing. Return on investment 2: evaluating the cost-effectiveness of needle and syringe programs in Australia 2009. Available from: http://www.health.gov.au/internet/main/publishing.nsf/Content/needle-return-2 (Cited May 2011.)
[3] STIGMA. The National Gay Men’s Syphilis Action Plan. 2009. Available from: http://stigma.net.au/resources/National_Gay_Mens_Syphilis_Action_Plan.pdf (Cited May 2011.)
[4] NSW Department of Health. Get Tested, Play Safe campaign. 2011. Available from: http://www.gettested.com.au/#/HOW%20MANY%20PEOPLE%20HAVE%20YOU%20SLEPT%20WITH?/ (Cited May 2011.)
[5] National Health and Medical Research Council and Natural Resource Management Ministerial Council. Australian drinking water guidelines 6, 2004. Available from: http://www.nhmrc.gov.au/_files_nhmrc/file/publications/synopses/adwg_11_06.pdf (Cited May 2011.)
[6] Natural Resource Management Ministerial Council; Environment Protection and Heritage Council. Australian Health Ministers’ Conference. Australian Guidelines for Water Recycling: Managing Health and Environmental Risks (Phase 1). 2006. Available from: http://www.ephc.gov.au/sites/default/files/WQ_AGWR_GL__Managing_Health_Environmental_Risks_Phase1_Final_200611.pdf (Cited June 2011.)
[7] Sydney Water. Five-Year Drinking Water Quality Management Plan. 2010. Available from: http://www.sydneywater.com.au/WaterQuality/FiveYearDrinkingWaterQualityManagementPlan/ (Cited May 2011.)
[8] NSW Government. Ten Year Review of the Sydney Water Inquiry. 2010. Available from: http://210.247.145.33/Publications/FactSheets/McClellan_Review_-_Ten_year_review_-_NSW_Government_response_to_recommendations.pdf (Cited May 2011.)
[9] NSW Department of Health. Drinking Water Monitoring Program. December 2005. Available from: http://www.health.nsw.gov.au/publichealth/environment/water/drinkwater_nsw.asp (Cited May 2011.)
[10] NSW Department of Health. Key recommendations on pandemic (H1N1) 2009 influenza from the NSW Health Emergency Management Committee. Available from: http://www.health.nsw.gov.au/pubs/2010/h1n1_2009_key_recomm.html (Cited May 2011.)
[11] NSW Department of Health. NSW Health influenza pandemic plan, Version 2.0. Available from: http://www.health.nsw.gov.au/policies/pd/2010/PD2010_052.html (Cited May 2011.)
[12] NSW Department of Health. Respiratory and cardiovascular diseases and cancer among residents in the Hunter New England Area Health Service. Available from: http://www.health.nsw.gov.au/pubs/2010/pdf/HNE_Respi_Cardio_Disease.pdf (Cited May 2011.)
[13] NSW Department of Health. Singleton cancer cluster investigation. Available from: http://www.health.nsw.gov.au/resources/news/pdf/singleton_cancer.pdf (Cited May 2011.)
[14] NSW Department of Health. Conclusion of the EAC on the findings of the General Practitioner data analysis for the Upper Hunter. Available from: http://www.health.nsw.gov.au/PublicHealth/environment/air/apeac.asp (Cited May 2011.)
[15] NSW Department of Health. Analysis of BEACH general practitioner encounter data to examine the potential health effects of the mining industry and other exposures in Singleton, Muswellbrook and Denman. Available from: http://www.health.nsw.gov.au/pubs/2010/pdf/beach_report.pdf (Cited May 2011.)
[16] NSW Department of Health. Housing for Health. Available from: http://www.health.nsw.gov.au/PublicHealth/environment/aboriginal/housing_health.asp (Cited May 2011.)
[17] NSW Department of Health. Closing the Gap: 10 Years of Housing for Health in NSW. An evaluation of a healthy housing intervention. Available from: http://www.health.nsw.gov.au/pubs/2010/pdf/housing_health_010210.pdf (Cited May 2011.)
[18] NSW Aboriginal Land Council and NSW Government. Aboriginal water supply and sewerage program. Available from: http://www.alc.org.au/media/27358/Final_A3%20Folded_3mm%20Bleed.pdf (Cited May 2011.)
a A child is assessed as fully vaccinated at 12 months of age if he/she has received age-appropriate vaccinations against diphtheria, tetanus, pertussis, polio, Haemophilus influenzae type B and hepatitis B.
b A child is assessed as fully vaccinated at 2 years of age (24 to <27 months of age) if he/she has received age-appropriate vaccinations against diphtheria, tetanus, pertussis, polio, Haemophilus influenzae type B, hepatitis B, measles, mumps and rubella.
c A child is assessed as fully vaccinated at 5 years of age if he/she has received age-appropriate vaccinations against diphtheria, tetanus, pertussis, polio, Haemophilus influenzae type B, hepatitis B, measles, mumps and rubella.
* Please note that from the May–June 2011 issue of the Bulletin, ‘notifiable conditions’ are now referred to in both text and tables as ‘scheduled medical conditions’, reflecting the terminology of the NSW Public Health Act 2010.

