Dental caries in children: a comparison of one non-fluoridated and two fluoridated communities in NSW
Amit Arora A B and Robin Wendell Evans AA Population Oral Health, Faculty of Dentistry, The University of Sydney
B Corresponding author. Email: amit.arora@sydney.edu.au
NSW Public Health Bulletin 21(12) 257-262 https://doi.org/10.1071/NB10029
Published: 8 March 2011
Abstract
Aim: The aim of the Child Dental Health Survey in Lithgow was to establish the oral health status of primary schoolchildren to assist the local council in deciding whether to fluoridate the water and to provide a baseline for future monitoring of changes in caries rates. Methods: All six primary schools in Lithgow were invited to participate, and 653 children aged 6–12 years were clinically examined for dental caries. World Health Organization criteria were used, whereby a decayed tooth is defined as a cavity into the dentine. Caries prevalence was measured as the mean number of decayed, missing and filled teeth (primary: dmft; secondary: DMFT). Significant caries indices were calculated to categorise children with the mean dmft/DMFT score of the highest 30 percentage (SiC) and the highest 10 percentage (SiC10) of caries. Data for Lithgow were compared with school dental service data for the socioeconomically comparable fluoridated townships of Bathurst and Orange. Results: The primary dentition caries estimates (dmft, SiC and SiC10) in Lithgow children aged 6 years were 0.92, 2.72 and 5.81, respectively; the estimates for permanent dentition caries (DMFT, SiC and SiC10) in Lithgow children aged 12 years were 0.69, 2.05 and 6.41, respectively. The caries prevalence in the permanent dentition of Lithgow children was significantly higher than that in children living in the fluoridated towns of Bathurst and Orange. No significant differences were observed in the estimates for primary teeth. Conclusion: Although the mean levels of dental caries in schoolchildren in Lithgow were low, oral health inequalities exist between children residing in non-fluoridated Lithgow and the fluoridated locations of Orange and Bathurst. The local council decided that Lithgow will have fluoridated water by December 2010.
The prevalence of dental caries has declined over time among children in most industrialised countries,1,2 which can be attributed to increased use of fluorides, improved oral hygiene and a decreased frequency of sugar intake.3 In 1958, the World Health Organization (WHO) recognised the importance of community water fluoridation and has repeatedly supported it as a good public health policy to reduce the risk of dental caries.4 However, the role of the community in decisions to fluoridate and the legislation for its implementation vary throughout the world. For example, water fluoridation is mandatory in Singapore and Ireland,5 whereas in the United States there is no federal legislation on fluoridation and the decision depends on each state.5
Water fluoridation is not mandatory in New South Wales (NSW) and the decision to fluoridate water supplies rests with local government councils under the NSW Fluoridation of Public Water Supplies Act 1957.6 Water fluoridation has been the predominant public health approach for caries prevention in NSW because of widespread coverage with public water supplies, and it is the most cost-effective, equitable, safe means of providing protection from tooth decay.7 More than half of NSW residents live in Sydney, which commenced water fluoridation in 1968.8 In 1993, 100% of metropolitan Sydney was fluoridated, but only 59% of people living elsewhere in NSW had access to fluoridated water.9 In an effort to promote further uptake of fluoridation and to reduce the burden of dental caries, in 2004 the NSW Government increased the capital subsidy for installation of new fluoridation plants from 50% to 100%. Since 2004, efforts by NSW Health, in partnership with area health services, the Australian Dental Association and local governments, has resulted in 94% of the NSW population having access to fluoridated water.10 In 2003, after 10 years of water fluoridation in the Blue Mountains, Evans et al.11 found that water fluoridation had reduced the risk of one or more decayed teeth in both the primary and the permanent dentition by 65%. Researchers have reported significant differences in caries prevalence between non-fluoridated and fluoridated areas of NSW.12,13 Consequently, to promote water fluoridation in the 6% of rural communities in NSW that are non-fluoridated, locally relevant, up-to-date information on oral health is required.
Lithgow is a rural town located 145 km west of Sydney, with a population of 19 756. In 2005 it was the only area within the boundaries of the Sydney West Area Health Service that remained unfluoridated (Sivaneswaran S, written communication, December 2005). The aim of the Child Dental Health Survey in Lithgow was to establish the oral health status of schoolchildren aged 6–12 years to assist the local council decide whether to fluoridate the water, and to provide a baseline for future monitoring of changes in caries rates. In contrast to the previous broad surveys of children’s oral health in NSW, which included only a few children from this community, a systematic survey of Lithgow children’s dental health was conducted by two dental health professionals using WHO criteria.
Methods
The school principals of all six listed primary schools in the Lithgow local government area were approached by letter to take part in the survey. The parents of all schoolchildren were then invited to take part in the dental survey through a take-home information pack containing information and a consent form. Weekly reminders were sent for 4 weeks using the school newsletters. Children participated in the survey if written consent had been obtained from their parents.
Children aged 6–12 years were clinically examined between August 2006 and November 2006. Children were examined by two public health dental specialists in schoolrooms with halogen lights as the light source. Teeth were examined wet, and if necessary a ball-ended WHO probe was used for exploration. The diagnostic criteria for dental caries were those of the WHO, whereby a decayed tooth is defined as a cavity into the dentine.14 The scores of the primary examiner (AA) were calibrated daily under the supervision of a calibrating examiner (RWE), and examiner reliability was assessed via Cohen’s Kappa statistic15 on duplicated scores obtained from both intra- and inter-examinations. The kappa value for inter-examiner reliability was 0.93, and the intra-examiner reliability was 0.98.
Caries prevalence is often represented as the mean number of teeth that are decayed, missing due to decay (extracted) or filled due to decay (termed dmft for primary dentition and DMFT for permanent dentition).16 In this study, caries prevalence in primary teeth is reported for children aged 6–10 years as primary (baby) teeth exfoliate with age, and that in permanent teeth is reported for children aged 6–12 years. As the distribution of caries prevalence is not normal but is highly skewed to particular population subsections, mean scores do not capture this skewness. The significant caries index (SiC) is the mean dmft/DMFT score of the 30% of the population with the highest scores.17,18 This index can be modified to the mean dmft/DMFT score of the 10% of the population with the highest scores (SiC10).
As it is possible that the children examined were not representative of the school-aged population, the estimated resident population at 30 June 2006 of children aged 6–12 years in Lithgow was used to calculate sampling weights for each child.19 These weights were applied when calculating age-specific indices to produce estimates that were representative of children aged 6–12 years in Lithgow.
Data from Lithgow were compared with school dental service data from the socio-economically comparable fluoridated townships of Bathurst and Orange. Statistical analysis was undertaken with EpiInfo (version 3.3.2, CDC, Atlanta, USA). Comparisons between the mean dmft/DMFT scores of children in Lithgow and Bathurst and Orange were tested with non-parametric methods (Wilcoxon signed rank test).
Approval to conduct this survey was obtained from the Human Research Ethics Committees of the University of Sydney, the NSW Department of Education and Training, the Catholic Education Board, and the Sydney West Area Health Service. The parents of children found to have caries were notified and given a referral to the public dental health system of the township.
Results
All the schools agreed to participate. Of the 1589 parents contacted, 689 (44%) gave consent for their children to be examined. Clinical data were available for the 653 children who were at school on the day of the examinations. The overall sample included equal proportions of boys and girls. No statistically significant difference in caries experience was observed by gender in the primary or permanent dentition.
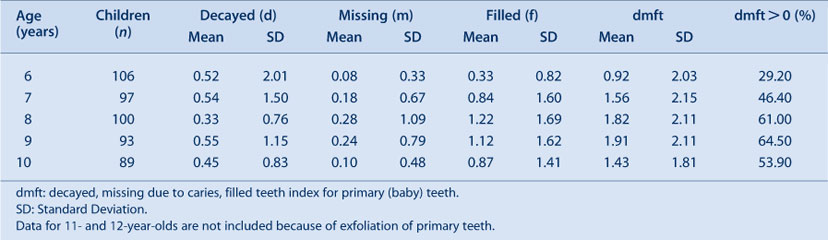
The population-adjusted caries experience in primary teeth of children aged 6–10 years is shown in Table 1. The mean dmft score increased from 0.92 to 1.91 between the ages of 6 and 9 years and then declined to 1.43 at age 10 years. The percentage of children with primary decay (dmft > 0) steadily increased across the age range 6–9 years, from 29.2% to 64.5%; however, this percentage subsequently decreased, and at 10 years of age only 53.9% of children showed evidence of decay in the primary teeth.
|
The SiC and SiC10 for the primary teeth of children aged 6–10 years are shown in Figure 1. For the 30% of children with the most decay, the mean dmft per child was considerably higher than the mean for the entire age group, and ranged between 2.72 and 4.38 dmft per child. For the 10% of children with the most caries, the SiC10 scores of 6- and 9-year-old children were more than six times and three times greater than the mean dmft scores, respectively.

|
The population-adjusted caries prevalence in permanent teeth of children aged 6–12 years is shown in Table 2. The mean DMFT score across all age groups was low, with a 12-year-old DMFT of 0.69. Less than 15% of children aged 6–8 years had permanent tooth decay (DMFT > 0); however, by the end of primary school, 28.4% of children aged 12 years had permanent tooth decay.

|
The SiC and SiC10 for the permanent teeth of children aged 6–12 years are shown in Figure 2. The SiC scores increased from 0.07 DMFT per child for children aged 6 years to 2.05 DMFT per child for children aged 12 years and, for each age group, ranged from approximately 2.5 to 3 times higher than the average DMFT. Across all age groups, the SiC10 scores were 4–10 times higher than the corresponding age-specific mean DMFT scores.

|
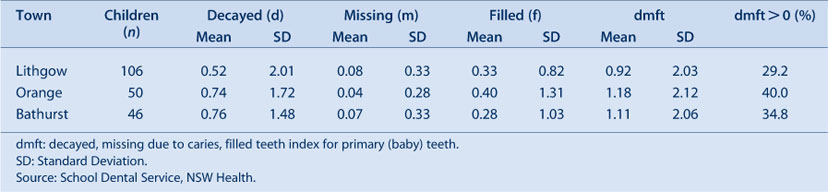
The caries rates in the primary dentition of Lithgow children were not statistically different from those in Bathurst and Orange (Table 3). In Lithgow, the mean dmft for children aged 6 years was 0.92, lower than the values recorded by the school dental services in Bathurst and Orange; however, this difference was not statistically significant.
|
Caries prevalence in the permanent dentition of Lithgow children was significantly higher than that of children living in the fluoridated towns of Bathurst and Orange (Table 4). The mean DMFT for children aged 12 years was 0.69 in Lithgow, 0.33 in Orange and 0.29 in Bathurst.

|
Discussion
Caries rates in the permanent teeth of Lithgow children were significantly higher than in those living in the fluoridated towns of Orange and Bathurst. No statistically significant differences were observed in caries prevalence in primary teeth between the three townships. The data from the survey provide an important snapshot of the oral health status of Lithgow children and were presented to the local council for consideration of the fluoridation proposal.
A potential limitation of this study was the 44% response rate. It was anticipated that the participation rate would be good as the dental examinations were carried out at school; nevertheless, absenteeism was common. The response rate was similar to those of previous studies.20 To overcome a possible sampling bias, a weighting procedure was used. As this study reports on the findings of clinical examinations, we did not report on the potential confounding factors for caries experience. We have, however, taken these into consideration and are conducting further research.
Caries prevalence in primary teeth increased between the ages of 6 and 9 years and then declined due to natural exfoliation. It was also observed that the number of filled primary and permanent teeth increased with age. A possible explanation could be the progress of carious lesions over time in the absence of fluoridation and the need for dental restoration. In our study, the mean dmft for children aged 6 years in Lithgow was 0.92, much lower than the statewide dmft of 1.53 for 5–6-year-olds reported in 2007.13 The dmft was also lower than the mean for 5–6-year-olds in the Sydney West Area Health Service, which was found to be 1.77 in 2007.13 Our data for other age groups were consistent with those for other non-fluoridated areas of NSW, such as Mudgee (dmft = 1.4) (Sivaneswaran S, written communication, August 2009).
The caries experience in the permanent dentition was similar to that for primary teeth. The DMFT for children aged 12 years in Lithgow was 0.69, lower than the statewide DMFT score for 11–12-year-old children reported in 200713 and also lower than the mean DMFT of 0.88 for 11–12-year-olds in Sydney West Area Health Service in 2007.13
The caries rates in the permanent teeth of Lithgow children were higher than the rates in children living in Orange and Bathurst. This may indicate that water fluoridation reduces the risk for dental decay, as noted in other publications from NSW.11–13 This was not, however, the case for the primary dentition. The finding that the differences in caries prevalence were not statistically significant for primary teeth may have been due to differences in the populations sampled in the three communities. Furthermore, our rates for the fluoridated and unfluoridated areas were lower than the statewide data.13 This may be due to overreporting of dental decay in statewide examinations, as the State diagnostic criteria included cavitated and non-cavitated carious lesions.
We used the WHO clinical criteria to diagnose caries, whereas the school dental service has access to radiographs as well, resulting in differences in diagnostic criteria and the finding of more caries. In our study, the examiners’ scores were highly reliable, as the clinical examinations were conducted by trained and calibrated dental public health specialists; the school dental service data were collected by uncalibrated examiners. Our diagnostic criteria for caries are more specific than sensitive, and our technique was less invasive, as we did not use radiographs as a diagnostic tool.
The findings of our study on caries prevalence among school-aged children and on parental support on water fluoridation21 were presented to the local council in the hope that this information would encourage it to support the fluoridation proposal. Following this study, the local council commissioned an independent body (Western Research Institute, Bathurst) to conduct a survey on support for fluoridation in Lithgow. It is heartening to note that 72% of households voted in favour of fluoridation (Murphy T, written communication, August 2009), and the council at its ordinary meeting in November 2007 resolved that: ‘council proceed with water fluoridation and request the installation of the necessary infrastructure’.22 Subsequently, Lithgow Council wrote to the Director-General of Health requesting fluoridation of the public water supplies under Section 6 of the Fluoridation of Public Water Supplies Act 1957. By the end of 2010, the Lithgow community will have access to fluoridated water. Future investigations will be needed to assess the benefit of water fluoridation in Lithgow.
Conclusion
Although the mean levels of dental caries in schoolchildren in Lithgow were low, oral health inequalities exist between children residing in non-fluoridated Lithgow and the fluoridated locations of Orange and Bathurst. The local council has decided that Lithgow will have fluoridated water.
Editor's note
Lithgow was gazetted to be fluoridated on 31 August 2010 and this will be implemented during 2011.23
Acknowledgments
We are grateful for support given by Dr Athin Narayan Sujeer, Dr Shanti Sivaneswaran (Centre for Oral Health Strategy, NSW Health) and Ms Ramona Grimm, and for statistical advice given by Dr Karen Byth (Westmead Hospital) and Ms Anne Ellershaw (Australian Research Centre for Population Oral Health, University of Adelaide). We are grateful to Elisabeth Heseltine for advice on the writing and editing of this paper. The schoolchildren, principals, teachers and parents are also gratefully acknowledged. This study was funded by the Centre for Oral Health Strategy, NSW Health.
References
[1] Marthaler TM. Changes in dental caries 1953–2003. Caries Res 2004; 38 173–81.| Changes in dental caries 1953–2003.Crossref | GoogleScholarGoogle Scholar | 1:STN:280:DC%2BD2c3lsVKgtA%3D%3D&md5=b7c7086b7d2e58fb0c9858ab1653dcaeCAS | 15153686PubMed |
[2] Peterson PE. Continuous improvement of oral health in the 21st century – the approach of the WHO Global Oral Programme. The World Health Report. Geneva: World Health Organization; 2003.
[3] Konig KG. Changes in the prevalence of dental caries: how much can be contributed to changes in diet? Discussion paper. Caries Res 1990; 24 16–8.
| Changes in the prevalence of dental caries: how much can be contributed to changes in diet? Discussion paper.Crossref | GoogleScholarGoogle Scholar |
[4] World Health Organization. WHO Expert Committee on Oral Health Status and Fluoride Use. Fluorides and Oral Health. WHO Technical Report Series No. 846. Geneva: World Health Organization; 1994.
[5] Jones S, Lennon M. Fluoridation. In: Pine CM, editor. Community Oral Health. Bath: Wright; 1997. pp. 221–47.
[6] Sivaneswaran S, Chong GTF, Blinkhorn AS. Successful fluoridation plebiscite in the township of Deniliquin, New South Wales, Australia. J Public Health Dent 2010; 70 163–6.
| 20210864PubMed |
[7] Australian Research Centre for Population Oral Health, Dental School, The University of Adelaide The use of fluorides in Australia: Guidelines. Aust Dent J 2006; 51 195–9.
| The use of fluorides in Australia: Guidelines.Crossref | GoogleScholarGoogle Scholar | 16848271PubMed |
[8] Spencer AJ, Slade GD, Davies M. Water fluoridation in Australia. Community Dent Health 1996; 13 27–37.
| 8897748PubMed |
[9] Sivaneswaran S. Water fluoridation successes in NSW 2003 to 2006. Newsletter Public Health Assoc Aust 2006; 24 7–10.
[10] Sivaneswaran S. Investing upstream – water fluoridation successes in New South Wales. Newsletter Public Health Assoc Aust 2009; 26 6–7.
[11] Evans RW, Hsiau ACY, Dennison PJ, Patterson A, Jalaludin B. Water fluoridation in the Blue Mountains reduces risk for tooth decay. Aust Dent J 2009; 54 368–73.
| Water fluoridation in the Blue Mountains reduces risk for tooth decay.Crossref | GoogleScholarGoogle Scholar | 1:STN:280:DC%2BC3c3oslSqsQ%3D%3D&md5=5c4dcdacda4416e84a8ac24f6114347fCAS | 20415937PubMed |
[12] Armfield J. Public water fluoridation and dental health in New South Wales. Aust N Z J Public Health 2005; 29 477–83.
| Public water fluoridation and dental health in New South Wales.Crossref | GoogleScholarGoogle Scholar | 16255452PubMed |
[13] Phelan C, Byun R, Skinner JC, Blinkhorn AS. Child Dental Health Survey 2007: a snapshot of the oral health status of primary school-aged children in NSW. N S W Public Health Bull 2009; 20 40–5.
| Child Dental Health Survey 2007: a snapshot of the oral health status of primary school-aged children in NSW.Crossref | GoogleScholarGoogle Scholar | 19401067PubMed |
[14] World Health Organization. Oral Health Surveys: Basic Methods. 4th ed. Geneva: World Health Organization; 1997.
[15] Cohen J. A coefficient of agreement for nominal scales. Educational and psychological measurement. Educ Psychol Meas 1991; 51 95–101.
[16] Klein H, Palmer CE, Knutson JW. Studies on dental caries: dental status and dental needs of elementary school children. Public Health Rep 1938; 53 751–65.
| Studies on dental caries: dental status and dental needs of elementary school children.Crossref | GoogleScholarGoogle Scholar |
[17] Bratthall D. Introducing the Significant Caries Index together with a proposal for a new global oral health goal for 12-year-olds. Int Dent J 2000; 50 378–84.
| 1:STN:280:DC%2BD3M3ls1KntA%3D%3D&md5=37b74e42aea819445f517e82953a224aCAS | 11197197PubMed |
[18] Nishi M, Stjernsward J, Carlsson P, Bratthall D. Caries experience of some countries and areas expressed by the Significant Caries Index. Community Dent Oral Epidemiol 2002; 30 296–301.
| Caries experience of some countries and areas expressed by the Significant Caries Index.Crossref | GoogleScholarGoogle Scholar | 12147171PubMed |
[19] Australian Bureau of Statistics. Population by age and sex, Australia, 2006. Canberra: Australian Bureau of Statistics; 2007. Available at: www.abs.gov.au/ausstats (Cited 15 July 2009).
[20] Brennan DS, Spencer AJ, Roberts-Thomson KF. Periodontal disease among 45–54 year olds in Adelaide, South Australia. Aust Dent J 2007; 52 55–60.
| Periodontal disease among 45–54 year olds in Adelaide, South Australia.Crossref | GoogleScholarGoogle Scholar | 1:STN:280:DC%2BD2s3ovFymtg%3D%3D&md5=392415cf7f47ed6c21f3fe21052df5a6CAS | 17500165PubMed |
[21] Arora A, Evans RW, Sivaneswaran S, Sujeer AN, Blinkhorn AS. Parental support for water fluoridation in Lithgow, New South Wales. Aust Dent J 2010; 55 417–22.
| Parental support for water fluoridation in Lithgow, New South Wales.Crossref | GoogleScholarGoogle Scholar | 1:STN:280:DC%2BC3M%2FitFOhtA%3D%3D&md5=39cb81b184a24d9e0ace717075639637CAS | 21133941PubMed |
[22] Lithgow City Council. Minutes Ordinary Meeting of Council. Lithgow: Lithgow City Council, 2007. Available at: http://www.council.lithgow.com/minutes/minutes_071119.pdf (Cited 25 March 2009.)
[23] Fluoridation of Public Water Supplies Act 1957. NSW Government Gazette 111: 4359. 3 September 2010.

