Child Dental Health Survey 2007: a snapshot of the oral health status of primary school-aged children in NSW
Claire Phelan A D , Roy Byun B , John C. Skinner A and Anthony S. Blinkhorn CA Centre for Oral Health Strategy, NSW Department of Health
B NSW Public Health Officer Training Program, NSW Department of Health
C Faculty of Dentistry, University of Sydney
D Corresponding author. Email: claire_phelan@wsahs.nsw.gov.au
NSW Public Health Bulletin 20(4) 40-45 https://doi.org/10.1071/NB08069
Published: 27 April 2009
Abstract
Objectives: The Child Dental Health Survey 2007 was commissioned to establish the oral health status of school children in NSW aged 5–12 years, to provide reliable regional oral health statistics and contribute to national population-based data collections. Methods: A total of 7975 children were clinically examined at 107 public, catholic and independent schools across NSW. Results: Key findings from the survey include: mean dmft for 5–6-year-olds of 1.53; mean DMFT for 11–12-year-olds of 0.74; 61.2% of 5–6-year-olds and 65.4% of 11–12-year-olds have never experienced decay in their primary and permanent teeth, respectively. These figures compare favourably to national benchmarks set in 2001. Conclusions: Data from the survey will be used as a baseline to measure the success of early intervention and prevention programs, for international comparisons, to provide solid evidence to support population oral health planning and for ongoing surveillance of populations of interest.
In 2001, the National Oral Health Monitoring Group proposed key indicators for assessment of oral health over time in Australia.1 Two signature age groups were chosen as benchmark age groups. These were 5–6 and 11–12-year-old children. These age groups are used by the World Health Organization (WHO) in order to allow international comparisons of children’s oral health status.2 Children’s dental caries (decay) is measured for primary (baby) teeth using the dmft (decayed, missing due to caries, filled teeth) index and for permanent teeth using the DMFT (Decayed, Missing due to caries, Filled Teeth) index. The lower the index, the better the dental health of the population. In addition, the proportion of children free from decay is also recorded. This measurement is critical to assess the impact of preventive programs and the need for clinical dental services.
In New South Wales (NSW), recent epidemiological data about children’s oral health were based on those seeking treatment in the public dental system and therefore were biased towards populations with high disease levels. In order to provide meaningful data that would allow interstate and international comparisons, a scientifically based Child Dental Health Survey was commissioned by the Chief Dental Officer for NSW in 2007.
The survey was conducted in conjunction with NSW area health services, the Australian Research Centre for Population Oral Health (ARCPOH) at the University of Adelaide and the University of Sydney. Ethics approval for the survey was granted from the NSW Population and Health Services Research Ethics Committee and from the State Education Research Approvals Process, NSW Department of Education and Training.
The aim of the survey was to assist in planning oral health services by providing reliable regional oral health statistics for primary school-aged children while also contributing to national population-based data collections. The survey represents a more efficient approach to oral health data collections than those available through public dental system collections or through previous risk assessment programs undertaken in NSW.3 It is the first survey in 20 years to use a randomised sample to investigate and report on various groups within the NSW child population. The aim of this paper is to present a snapshot of regional statistics and to provide evidence on the distribution of dental disease in children from populations of interest.
Note that within NSW Health, the term ‘Aboriginal’ is generally used in preference to ‘Aboriginal and Torres Strait Islander’, in recognition that Aboriginal people are the original inhabitants of NSW.
Methods
The survey covered a representative sample of children aged 5–12 years from metropolitan and non-metropolitan public, Catholic and independent schools in NSW. A two-stage sampling design was employed, with schools defined as the primary sampling units. First, schools were stratified by area health service region and a sample of schools was selected from each region to ensure adequate regional sample sizes. Prior to selection, schools within each region were sorted by the Index of Relative Socio-Economic Disadvantage, which is one of the Socio-Economic Indexes for Areas (SEIFA), to ensure a spread of schools from regions with various socioeconomic backgrounds. Second, a random sample of children enrolled at each of these schools was selected (n = 76). Lists of student names were created and sorted by date of birth. Age was calculated as date of examination minus date of birth. Skip intervals were then applied for each age group to generate the required sample.
Children aged 5–6 and 11–12 years were over-sampled to allow area health service comparisons of disease status. These data have been identified by NSW Health as key data to support state and area health service planning, reporting and performance indicators.
Twenty teams of calibrated dental therapists and dental assistants collected the information during the 2007 calendar year. Standard equipment, including portable air syringe compressors, lighting and dental instruments were used to maximise inter-examiner reliability. A principal survey examiner conducted the training and calibration of examination teams, and also completed inter-examiner reliability testing on a sub-sample of children. The reliability of each of the examiners relative to the principal survey examiner was determined by calculating the intra-class correlation coefficient (ICC) of count data for each replicate pair and the Kappa values for categorical coding of individual tooth and surface status. The ICC was calculated using the method of Shrout and Fleiss, and Kappa statistics were calculated using the method of Cohen.4,5
Data were recorded on optical mark recognition forms developed by ARCPOH. These forms were retrofitted to TeleForm version 10 for scanning and verification. Data were then exported to Microsoft Access for further cleaning, following which data analysis was performed in SAS for Windows version 9.1.3.
Basic demographic data were collected, including date of birth, sex, postcode of residence and Aboriginality. Country of mother’s birth and Centrelink concession card status were also collected. The level of dental caries in an individual was recorded by tooth surface and used to calculate tooth-level status. The average decay experience (mean number of dmf/DMF teeth) is an expression of the severity of the disease in the population. Need for immediate treatment (defined as requiring dental treatment for pain, abscessed teeth, grossly decayed teeth, avulsed or fractured teeth, or other severe conditions with oral manifestations) was recorded as was dental fluorosis using the Thylsrup and Fejerskov (T-F) Index.6
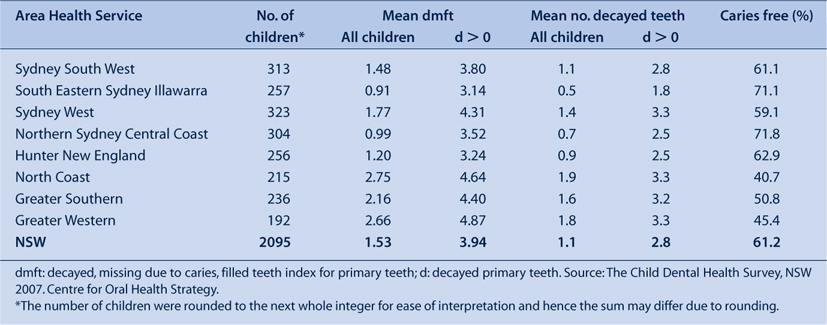
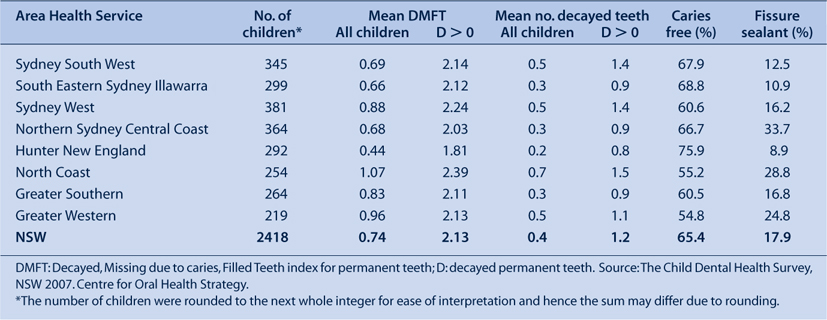
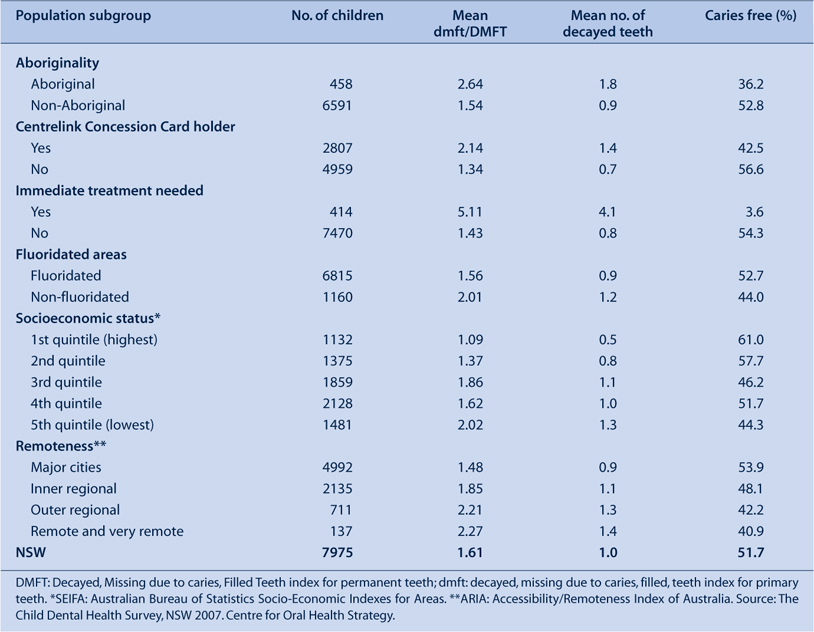
For each child, the postcode of residence was used to determine the area health service, fluoridation status of the reticulated water supply using the database maintained by the Centre for Oral Health Strategy, socioeconomic status using the SEIFA index and remoteness categories using the Accessibility/Remoteness Index for Australia. The estimated residential population at 30 June 2007 of 5–12-year-old children within each area health service region and age-specific class sizes in each school, were used to calculate sampling weights for each child.7 These weights were applied when calculating regional age-specific indices and indices for population subgroups, to obtain estimates that were representative of 5–12-year-old children in NSW (Tables 1–3). NSW Health consulted closely with ARCPOH throughout the survey to ensure high reliability and validity of data so that national comparisons would be possible.
|
|
|
Results
Assessment of inter-examiner reliability
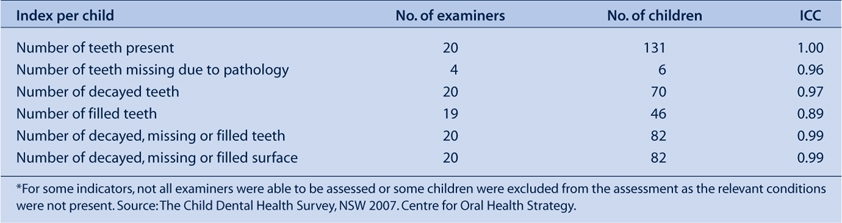
To assess the reliability of clinical measurements between examiners, replicate pairs of examinations were conducted with 131 children, who were examined by the principal survey examiner and by one of 20 clinical examiners. The number of replicate pairs for each examiner ranged from five to eight and examinations were conducted at nine different schools, with the number of examiners per school ranging from one to six.
High levels of agreement were obtained for tooth presence, missing, decayed or filled teeth (ICC values ranged 0.89 to 1.00; Table 4). Excellent agreement was obtained for decayed, missing or filled status of individual teeth or surface (Kappa values were 0.86 and 0.89, respectively; Table 5).
|

|
Child dental health status
A total of 7975 children were examined from 107 schools. There were 3923 male and 4052 female respondents. In the two key indicator age groups, there were 2095 in the 5–6-year-old group and 2418 respondents in the 11–12-year-old group. The mean ages of these groups were 6.1 years and 11.8 years respectively.
Five–six-year-old age group
The mean dmft for 5–6-year-olds was 1.53 and the mean decayed teeth (d) component was 1.1 (Table 1). Among 5–6-year-old children with untreated decay in their primary teeth (d > 0), mean dmft was 3.94 with an average of 2.8 decayed primary teeth. Table 1 shows that the mean dmft index varied widely between area health services. The levels of untreated decay (the d component of the index), showed similar area health service differences. North Coast, Greater Southern and Greater Western all recorded high levels of untreated decay: 1.9, 1.6 and 1.8, respectively.
These marked differences in mean dmft and d scores were also reflected in the proportions of children in the different area health services who were caries free. The proportions varied from 71.8% to 40.7%.
Eleven–twelve-year-old age group
The mean DMFT for 11–12-year-old children was 0.74 and the mean D value was 0.4 (Table 2). Among 11–12-year-old children with untreated decay in their permanent teeth (D > 0), mean DMFT was 2.13, with an average of 1.2 decayed permanent teeth. Again, large differences were found between area health service regions, with Hunter New England having the lowest mean DMFT score of 0.44 and North Coast having the highest at 1.07.
Table 2 also shows that the differences in untreated decay rates were considerable: 0.2 in Hunter New England and up to 0.7 in the North Coast. The overall proportion of 11–12-year-old children free from dental decay in their permanent teeth was 65.4%; however, these proportions varied from 54.8% to 75.9%.
The survey collected data on the presence of fissure sealants in each child. The proportion of children in the 11–12-year-old age group with at least one fissure sealant present in their permanent teeth was 17.9% statewide and varied from 33.7% in Northern Sydney Central Coast to 8.9% in Hunter New England (Table 2).
Subpopulation statistics for the whole sample
Four-hundred and fifty-eight Aboriginal children were surveyed, comprising 5.7% of the survey population This is higher than the statewide proportion of Aboriginal children in NSW (4.0%); however, any over-sampling was unintentional.8 These children had considerably higher dental disease experience than non-Aboriginal children in the survey (2.64 versus 1.54 dmft/DMFT; Table 3) and had on average twice as many decayed teeth (1.8 versus 0.9).
The Centrelink Concession Card holder status of children’s parents or guardians was collected in order to determine socioeconomic status. Data on children for 2807 Centrelink Health Care Card, Pensioner Concession Card and Commonwealth Seniors Health Card holders in NSW were collected in the survey. These children experienced substantially higher rates of dental disease than the remainder of the survey population (2.14 versus 1.34 dmft/DMFT; Table 3) and had on average twice as many decayed teeth (1.4 versus 0.7).
The survey identified 414 children in NSW (5.2% of the survey population) who required immediate treatment. Those that required immediate treatment had a mean dmft/DMFT rate of 5.11 and had 4.1 decayed teeth on average (Table 3). Only 3.6% of children requiring immediate treatment had never experienced decay.
In 2007, children living in fluoridated areas of NSW had lower mean dmft/DMFT rates than those living in non-fluoridated areas (1.56 versus 2.01; Table 3) and there were a higher proportion of children who had never experienced decay compared with children in non-fluoridated areas (52.7% versus 44%).
The mean dmft/DMFT rate by socioeconomic status was also compared using the SEIFA index of relative socioeconomic disadvantage, with the mean dmft/DMFT rate increasing from 1.09 in the highest socioeconomic status quintile to 2.02 in the lowest quintile (Table 3). Similarly, the mean number of decayed teeth increased from 0.5 in the highest quintile to 1.3 decayed teeth in the lowest quintile. The proportion of children aged 5 to 12 years with no caries experience decreased from 61.0% in the highest quintile to 44.3% in the lowest quintile.
Oral health status deteriorated with increased remoteness. In NSW in 2007, mean dmft/DMFT increased from 1.48 in the major cities to 2.27 in the remote and very remote areas (Table 3). The number of decayed teeth also increased with remoteness, from an average of 0.9 decayed teeth in the major cities to 1.4 in the remote and very remote areas. The proportion of children with no decay experience decreased with increasing remoteness, falling from a proportion of 53.9% in the major cities to 40.9% in the remote and very remote areas.
Discussion
The data from the survey provide an important snapshot of the oral health status of primary school-aged children in NSW. While statewide data show disease levels comparable to national rates, there are still large variations in NSW particularly in terms of remoteness, Aboriginality, access to water fluoridation and socioeconomic status.
The mean dmft in 5–6-year-old children in NSW is 1.53, which compares favourably to the national benchmark in 2001 of 1.89. Children aged 5–6 years in NSW had on average 1.1 primary teeth that were decayed. The mean dmft varied from 0.91 in South Eastern Sydney Illawarra to 2.75 in the North Coast and the mean number of decayed primary teeth varied from 0.5 in South Eastern Sydney Illawarra to 1.9 in the North Coast, reflecting both rural/urban differences in disease status as well as access to fluoridated water supplies.
The mean DMFT of 11–12-year-old children in NSW is 0.74, which compares favourably to the national benchmark in 2001 of 0.95. Children aged 11–12 years in NSW had, on average, 0.4 permanent teeth that were decayed. The mean DMFT varied from 0.44 in Hunter New England to 1.07 in the North Coast and the mean number of decayed permanent teeth varied from 0.2 in Hunter New England to 0.7 in the North Coast.
The high level of dental disease detected in Aboriginal children in this survey is consistent with the findings of previous child dental health surveys.9 In NSW, 16 Aboriginal Community Controlled Organisations provide dental services to local communities using a combination of Commonwealth and NSW Government funding. These services are often in rural and remote communities that do not have access to fluoridated water supplies.
The NSW Government, via the NSW Department of Health and the Centre for Oral Health Strategy, have implemented a range of programs to prevent dental decay in children and to identify disease early and intervene where appropriate. These programs include initiatives to encourage water supply authorities to introduce water fluoridation, the Early Childhood Oral Health Program and various oral health promotion initiatives.10 These health promotion activities are related to the priorities of both the State Health Plan and NSW State Plan with the latter describing the state oral health strategy as being ‘...to design and implement new models of care with a focus on prevention and early intervention’.11 The State Health Plan also includes the expansion of the ‘...availability of fluoridated water to the State’s population’ and the need for better oral health promotion programs’.12 In order to monitor the progress of these programs, surveys of child dental disease status will be required on an ongoing basis.
The use of pit and fissure sealants among children at high risk of dental caries has been proven to be a cost-effective intervention for public oral health services.13,14 This strategy is mandated by a NSW Health Policy Directive.15 NSW Health has developed draft targets in response to the finding of the Child Dental Health Survey 2007 that statewide only 17.9% of children aged 11–12 years had one or more fissure sealants present in their permanent teeth. It has been proposed that the target coverage should be 25% by 2012.
The Child Dental Health Survey 2007 has provided high quality data that encourages area health services to make the shift to an evidence-based population health approach and allows NSW Health to set targets for proven preventive strategies and to evaluate preventive programs. Area health services have further benefited through the development of local expertise in epidemiological survey methods and through having access to updated scanning and data processing technology at the state-level. The usefulness of the survey data has been enhanced by the timeliness of data processing, the analysis and release of which took approximately 8 months. The survey has established baseline data that will be comparable with data to be collected by the National Child Dental Health Survey planned for 2010 and 2011.
Conclusions
-
NSW Health has demonstrated that it is possible to undertake a statewide survey of school children’s dental disease status with a minimum of disruption to schools and to the ongoing provision of clinical oral health services.
-
Data from the Child Dental Health Survey 2007 provide solid evidence to support population oral health planning at both regional and state levels, and facilitate ongoing surveillance of populations of interest.
-
The rate of dental disease in Aboriginal children is a continuing cause for concern, being almost twice that of the NSW child population.
Acknowledgments
The authors gratefully acknowledge the assistance and expertise during the survey planning phase of Dr Clive Wright from the Centre for Oral Health Strategy and, from ARCPOH, Professor John Spencer, Dr Kaye Roberts-Thomson, Anne Ellershaw, Dr Loc Do and Dr Jason Armfield. The authors also acknowledge Dr Sandra Meihubers for conducting the calibration and reliability testing for NSW Health survey examination teams, Dr Alan Patterson for protocol development, the exam teams and co-ordinators for administering the survey and Sam Sterland and staff from the National Church Life Survey for retrofitting and scanning of the data forms to Teleform.
[1]
[2]
[3]
[4] Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull 1979; 86(2): 420–8.
| Crossref | GoogleScholarGoogle Scholar | PubMed | CAS | (Cited 20 February 2009.)
[8]
[9]
[10]
[11]
[12]
[13] Weintraub JA. Pit and fissure sealants in high-caries risk individuals. J Dent Educ 2001; 65(10): 1084–90.
| PubMed | CAS | (Cited 9 February 2009.)

