Communicable Diseases Report, NSW, July and August 2009
Communicable Diseases Branch, NSW Department of Health
NSW Public Health Bulletin 20(10) 166-171 https://doi.org/10.1071/NB09029
Published: 9 November 2009
Abstract
For updated information, including data and facts on specific diseases, visit www.health.nsw.gov.au and click on Public Health then Infectious Diseases, or access the site directly at: http://www.health.nsw.gov.au/publichealth/infectious/index.asp.
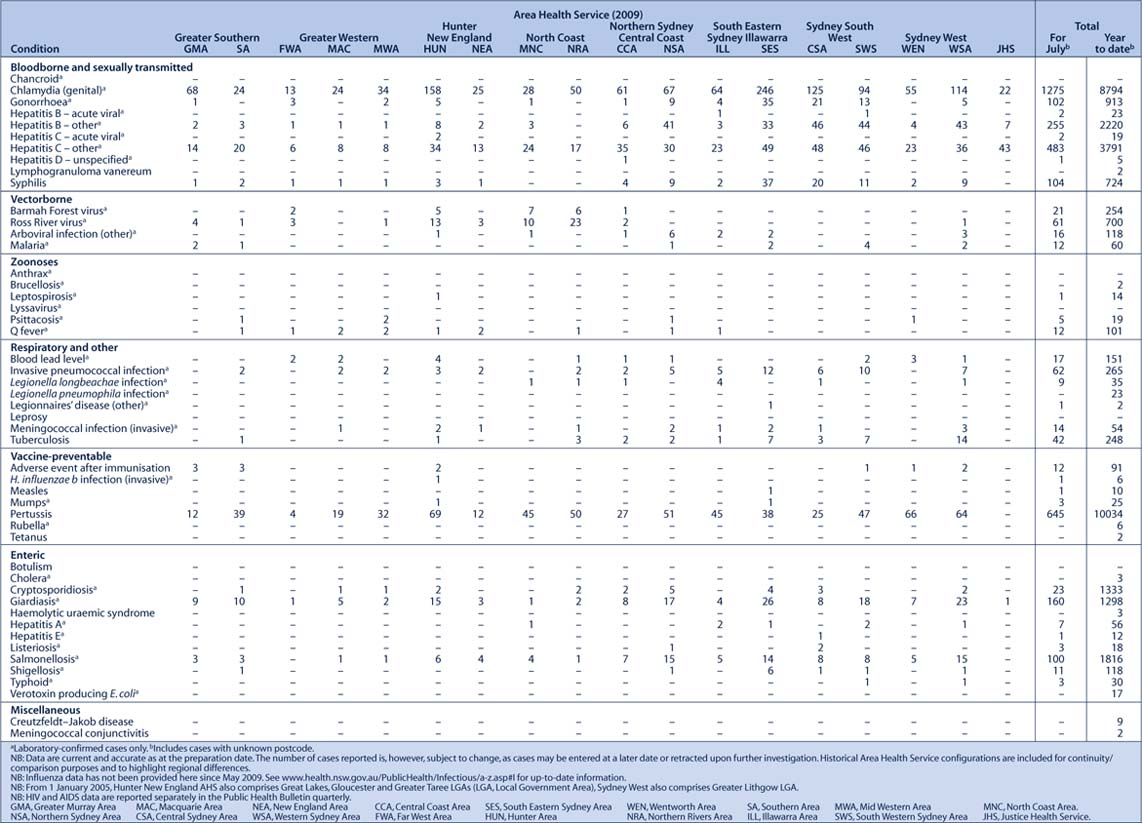
Figure 4 and Tables 2 and 3 show reports of communicable diseases received through to the end of August 2009 in New South Wales (NSW).
Invasive meningococcal disease
Twenty-seven cases of invasive meningococcal disease were reported in July and August in NSW, bringing the total number of cases to 68 so far this year. Two adult deaths were reported during July and August 2009. In comparison to August in 2008, there were 51 cases reported and one death.
There has been a downward trend in meningococcal notifications across all area health services in NSW since 2000. The highest numbers of notifications are reported among children aged less than 5 years at onset, with a second peak in the 15–24 year age group.
A vaccine against meningococcal C was added to the National Immunisation Program Schedule in January 2003. Consequently, serogroup C meningococcal disease is now mainly seen in adults and in unimmunised children. Serogroup B is the most common form of meningococcal disease in NSW. Of the 27 cases notified during July and August, 14 cases were due to serogroup B and two cases were due to serogroup C.
A media alert was released in August, reminding the public to be alert for the symptoms of meningococcal disease during winter and spring, the peak seasons for infection. An alert was also sent to GPs throughout NSW, highlighting the importance of early diagnosis and treatment of meningococcal disease.
Pertussis (whooping cough)
Monthly notifications of pertussis continue to decline steadily from the peak of the outbreak in December 2008. There were 1207 cases notified with onset in July and August, compared with 2082 in the preceding 2 months. The decrease was noted across all area health services in NSW. Comparison of data over time must be undertaken with caution however because of: recent changes in the use of diagnostic technologies (including the increasing use of nucleic acid testing); and changes in case ascertainment over time (related to increased awareness of the disease among doctors and the broader community).
The highest number of cases continue to be reported for children aged less than 15 years at onset, specifically children aged 0–4 and 5–9 years. Because pertussis immunity wanes over time, many older children and adults are susceptible to infection and can be the source of new infections in infants. Timely immunisation of infants is important because unvaccinated infants are at the highest risk of infection and of associated complications.
Since March 2009 and for a limited time in NSW, free pertussis (dTpa) vaccine has been available for: all new parents; couples who are planning a pregnancy; grandparents; and any other adults who will regularly care for infants aged less than 12 months. From March to August this year, 122 326 letters were sent to new parents in NSW, highlighting the pertussis outbreak and informing them of the availability of the free vaccine.
Measles
One case of measles was notified in July in NSW, bringing the total for the year to 10. This case was reported in an infant (too young for the Measles-Mumps-Rubella (MMR) vaccine) on their return from overseas travel. Thirty-nine cases of measles were notified in 2008. The majority of measles cases notified so far this year have been in young people recently returned from overseas travel, or in their contacts.
Many people born between 1966 and 1980 remain susceptible to measles because most people in this age group have not been exposed to measles infection and those who were routinely immunised typically received only one dose. Two doses are required to provide a high level of protection. Anyone born after 1965 should ensure that they have had two doses of MMR vaccine, unless they know they are immune.
Gastroenteritis in institutions
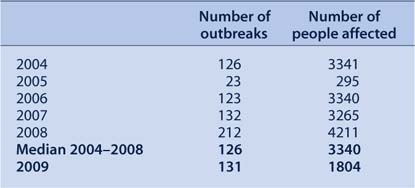
From 1 July 2004 to 31 August 2009, 747 outbreaks of gastrointestinal illness in institutions, affecting at least 16 256 people, were reported to NSW Health. Outbreaks of viral gastroenteritis are more commonly seen in winter months (Figure 1).
In 2009, between 1 July and 31 August, 131 outbreaks of gastrointestinal illness in institutions were reported, affecting 1804 people. This represents a small increase of 4% over the median number of outbreaks reported during the same time period from 2004 to 2008 (n = 126), and a significant decrease of 46% on the median number of people affected as a result of the outbreaks (n = 3340) (Table 1).
|
|

|
Twenty percent of the outbreaks were caused by norovirus, 4% by rotavirus, 1% by Clostridium difficile and Campylobacter respectively, and 75% were of unknown aetiology but were suspected to have been caused by person-to-person spread of a viral illness after investigating the epidemiological evidence and clinical symptoms of those affected. Fifty-five percent of the outbreaks occurred in aged-care facilities, 24% in hospitals, 20% in child-care centres, and 1% in a military facility.
Data collected on the number of presentations to emergency departments are consistent with the data shown in this report, with no increase in presentations during the time period 1 July–31 August 2009 when compared with data collected from the previous 5 years.
In children aged 0–4 years, presentations to emergency departments for gastrointestinal illness during the period July–August 2009 decreased when compared with earlier years (Figure 2).

|
This decrease may be due to the introduction of the rotavirus vaccination into the National Immunisation Program in July 2007. The Eastern Sydney Laboratory Surveillance Program, based at the South Eastern Sydney Illawarra Public Health Unit, shows a reduction in the number of cases of rotavirus (Figure 3).

|



