Tuberculosis in NSW, 2003–2007
Bridget A. O’Connor A , Lindy L. Fritsche A , Amanda J. Christensen A and Jeremy M. McAnulty ACommunicable Diseases Branch, NSW Department of Health
NSW Public Health Bulletin 20(4) 59-68 https://doi.org/10.1071/NB09001
Published: 27 April 2009
Tuberculosis (TB) has been a public health issue for a long time. ‘Since the first appearance of TB in humans probably some 8000 years ago, its control has continued to elude the brightest minds and challenge both the human and economic resources of countries around the world’.1 Towards the end of the nineteenth century antituberculosis campaigns began initially in Europe and North America.1 Some 100 years later, tuberculosis control remains a major priority for communicable disease surveillance, prevention and control in New South Wales (NSW).2
Despite having one of the lowest incidence rates of tuberculosis in the world (consistently around 5–6 cases per 100 000 population since the 1980s), tuberculosis control continues to be a challenge in Australia.3 Approximately 55% of the 9.1 million tuberculosis cases estimated globally in 2006 live in nearby South East-Asia and the Western Pacific Regions.4
Tuberculosis is caused by infection with the bacteria Mycobacterium tuberculosis.5 When people who are infectious cough, sneeze or talk, they expel tuberculosis germs, known as bacilli, into the air. A susceptible person only needs to inhale a small number of the bacilli to acquire the infection. Most people with the M. tuberculosis infection harbour the bacterium without symptoms (latent infection), but some develop active tuberculosis. People who have newly acquired the infection have about a 10% chance of developing active disease in their lifetime; approximately half of those who develop tuberculosis do so within 2 years of infection.6
The usual incubation period from infection to demonstrable primary lesion or significant tuberculin reaction is 2–10 weeks.6 Most people with active tuberculosis are no longer infectious after they have received 2 weeks of treatment with appropriate multi-drug therapy.
In this report we review the incidence of tuberculosis and the characteristics of patients notified with tuberculosis in NSW for the period 2003–2007.
Methods
Tuberculosis is a notifiable disease in NSW under the NSW Public Health Act 1991; laboratories, doctors and hospitals must report all cases to their local public health unit. Public health unit or chest clinic staff enter case details into the Notifiable Diseases Database (NDD), which is maintained by the Communicable Diseases Branch of the NSW Department of Health. Cases were assigned to their corresponding year of notification using a specific tuberculosis field in NDD called year of diagnosis. This field was added to NDD in 2004 to assist the assignment of cases where dates of onset, specimen collected, notification and treatment overlap years. Cases in 2003 and earlier were assigned to their corresponding year if their date of onset, date of report or date of notification fell between 1 January and 31 December of the relevant year.
We analysed the characteristics of cases for the period 2003–2007 and examined trends in incidence since 1991. Incidence rates were calculated using the Australian Bureau of Statistics (ABS) estimated mid-year population for the relevant year. Estimates for different resident populations by country of birth were provided by the Health Outcomes Information Statistical Toolkit (HOIST) and were calculated from a number of ABS datasets.7
Pulmonary cases were defined as patients whose primary site of tuberculosis disease was the lung (either with or without involvement of other sites). Reactivated cases were defined as patients who had previously received a full or partial course of drug therapy followed by a new episode of disease.
Multi-drug resistant tuberculosis (MDR-TB) was defined as resistance to at least isoniazid and rifampicin, two antibiotics commonly used to treat the disease. Extreme drug resistant tuberculosis (XDR-TB) was defined as resistance to almost all drugs used to treat tuberculosis, including isoniazid, rifampicin, fluoroquinolones and at least one of three injectable drugs (i.e. amikacin, kanamycin or capreomycin).
Assessable outcomes of tuberculosis cases are those that are measurable within the NSW Tuberculosis Program as well as cases transferred interstate. Non-assessable outcomes are defined as those where cases have transferred overseas or their outcome could not be measured for other reasons.
High-burden countries were defined according to the World Health Organization (WHO) Global Tuberculosis Control 2008 – Surveillance, Planning, Financing report.4
Results
Note that within NSW Health, the term ‘Aboriginal’ is generally used in preference to ‘Aboriginal and Torres Strait Islander’, in recognition that Aboriginal people are the original inhabitants of NSW.
Case notifications
From 2003 to 2007, between 373 and 465 cases of tuberculosis were notified each year in NSW (median 437 cases). The rate of notifications ranged from 5.6 cases per 100 000 population in 2003 to 6.8 cases per 100 000 population in 2006 (average notification rate during the period was 6.3 cases per 100 000 population). The rate of tuberculosis in NSW remained relatively stable from 1991 through to 2007 (Table 1).

|
Demographic characteristics
From 2003 to 2007, the incidence of tuberculosis was higher among people living in the Sydney metropolitan area than in other areas of NSW (Table 2). This finding is consistent with data from 1991 to 2002.8

|
The incidence of disease was similar for males and females in the period 2003–2007 but varied according to age (Table 2). There was a bimodal distribution for age at onset; rates peaked in those aged 25–34 years and in those 75 years and older. This pattern is similar to the age distribution for the period 1991–2002.8 During 2003–2007, infants and preschool-aged children had a higher rate of disease than school-aged children.
Aboriginal Australians accounted for less than 1% of cases in NSW, with two to four cases reported each year during 2003–2007 (Table 2).
During 2003–2007 more than 85% of tuberculosis cases were born overseas, and over 60% were from Asia (Table 3). Over the 5-year period, there was an increase in the rate of tuberculosis among people born in Southern and Central Asia while rates in other areas of Asia remained steady (Figure 1). The rate of tuberculosis among people born in Australia continues to remain around one case per 100 000 population.

|

|
Site of infection
The main site of disease from 2003 to 2007 was the lung (58–61% of cases) (Table 4). The second most reported site for all years was lymphatic tissue (17–22% of cases).

|
Case classification
From 2003–2007, 94–97% of cases were notifications of newly diagnosed disease, and 3–6% were reactivated cases (Table 4). Of the reactivated cases, 74% had tuberculosis following treatment overseas and 26% had tuberculosis following treatment in Australia.
Laboratory confirmation
Over 70% of cases during 2003–2007 were laboratory confirmed, with either M. tuberculosis identified by culture, nucleic acid amplification tests or both (Table 4).
During this time, sputum microscopy and culture results were reported for over 90% of cases with pulmonary disease. Of these, around 40% had acid-fast bacilli identified on direct sputum smears, and around 75% were reported to have M. tuberculosis cultured in the sputum.
Clinical outcomes
Based on assessable outcomes from 2003 to 2007, 96–98% of cases completed treatment or were classified as cured (culture negative at completion of treatment) (Table 5). From 2003 to 2007, between 17 and 25 cases died each year; of these, tuberculosis was reported as the cause of death in one to five cases per year (Table 5).

|
HIV co-infection
The rate of human immunodeficiency virus (HIV) testing of tuberculosis cases improved during 2003–2007, but remains low. In 2003, 68 cases (18%) were tested for HIV infection, increasing to 193 cases (43%) tested in 2007 (Figure 2).8 Overall the proportion of cases with tuberculosis-HIV co-infection ranged from 1–3% during the period.

|
Drug resistance
Overall, 15 (0.7%) of the 2161 tuberculosis cases reported in NSW during 2003–2007 were multi-drug resistant, compared to 25 (0.5%) of 5042 cases reported during 1999–2002.8 One MDR-TB case (in 2005) had tuberculosis-HIV co-infection. Over the period 1999–2007, 40 cases of MDR-TB were identified, representing 1% of tuberculosis notifications.
During 2003–2007, nine (60%) cases with MDR-TB were aged 20–35 years and 11 (73%) were male. Of the 15 cases, 13 (87%) were born overseas; six in Southern and Central Asia, four in South East Asia, two in Africa and one in the Pacific Islands. Of the two Australian-born cases, one had resided in a high-burden country and one had co-existing immunosuppression.
Eleven (73%) of the MDR-TB cases presented with pulmonary disease and 10 (67%) were smear positive. Ten (67%) cases reported no previous treatment, indicating the infection was likely to be a primary infection with MDR-TB rather than a newly resistant infection. Of five cases who acquired resistance following previous treatment, four had been treated overseas and one had been treated in Australia. One case of XDR-TB was retrospectively identified in a person who was notified in 2002 using the revised case definition issued by WHO in 2007.9 This person was born in Fiji. They presented with extrapulmonary tuberculosis and reported no past history of tuberculosis. There was a family history of tuberculosis overseas three decades before diagnosis. The case was successfully treated with second-line drugs.
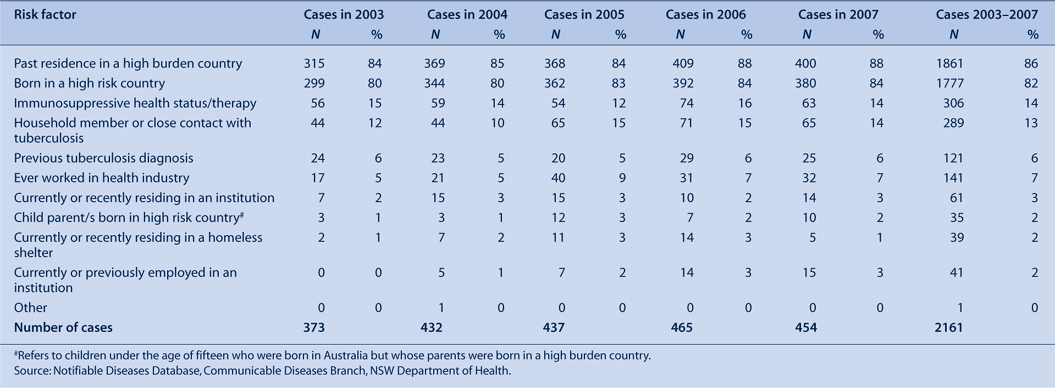
Risk factors
From 2003 to 2007, the most commonly reported risk factors for tuberculosis were: past residence in a high-burden country (83–88%); birth in a high-burden country (80–84%) (Table 6). During 2003–2007, the reported risk surrounding healthcare workers and transmission of tuberculosis has not changed significantly over time (Table 7). The annual proportion of cases that report having ever worked in a healthcare facility (in Australia or overseas) was 5–9%, with most of these cases (4–7%) being born overseas. Cases reported as currently or recently employed as healthcare workers (at time of diagnosis) constitute 3–6% of tuberculosis cases during 2003–2007.
|

|
Performance indicators
In 2002, the National Tuberculosis Advisory Committee developed national performance indicators for tuberculosis.10 Table 8 presents the performance criteria and the NSW and Australian data for each indicator for 2003–2007.

|
Between 2004 and 2006, the indicator of less than 0.1 cases per 100 000 population in children aged less than 15 years was reached in NSW for Aboriginal children. The incidence of tuberculosis in Aboriginal Australians and non-Aboriginal Australian-born children are higher than the expected performance criteria Australia-wide and in NSW. Overall the NSW rate of infection in Aboriginal Australians represents three to four cases per year. No Aboriginal children in NSW have been notified with tuberculosis since 2003 when two children were reported. Four to nine cases were notified per year in non-Aboriginal Australian-born children. The majority of these children report having parents born in high-burden countries as well as other risk factors such as being a household contact of a tuberculosis case.
The crude incidence in NSW in Aboriginal Australians and non-Aboriginal Australian-born people is similar to or less than the combined rate for all Australian states and territories. However, the crude incidence of tuberculosis cases born overseas was higher in NSW compared to the incidence in other jurisdictions. Compared to the Australian data, the proportion of cases with a recorded HIV status is lower in NSW.
Discussion
Tuberculosis in NSW continues to affect people who were born in countries with a high prevalence, with rates peaking in the 25–34 year age group and a secondary peak in the 75 and older age group. The highest incidence was among people living in the Sydney metropolitan area, reflecting migration settlement patterns as most people from high-burden countries initially settle in metropolitan areas.11
The success of the NSW Tuberculosis Program can be seen in the incidence of tuberculosis in NSW remaining steady over the last decade despite large-scale migration from high-burden countries.4 Other successes of the Program are reflected in the high treatment success rates, absence of treatment failures and low rates of relapse of cases initially treated in Australia. The incidence of tuberculosis among Australian-born people is also low and may reflect the low risk of exposure in this population. Contact tracing programs and preventive therapy, occupational screening of healthcare workers as well as improvements in the health of the general population are also likely to be contributing to the low rate of tuberculosis among Australian-born people.8
Although overall rates of tuberculosis are low in NSW, there are still a number of performance indicators that have not reached expected outcomes. NSW reports higher rates of tuberculosis in people born overseas than in people born in Australia, which may reflect migration patterns within Australian states and territories.12
Since 2004, only 30–40% of tuberculosis cases in NSW were tested for HIV infection each year. The low rate of testing could be due to the reluctance of treating doctors to request the test or they may be unable to identify any risk factors for HIV infection and therefore are not testing. Risk factor assessment (in a study reviewed from North America) does not reliably predict HIV infection in tuberculosis patients.13 Recommendations have been made that all persons with tuberculosis should be routinely offered HIV testing.13 Improved compliance with HIV testing is needed to meet the national performance indicator of 100% of cases assessed for HIV status. NSW Department of Health is currently reviewing policies to improve the proportion of tuberculosis cases who are offered HIV testing and the proportion of positive HIV cases who are offered assessment for tuberculosis co-infection.
MDR-TB is an ever present threat to tuberculosis control in Australia. Treatment of MDR-TB and XDR-TB is more complex, requires a longer treatment time and is often associated with a poorer outcome for the patient. Although numbers of MDR-TB cases in NSW are steady, NSW is seeing an increase in rates of tuberculosis from regions with a high incidence of MDR and XDR-TB. Continued prevention and control of surveillance of tuberculosis and, in particular, resistant strains is necessary in NSW.
Nationally, an increase in the number of tuberculosis notifications in healthcare workers has been reported, especially among people born overseas.3 Although NSW has seen a slight increase in cases who are healthcare workers during 2003–2007, the proportion born overseas has not changed. The risk of transmission in the healthcare setting is currently low although ongoing surveillance is required.
This report indicates that the incidence of tuberculosis in NSW has remained stable over recent years. Tuberculosis remains a disease that mostly affects people born in countries of high prevalence with little evidence of local transmission. The threats to the NSW Tuberculosis Program are similar to those that challenge tuberculosis control globally and include control of MDR-TB and XDR-TB, and identification and management of tuberculosis-HIV co-infection. To continue the success of the Program, it is important to maintain effective collaboration with key stakeholders across clinical, public health and community sectors.
Acknowledgments
We acknowledge the important role of staff of the chest clinics, public health units, laboratories, doctors and Communicable Diseases Branch of NSW Department of Health in collecting and reporting data on tuberculosis cases in NSW. In particular, we acknowledge Peter Jelfs and Vitali Sintchenko from the Institute of Clinical Pathology and Medical Research for reviewing the drug resistance data.
[1]
[2] McAnulty J, Stewart K. NSW Public Health Network. Priorities for communicable disease control in New South Wales, 2003. N S W Public Health Bull 2003; 14(9–10): 200–5.
| Crossref | GoogleScholarGoogle Scholar | PubMed | (Cited 27 February 2009.)
[8] O’Connor B, Christensen A, McAnulty J. EpiReview: tuberculosis in New South Wales, 1991-2002. N S W Public Health Bull 2004; 15(7–8): 138–43.
| PubMed | (Cited 24 February 2009.)
[10]
[11]
[12]
[13] Emerson CR, Post JJ. To routinely offer testing for HIV infection in all cases of tuberculosis: a rational clinical approach? Med J Aust 2008; 188(3): 162–3.
| PubMed |


