Another opportunity for prevention: assessing alcohol use by women attending breast screening services in Lismore, NSW
Michelle D. Daly A C , Megan E. Passey B and Amanda J. Harvey AA North Coast Area Health Service
B Department of Rural Health (Northern Rivers), School of Public Health, University of Sydney
C Corresponding author: Email: Michelle.Daly@ncahs.health.nsw.gov.au
NSW Public Health Bulletin 20(6) 90-92 https://doi.org/10.1071/NB07121
Published: 24 June 2009
Abstract
Substantial epidemiological evidence supports the association between alcohol consumption and the risk of breast cancer; however, information on alcohol consumption is not routinely collected by breast screening services in NSW. This study was conducted to investigate the level of self-reported alcohol use among women accessing North Coast BreastScreen in Lismore, NSW. Two hundred and sixty-four consecutive women were screened using the Alcohol Use Disorders Identification Test. Their drinking status was categorised as low risk, risky or high risk. Two-thirds of the screened women (69.7%) were classified as low-risk drinkers; 9.8% as risky and 0.4% as high-risk drinkers. Although the risk of breast cancer increases with the amount of alcohol consumed, evidence suggests that even low-risk drinking is associated with increased risk of breast cancer. Implications for prevention activities by breast screening services are discussed.
As part of its routine program, BreastScreen New South Wales (NSW) assesses women for breast cancer risk factors. Alcohol use is not currently assessed in any BreastScreen NSW service, despite substantial evidence supporting the association between alcohol consumption and the risk of breast cancer.1–4 Consumption of 30 g of alcohol each day (three standard drinks) is associated with a similar level of risk to other recognised risk factors for breast cancer, such as young age at menarche and family history; however, alcohol consumption is one of the few risks that is modifiable.2
The current National Health and Medical Research Council (NHMRC) guidelines note that alcohol increases women’s risk of breast cancer and the risk increases with the level of alcohol used. Compared with women who drink little or no alcohol, the risk of breast cancer is 35% higher in women who drink three to four standard drinks a day and 67% with more than four drinks a day. Even low level drinking is associated with some increase in risk.4
The 2004 National Drug Strategy Household Survey found that just over half (58.1%) of women aged 60 years or more approved of regular (i.e. daily or nearly every day) alcohol use. Approval for regular drinking in younger age groups was higher, with 74.7% of 40–49-year-old women and 69% of 50–59-year-old women approving of regular drinking. The survey also showed that in the Australian adult female population, 9.6% used alcohol at a level considered to be risky or high risk for long-term harm from a range of chronic physical and psychological illnesses.5
BreastScreen services are free to eligible women and the uptake is high, with 63.5% of women aged 45–54 years, 80.9% of women aged 55–64; and 84.2% of 65–74-year-old women reporting having received a screening mammogram in the previous 2 years.6 For the North Coast region of NSW, the corresponding figures are 73.1%, 81.9% and 80.5% respectively.6 We conducted a study to assess the level of self-reported alcohol use among women accessing North Coast BreastScreen.
Methods
The receptionist or a women’s health nurse invited consecutive women attending North Coast BreastScreen in Lismore NSW to participate in a study. They were informed that the purpose of the study was a survey on alcohol use. Those providing written informed consent were asked to complete a brief anonymous questionnaire that included the Alcohol Use Disorders Identification Test (AUDIT) assessment tool and basic demographic information.
The AUDIT is a brief 10-item screening instrument developed by the World Health Organization for detecting risky and high-risk levels of drinking.7 It has been used widely and validated as a screening tool in more than 16 studies, including Australian studies.7–11 It uses three domains: alcohol intake; dependence; and problems associated with drinking. Based on the scores, it classifies respondents’ alcohol use into three drinking risk levels: low risk (includes non-drinkers), risky and high risk. For women, low-risk drinking is classified as scoring 0–5 on the AUDIT; risky drinking is a score of 6–12; and high-risk drinking is a score of 13 or more.7
Data were collected one day per week over three consecutive months in 2006. Women were given information on the study and, if willing to participate, were asked to provide consent. Participants were given written instructions on how to complete and self-score the survey. They were also given written feedback on their AUDIT score, options for interventions and other relevant information. All women were able to complete the AUDIT while waiting to have their mammogram, without assistance from the researchers. No women asked to speak with a clinician to discuss their drinking risk level. Women were instructed to separate their consent form and AUDIT and place them in two separate envelopes to ensure anonymity.
Data were entered onto a specifically designed database. Based on the AUDIT score, women were categorised as non-drinkers, low-risk drinkers, risky or high-risk drinkers.
Ethical approval for the study was obtained from the North Coast Area Health Service Human Research Ethics Committee.
Results
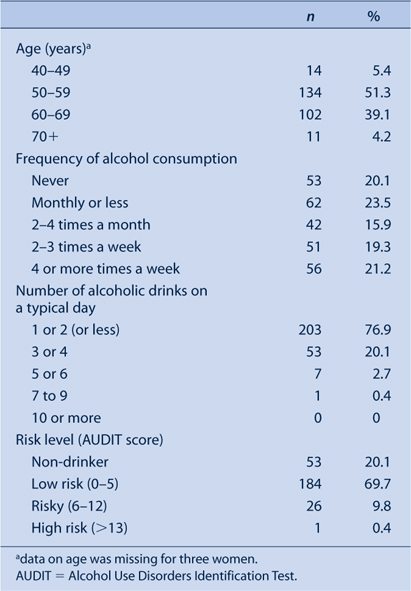
Two hundred and sixty-four women completed the AUDIT questionnaire. No women declined to participate. Fifty-three women (20.1%) were classified as non-drinkers, 184 (69.7%) as low-risk drinkers, 26 (9.8%) as risky drinkers and one (0.4%) as a high-risk drinker (Table 1). All but four of the women classified as risky or high-risk drinkers drank alcohol at least two to three times per week, with 12 reporting drinking four or more times per week. Nearly a quarter of the women reported drinking at least three or four drinks on a typical day when they were drinking.
|
Discussion
In this study, we found that 10.2% of women attending North Coast BreastScreen reported risky or high-risk drinking, when screened using the AUDIT. This is lower than the rates reported for the NSW Population Health Survey (2006).6 However, the definitions of risky drinking used in the two studies are different. We used the AUDIT, which has been widely validated for use as a screening tool in clinical settings, with the intention of providing interventions for those identified as drinking at risky levels. By contrast, the NSW Population Health Survey uses a definition appropriate for population surveys and defines risky drinking for women as one of the following: drinking alcohol on a daily basis; drinking on average more than two standard drinks per day; or drinking more than four standard drinks on any one day. High-risk drinking was determined as drinking seven or more standard drinks on any one day as per NHMRC Australian Alcohol Guidelines.4 With the AUDIT, women drinking every day but at low levels would not be classified as risky drinkers. Thus use of the drinking levels defined in AUDIT results in a more conservative estimate of the prevalence of risky drinking.
The prevalence of risky drinking is consistent with the level of acceptability of alcohol use reported in the 2004 National Drug Strategy Household Survey.5 This result may reflect a lack of awareness of the association between alcohol use and breast cancer. The Breast Health Survey found that 31.1% of women considered there was no increased risk of breast cancer associated with alcohol consumption.12
Given the prevalence of risky drinking among women in the breast screening age group, and that alcohol consumption is a modifiable risk factor for breast cancer, it would be beneficial for primary health-care services such as BreastScreen to implement routine screening and early intervention. Completion of the AUDIT screening tool without any clinician feedback has itself been shown to be an effective brief intervention and is therefore more beneficial than merely providing women with information on the risks associated with alcohol use and breast cancer.13 Completion of the AUDIT encourages women to reflect on their drinking level. The NSW Health clinical guidelines for nursing and midwifery practice in NSW support a self-help model of intervention when staff lack time to provide a more intensive intervention.14 The guidelines add that self-help approaches are effective with women who drink at mild and moderate levels. However, it would be beneficial to conduct further research on the effectiveness of this approach in the BreastScreen setting.
In our study, we were able to incorporate the use of the AUDIT into the daily screening procedures of North Coast BreastScreen, with no women refusing to participate. Women were given information on how to complete and self-score the survey, feedback on their score and options for interventions, including contact details for drug and alcohol services. As BreastScreen has the mandate to screen all women aged 50–70 years for breast cancer, the service routinely sees the majority of women in this age group. Screening and provision of feedback in a manner similar to that used in this study by all NSW BreastScreen services would be an inexpensive mechanism for identifying women at risk and alerting women to the risks associated with alcohol consumption. Delivering this intervention would also support the role of general practitioners who provide early interventions in primary care.
The NHMRC recently released new draft guidelines for safe alcohol consumption, which suggested reducing the level of alcohol consumption that is considered safe. These new guidelines reinforce the argument for incorporating screening for alcohol use, with provision of suitable interventions, into the routine procedures of BreastScreen services.
Acknowledgments
We would like to thank the staff of Lismore BreastScreen Services and the women who participated in the study.
[1] Singletary K, Gapstur S. Alcohol and breast cancer: review of epidemiologic and experimental evidence and potential mechanisms. JAMA 2001; 286(17): 2143–51.
| Crossref | GoogleScholarGoogle Scholar | PubMed | CAS | (Cited 20 March 2009.)
[4]
[5]
[6]
[7] Saunders JB, Aasland OG, Babor TF, De La Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption. Addiction 1993; 88 791–804.
| Crossref | GoogleScholarGoogle Scholar | PubMed | CAS |

[8] Saunders JB, Aasland OG, Amundsen A, Grant M. Alcohol consumption and related problems among primary health care patients. WHO collaborative project on early detection of persons with harmful alcohol consumption. Addiction 1993; 88 349–62.
| Crossref | GoogleScholarGoogle Scholar | PubMed | CAS |

[9] WHO Brief Interventions Study Group A cross-national trial of brief interventions with heavy drinkers. Am J Public Health 1996; 86 949–55.

[10] Conigrave KM, Hall W, Saunders JB. The AUDIT questionnaire: choosing a cut-off score. Addiction 1995; 90 1349–56.
| Crossref | GoogleScholarGoogle Scholar | PubMed | CAS |

[11] Conigrave KM, Saunders JB, Reznik RB. Predictive capacity of the AUDIT questionnaire for alcohol-related harm. Addiction 1995; 90 1479–85.
| Crossref | GoogleScholarGoogle Scholar | PubMed | CAS |

[12]
[13] Babor TF, Grant M. A randomized clinical trial of brief interventions in primary health care: summary of WHO project. Addiction 1994; 89 657–60.
| Crossref | GoogleScholarGoogle Scholar | PubMed | CAS |

[14]

