Mapping community-based youth mental health services in Tasmania, Australia
Melissa Savaglio A , Marie Yap B C , Ash Vincent D and Helen Skouteris A E *A
B
C
D
E
Abstract
Tasmania has the most rurally and remotely dispersed population of young people in Australia with high rates of youth experiencing mental ill health and socioeconomic disadvantage. Standard descriptions of mental healthcare provision are necessary for evidence-informed mental healthcare policy, planning and implementation. This systematic scoping study aimed to: (1) map and describe the characteristics of community-based youth mental health services (including substance-use) for young people in Tasmania, Australia and (2) identify gaps in service accessibility and provision.
A list of eligible services was developed through a systematic search and consultation with key stakeholders. Data were collected from a representative from each eligible service via an interview or online survey. A standardised framework was used to classify, describe and map services. Thematic analysis was used to analyse service providers’ perceived gaps to service access and provision.
Twenty-eight community-based mental health services for youth were identified, predominantly located in the major city of Tasmania’s three service regions. Service gaps include the ‘missing middle’, lack of integrated supports and limited service capacity.
The findings highlight the limited availability, accessibility and capacity of youth mental health services across Tasmania. Recommendations focus on increasing accessibility of rural/regional supports, provision of assertive outreach, psychosocial support, integrated care and strengthening the rural mental health workforce. These findings may inform the (re)design/(re)development of community-based youth mental health services in Tasmania. The findings may also guide evidence-informed mental health service planning, decision-making, development and implementation of integrated models of youth mental health care across Australia.
Keywords: Australia, community-based support, community services, mental illness, qualitative, rural health, service mapping, Tasmania, youth mental health.
Introduction
Young people (aged under 25 years) experience the highest rates of mental health concerns than any other age group (ABS 2022). This is concerning given the adverse personal, community, societal, economic and intergenerational consequences of mental health concerns among youth. Mental illness is one of the leading causes of burden of disease among youth in Australia; suicide is the leading cause of death (AIHW 2021). In Tasmania, the percentage of young people experiencing a mental health concern has significantly increased from 10.6% in 2012 to 18.8% in 2018 (ABS 2018). Tasmania’s rate of youth suicide is higher than the national average (ABS 2022). Given that the onset of approximately 50% of mental disorders often occur before age 25 (Caspi et al. 2020), enhancing youth mental health services must remain a priority.
Community-based mental health services support young people globally; the sector is considered an affordable and accessible model of mental health care. As with mental health systems worldwide, it is recognised that Tasmania’s community service system for supporting young people is severely fragmented (CCYP 2018; PHT 2020; MHC 2021). Key reform priority areas of the Tasmanian Government’s Rethink Mental Health 2020–2025 plan to integrate community mental health services and improve support for people experiencing mental illness include: (1) providing access to support early in life and early in illness; (2) an integrated mental health system; (3) shifting the focus from hospital-based care to support in the community; (4) supporting and developing the workforce; and (5) responding to the needs of young people (PHT 2020). Following independent review, the state-wide Child and Adolescent Mental Health Service (CAMHS) has undergone reform to provide more specialist support for youth with the most severe, complex and acute needs (Department of Health 2020). Despite strong local community support, there have been no other reviews or royal commissions of Tasmania’s youth mental health system.
The standard description of local care provision is essential for evidence-informed mental healthcare policy, planning and implementation (Salvador-Carulla et al. 2013). Service mapping involves providing a detailed description of local socio-demographic characteristics and the local service provision (Romero-López-Alberca et al. 2019). A standardised classification system is used for coding local services to facilitate comparisons between services and service providers (Salvador-Carulla et al. 2013). Service mapping assists in showing patterns of care delivery and identifying gaps in service availability. Formal service mapping for mental health care has been conducted across various areas in Australia (Bell et al. 2018; van Spijker et al. 2019; Salvador-Carulla et al. 2022). As highlighted in the Rethink 2020–2025 mental health plan (PHT 2020), mental health service mapping for Tasmania was conducted in 2019–2020, commissioned by the Department of Health and Primary Health Tasmania (Gossip et al. 2023). However, there was no discussion or specification of availability of community-managed services specifically targeted for children and young people. Australia-wide, there has been limited focus on state-wide mapping of mental healthcare services specifically for youth, having only been conducted in the Australian Capital Territory (ACT) to date (Furst et al. 2021). This is a significant gap that requires attention to accurately shape and inform local mental health policy and service planning.
Tasmanian mental health stakeholders acknowledge that the community-based mental health services for youth are currently insufficient (CCYP 2018; PHT 2020; MHC 2021), yet no systematic service mapping of the youth community mental health sector has been published. Standardised classification and documentation of the local landscape is warranted to identify key gaps in youth mental health service provision to inform future service planning, adapt current services or design new services. Therefore, this service scoping study aims to: (1) map and describe the characteristics of community-based mental health services available for young people (aged under 25 years) in Tasmania and (2) identify key gaps in service accessibility and provision. It is intended that this data will be used to guide evidence-informed youth mental health service planning and decision-making across the state.
Method
Study setting
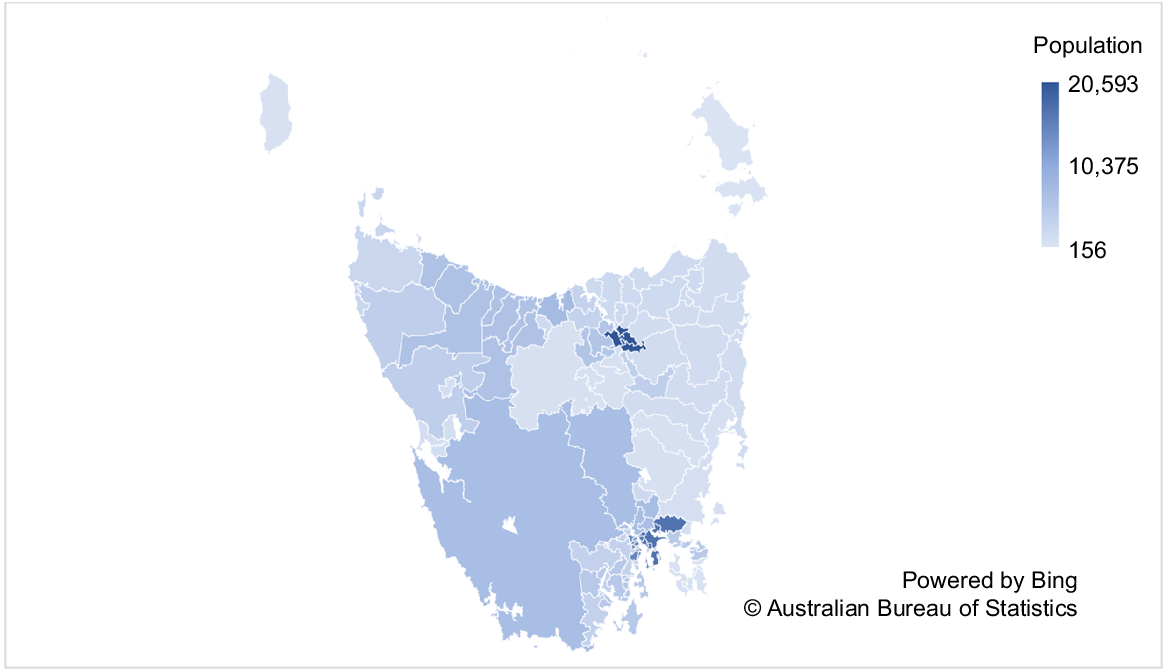
Service mapping was conducted for Tasmania; the third smallest state/territory in Australia with a population of 571,873 (Tasmanian Government 2023) and population density of 8.36 people per square kilometre (State Growth Tasmania 2022). A quarter (27%) of Tasmania’s population are aged 0–24 years, with 20% aged <18 years, compared to the Australian population of young people at 30% and 22%, respectively (State Growth Tasmania 2022). Tasmania has 29 local government areas (LGAs) that cover three service catchments/regions – South (including Hobart, the capital city), North (including Launceston) and North-West (including Devonport and Burnie). The proportion of young people living across these three regions is approximately 50.8%, 27.6% and 21.7%, respectively (State Growth Tasmania 2022). Tasmania has the most rurally and remotely dispersed population in Australia, with 32% of young people living outside the four major LGAs of Hobart, Launceston, Devonport and Burnie (State Growth Tasmania 2022). Fig. 1 presents the population density of young people in Tasmania. The Index of Relative Socio-economic Disadvantage indicates that Tasmania has the highest proportion of children living in the most socio-economically disadvantaged areas (CCYP 2018). Approximately 68% of young people in Tasmania live in LGAs of greatest disadvantage; half of these children live in the North and North-West, which are considered the most socioeconomically disadvantaged regions in the country (CCYP 2018).
Service inclusion and exclusion criteria
Community-based mental health services for young people in Tasmania were identified. Services were included in the current study if they: (1) were described as a support service for children, adolescents or young people with mental illness/experiencing mental health concerns, including substance misuse; (2) specifically supported young people under 25 years of age; (3) were delivered in the community, rather than hospital-based/inpatient services; and (4) were located in Tasmania. Services were excluded if they: (1) only supported people over the age of 18, as this was considered an adult service; (2) provided generic support for the general population, not specifically for children and adolescents (e.g. GPs); and (3) were delivered within the private sector (i.e. private psychologists) or acute sector (i.e. hospital-based, inpatient care).
Search strategy
An advisory group of Tasmanian youth mental health stakeholders (n = 16) was involved in the study’s design, data collection and analysis. Stakeholders included local mental health sector and peak body representatives (n = 2), government representatives (Department of Health, n = 2), service providers/clinicians (n = 6), young people with lived experience of mental illness (n = 3) and parents/carers (n = 3). The service search was conducted in June 2022. A workshop was held with the advisory group to discuss stakeholders’ awareness and knowledge of existing eligible services, and generated a list of all service providers across the state. Informed by stakeholder consultation, an online search of service provider websites, Primary Health Tasmania website, FindHelpTas and the Strong Families Safe Kids service directory (i.e. state-wide resource for providers/practitioners to locate child wellbeing services) was conducted to identify potentially eligible services.
Data collection
Data collection was conducted throughout July–October 2022. Eligible services were contacted via email or phone. Services nominated a representative (e.g. CEO, clinician, etc.) to participate. Service data were collected via an online survey or a telephone/Zoom interview with each service representative, depending on their personal preference, capacity and availability. The same questions were used for the interview schedule and survey to ensure consistency (see Supplementary Table S1). Interviews were 30 min in duration; surveys took approximately 16 min to complete. Data collected from service representatives were verified against any publicly available information found online. Service representatives were asked about service accessibility (i.e. location, capacity, cost, funder, opening hours, referral process), characteristics of the service target population (e.g. age range, severity, eligibility criteria) and components of service delivery (e.g. mode of delivery, type of support provided, staffing, service intensity/duration). Representatives were also asked to identify any perceived gaps to service access and provision. Examples of key questions are: What are the barriers to accessing your service? and What are the challenges to delivering your service? Two identified services did not respond and were therefore not included in the qualitative component of the study regarding perceived service gaps. Service characteristic information was gained from publicly available data.
Data analysis
The Description and Evaluation of Services and DirectoriEs for Long Term Care (DESDE-LTC) tool was used to classify the identified services (Romero-López-Alberca et al. 2019). The DESDE is a well-established standardised classification system to code and describe health services, which has been widely used for mental health service mapping in Australia and internationally (Romero-López-Alberca et al. 2019; Salvador-Carulla et al. 2022). Each service was allocated a DESDE code, which comprises three core components, as shown in Supplementary Table S2: (1) client age group; (2) client eligibility/diagnostic group; and (3) type of care provided. The typology of care was outpatient community-based mental health services. Data collection aligned with this tool. Service characteristics were tabulated and described in-text. To visually demonstrate service accessibility, the location of services were mapped.
Thematic analysis was used to analyse representatives’ qualitative responses to the open-ended questions regarding perceived service gaps and barriers to service access/provision. Analysis was guided by Braun and Clarke’s (2006) six-phase approach to coding and theme development, and qualitative reporting aligned with the Consolidated Criteria for Qualitative Research checklist (Tong et al. 2007). Data coding was inductive and semantic. Data were double-coded to ensure inter-rater reliability. Related/homogenous codes were grouped together to form three themes, reflecting three key gaps in service provision.
Results
Service characteristics
Supplementary Table S3 presents a summary of service characteristics and the classification of services according to DESDE-LTC codes. Twenty-eight community-based mental health services were identified, delivered by 22 service providers. The services were delivered at 46 locations across the state. Sixteen services were available in more than one location.
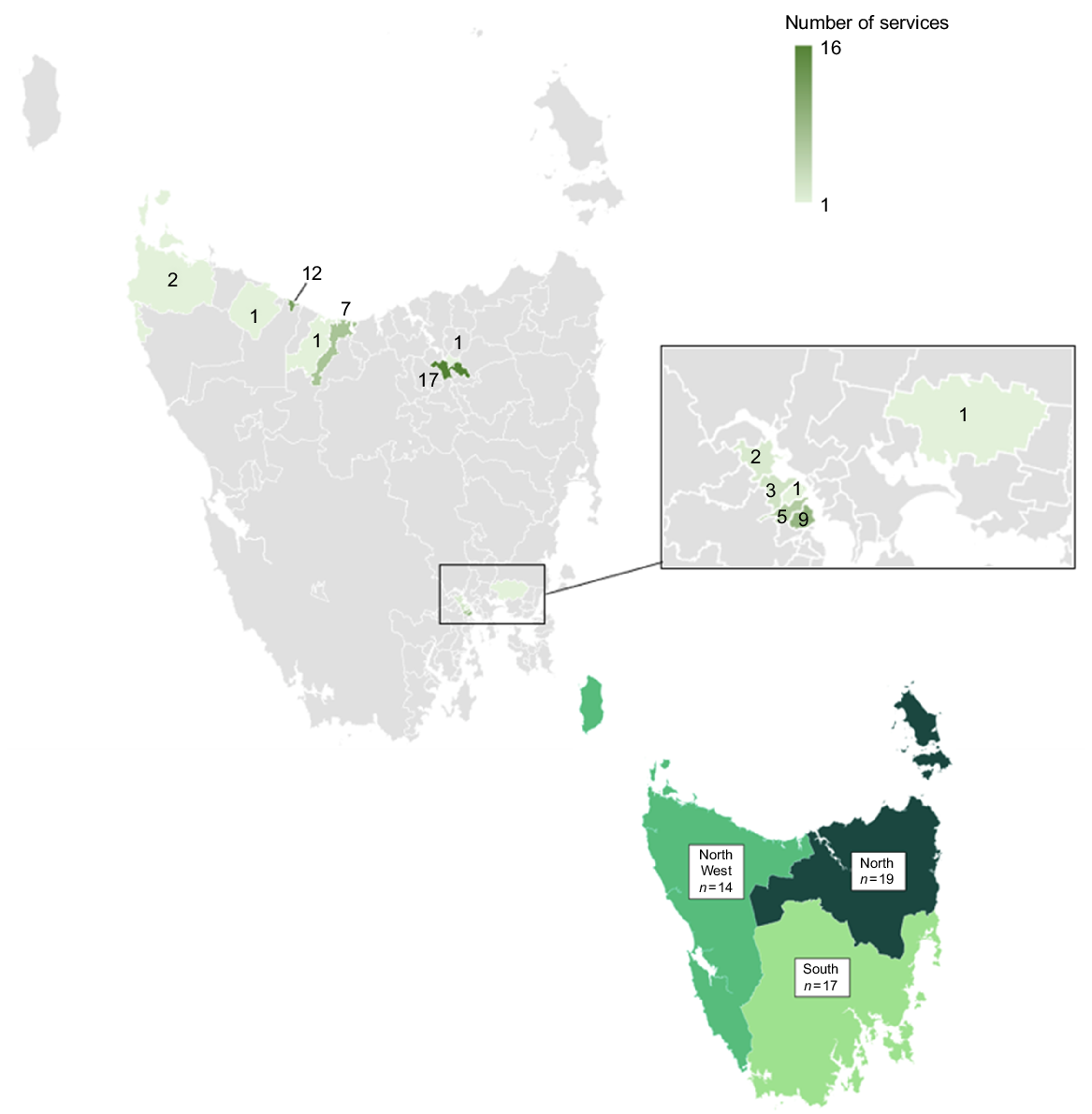
Fig. 2 maps the location of mental health services across the state. The 28 services were located in 13 suburbs across Tasmania, in only 7 out of 29 LGAs. Services were predominantly located in the major city of each service region, including Launceston (n = 17), Burnie (n = 12) and Hobart (n = 9). Only 38% of services were located outside these major cities, in neighbouring metropolitan areas. No services were identified from 22 LGAs where the remaining 32% of young people live, leaving approximately 105,000 young people underserviced. Eight services were available state-wide, eight in the South (i.e. only young people who live in the South are eligible), five in the North, one in the North-West, two in the South and North and four in the North and North-West (n = 27).
Locations of 28 community-based youth mental health services in Tasmania across suburbs (above) and regions (below).
No services had out-of-pocket costs associated for young people, and young people could self-refer to 82% of services. Services were predominantly accessible on weekdays between 9 am to 5 pm (93%, n = 26). At the time of data collection, the majority of services were at full capacity, with 74% not currently accepting any new clients requiring ongoing support, and the average wait-time was 4 months.
Key eligibility criteria across services included age, severity and type of presenting concerns. According to DESDE-LTC classifications, the majority of the 28 services (39%, n = 11) were for children and adolescents (aged 0–18 years), 10 were for adolescents and young adults (aged 12–25 years), six services supported adolescents only (aged 10–18 years) and one was for children (aged 0–10 years). Many services (65%, n = 18) supported young people experiencing any type of mental health concern. The remaining services targeted contextual/psychosocial stressors (e.g. homelessness, school disengagement, n = 5), substance use (n = 3) or those affected by family violence or sexual assault (n = 2). Approximately 50% of services were Tier 2 level support for those with mild to moderate concerns (n = 14) and 32% were Tier 1 early intervention support for emerging or mild symptoms (n = 9). Three services supported young people experiencing moderate to severe concerns (Tier 3) and two provided Tier 4 support to those with the most acute/high-risk needs.
Sixty percent of services (n = 16) were non-mobile/centre-based services. Seven services (25%) provided the option of outreach support within their respective service region. Most services (81%) sought to provide tailored frequency and intensity of support that met each young person’s needs, with significant variation ranging from weekly to monthly. The average duration of support was 6 months; the majority of services were considered short-term or brief intervention. Service provision included therapeutic support (e.g. individual, group or family therapy, n = 21, 75%), and seven services provided case management/service coordination to address broader needs. The majority of services (79%) had a multidisciplinary team (e.g. psychologist, social worker, caseworker).
Gaps in service provision
Three major themes describing key gaps in community-based mental health service access/provision for young people, from the perspective of service providers, were identified: (1) the missing middle; (2) services at capacity; and (3) integrated supports.
Service providers (20/26) identified ‘the missing middle’ as a predominant gap in the community-based youth mental health sector that continues to widen. This refers to the lack of Tier 3 therapeutic and psychosocial support for young people presenting with moderate to severe mental health concerns whose needs are not being met by existing services (i.e. too high-risk for Tier 2, but below the severity threshold for Tier 4 services).
The system is broken. I had a young person who I referred to CAMHS after a hospital presentation for suicidal ideation and other things, but CAMHS deemed them not severe enough. The only other option is headspace, but they were too severe. So we’re left holding them, but it’s a completely inappropriate fit for our service. (Tier 2 service, South)
This was attributed to the increasing contexual complexities exhibited by young people attempting to access support (e.g. multiple diagnoses, homelessness, family violence, etc.), combined with strict service eligbility criteria.
We’ve noticed increased acuity and chronicity probably over the past five years … in addition to multiple mental health comorbidities, there’s also a really long list of situational and environmental factors that are adding complexity. (Tier 4 service, North-West)
The missing middle poses a barrier to providing young people with the most appropriate timely support that meets their needs.
We struggle with a lot of young people that are not at that CAMHS threshold, but are far too complex for us. There’s nowhere else for them … the only step-down might be private psychology but that’s often not appropriate. (Tier 2 service, North)
The majority of providers (24/26) noted increasing demand for their services over the past 5 years, resulting in increased pressure on staff and multiple months-long waiting lists. This highlights the limited availability of services and the under-resourced state of the community sector, which remains exacerbated post COVID-19 pandemic.
The sector is very splintered because so many services, especially NGOs [non-government organisations], have little bits of money, so it’s grossly under-done and under-staffed to keep up with increasing presentations. We only have two workers, so we just haven’t had the increase in resources to meet the increasing need. (Tier 3 service, South)
Providers acknowledged the minimal capacity for outreach as an adverse consequence of a lack of resources (i.e. time, staff), which poses a barrier to service accessibility and engagement for young people outside major cities who may not engage in telehealth or require intensive support.
Because of the lack of clinicians and the more acuity and higher volume of referrals, we have to work within this building alone. Our ability to actually get out into the communities for outreach is significantly limited. Kids are travelling 1–2 hours to attend services. Outreach is missing across the board. (Tier 2, North)
Service providers (21/26) identified key supports that are lacking across the youth community-based mental health sector to provide a more integrated/holistic response, including one-stop-shop models of care, psychosocial support and peer workers.
There are very limited options for referring out. We might refer to 3–4 different services because there’s none that can provide the therapeutic support and the psychosocial support. We shouldn’t be making the young person go to multiple services. (Tier 2, North)
Psychosocial support in general is a missing gap for young people. We have some referral options when someone turns 18, but for children under 18, that’s really lacking. (Tier 1, South)
We need options that are longer than 12 months. Rather than trying to find another service to step-down to, because there’s nothing available or appropriate, the appointments become less frequent, and the young person can remain with that same clinician to keep the continuity, attachment and role modelling going. (Tier 4, South)
Service providers suggested that peer workers could assist in providing psychosocial support to reduce the burden on existing services and better address the underlying contextual needs of young people experiencing mental illness.
Youth peer support workers could fill that space. I think they could definitely be the missing link to that more integrated, practical, wrap-around support that we can’t currently do. (Tier 2, South)
Discussion
This study sought to map and describe community-based mental health services for young people in Tasmania and identify key gaps to inform future service design, development and delivery. A systematic scoping approach was conducted to identify, classify, map and describe services, combined with qualitative data collection with service representatives. A total of 28 services, delivered by 22 service providers, were identified. The number, diversity and capacity of services was significantly less in comparison to other Australian states/territories (Salvador-Carulla et al. 2022). For example, previous service mapping identified 35 services with larger capacity in the ACT, which has a smaller population (Furst et al. 2021). The findings indicate limited accessibility, availability, capacity and diversity of community-based mental health services for Tasmanian youth.
Service accessibility is a key barrier for young people in Tasmania. Despite high need, there are fewer and less diversity of services in the rural North-West service catchment compared to the other regions. Service location does not adequately align with Tasmania’s dispersed population density; services are clustered in the major city of each region, despite a highly dispersed/rural population. Services are not located in rural and remote areas where over 30% of youth live. This is consistent with previous mental health service mapping across rural and remote areas of Australia, Canada and Finland, which identified consistently scarce and fragmented support (van Spijker et al. 2019; Salinas-Perez et al. 2020). Those in rural/regional areas face significant socioeconomic disadvantage, exclusion, systemic barriers to service access/engagement and poorer mental health outcomes (Salinas-Perez et al. 2020). While telehealth has become embedded among many services following the COVID-19 pandemic, the findings highlight the need for greater assertive mobile outreach capacity to better reach young people in their environment, which can increase accessibility, improve engagement and enhance therapeutic gains among youth, specifically for those who may not engage with telehealth or centre-based services (Anderson et al. 2017). The majority of services were at full capacity with long waiting lists, further compromising and delaying young people’s access to support. Youth mental health services internationally are struggling to meet the burden and increasing complexity of presentations with the funding and resourcing available (Samji et al. 2022). Enhancing service accessibility remains an ongoing local and national priority, particularly in rural/regional areas where mental health workforce shortages are more pronounced (van Spijker et al. 2019). Providers suggested that lived-experience youth peer support workers could provide wrap-around support to strengthen the workforce and capacity for support in rural areas. Embedding peer workers into existing clinical mental health services may ensure that this cohort receive the support that they require.
The current findings highlight the ‘missing middle’ in Tasmania’s youth community mental health sector – those who require intensive community support but fall between services available for mild and severe mental health concerns. The majority of Tasmanian services provide early intervention for emerging risk or mild concerns (Tier 1 and Tier 2), while state-wide CAMHS intends to support the most severe, complex and acute mental health presentations (Tier 4), with minimal Tier 3 services. Two thirds of young people engaged in early intervention mental health services do not experience improvements in social and occupational functioning (Iorfino et al. 2022), yet there are limited step-up options to support these outcomes. The need for services to fill this ‘missing middle’ has been identified in previous Australian service mapping across Victoria, New South Wales (NSW) and ACT (Salvador-Carulla et al. 2022). Services providing social and education-related care for youth with mental health concerns are lacking, and have the lowest stability of funding (Furst et al. 2021). This is concerning given high rates of young people aged 15–25 years with mental health concerns not engaged in education and/or employment (Holloway et al. 2018). In acknowledgement of rural mental health workforce shortages, lived-experience peer support workers could complement existing and future mental health services intending to address the missing middle. Particularly in Canada, peer workers have been crucial to the implementation and scale-up of integrated health and social care models of care for young people (i.e. Youth Wellness Hubs in Ontario; Henderson et al. 2023). Stepped-care mental health service provision in Australia is a national priority, so there is an urgent need to enhance integration and continuity of community youth mental health care. Dynamic service models that emphasise integrated and multidisciplinary interventions to provide therapeutic support alongside wrap-around social and occupational support may improve the trajectory of youth experiencing mental illness.
Implications
The current findings inform the following recommendations to enhance the youth community mental health sector.
Address the missing middle – develop new or strengthen existing services to support the therapeutic and psychosocial needs of young people experiencing moderate to severe mental illness.
Focus more on wrap-around psychosocial support to enhance the functioning of young people presenting with multiple contextual and socioeconomic complexities underpinning their mental health.
Develop one-stop-shop models of care (i.e. integration hubs) or better resource existing services by embedding peer workers to provide holistic support, increase continuity of care and support service integration.
Recruit, train and support lived-experience peer workers to provide wrap-around psychosocial support for young people experiencing mental illness, and to strengthen the rural mental health workforce.
Implement new services or scale-up existing services in rural/regional LGAs, or provide assertive outreach and/or telehealth to increase service accessibility.
Increase capacity for after-hours support to enhance service accessibility and flexible service provision.
Increase duration of support (over 12 months) to enhance continuity of care and better address underlying contextual factors.
Provide greater longer-term resourcing/funding for community mental health services.
These recommendations align with key national priority areas from the National Children’s Mental Health and Wellbeing Strategy (Commonwealth of Australia 2021). While service mapping is strongly recommended across all states and territories to identify specific local gaps, insofar as there are similar gaps, these implications may also broadly inform community mental health across Australia to enhance national youth mental health service provision.
Limitations
The current study provided specific insight and recommendations for Tasmanian community mental health. While focused on the local context of one Australian state, the key findings and gaps, including the ‘missing middle’, lack of rural/regional supports and limited service capacity, have been identified locally and internationally (Anderson et al. 2017). The use of the DESDE-LTC as a standardised classification system is a strength of this study that enables future comparisons to other areas across Australia and internationally. A key limitation is that this study did not include ‘adult’ services, and hence does not provide the full scope of services that young adults aged 18–25 years may access. Another significant limitation is that services were mapped against the population of young people without an estimation of current disorder prevalence across the state. Furthermore, this study focused on community-based mental health services only, so private providers (i.e. services requiring private insurance or out-of-pocket payment), generic services (e.g. GPs) and emergency or inpatient acute/hospital-based services have not been mapped. These services have been excluded in previous large-scale service mapping studies as it is considered necessary to take stock of the community sector separately. Nonetheless, as strong mental health systems require synergy, integration and navigation across all areas, it is recommended that the services not within the scope of the current paper are also mapped and then compared using the same classification via an integrated mental health atlas to improve understanding of the local youth mental health system.
Conclusion
This study utilised a systematic mapping approach to identify, classify and describe the availability of communtiy mental health services for youth in Tasmania. The findings highlight the urgent need to address the ‘missing middle’, provide more holistic psychosocial supports, implement assertive outreach and integrated models of care and increase service accessibility. The current findings will be used to inform future service planning, design and development to address the identified gaps. Systematic service mapping should be conducted across all regions to inform mental healthcare policy, planning and implementation to enhance outcomes for youth.
Data availability
The data that support this study can be accessed upon request from the corresponding author.
Declaration of funding
Ms Savaglio is funded by a National Health and Medical Research Council Postgraduate Scholarship for Public Health and Health Services Research (2014147).
References
ABS (2018) National health survey: first results, 2017-18: Tasmania; Table 3.1 Long-term health conditions, Proportion of persons. Australian Bureau of Statistics, Canberra. Available at https://www.abs.gov.au/statistics/health/health-conditions-and-risks/national-health-survey-state-and-territory-findings/latest-release#data-download [Verified 18 April 2023]
ABS (2022) National study of mental health and wellbeing. Australian Bureau of Statistics, Canberra. Available at https://www.abs.gov.au/statistics/health/mental-health/national-study-mental-health-and-wellbeing/latest-release [Verified 18 April 2023]
AIHW (2021) Australia’s youth: mental illness. Australian Institute of Health and Welfare, Canberra. Available at https://www.aihw.gov.au/reports/children-youth/mental-illness [Verified 18 April 2023]
Anderson JK, Howarth E, Vainre M, Jones PB, Humphrey A (2017) A scoping literature review of service-level barriers for access and engagement with mental health services for children and young people. Children and Youth Services Review 77, 164-176.
| Crossref | Google Scholar |
Braun V, Clarke V (2006) Using thematic analysis in psychology. Qualitative Research in Psychology 3(2), 77-101.
| Crossref | Google Scholar |
Caspi A, Houts RM, Ambler A, et al. (2020) Longitudinal assessment of mental health disorders and comorbidities across 4 decades among participants in the Dunedin birth cohort study. JAMA Network Open 3(4), e203221.
| Crossref | Google Scholar |
CCYP (2018) The health and wellbeing of Tasmania’s children and young people report. Commissioner for Children and Young People, Tasmania. Available at https://www.childcomm.tas.gov.au/wp-content/uploads/2018/08/The-Health-and-Wellbeing-of-Tasmanias-Children-and-Young-People-Report-2018.pdf [Verified 18 April 2023]
Commonwealth of Australia (2021) The national children’s mental health and wellbeing strategy. Commonwealth of Australia, Canberra. Available at https://www.mentalhealthcommission.gov.au/getmedia/9f2d5e51-dfe0-4ac5-b06a-97dbba252e53/National-children-s-Mental-Health-and-Wellbeing-Strategy-FULL [Verified 18 April 2023]
Department of Health (2020) Government response to the CAMHS review and recommendations. Department of Health, Tasmania. Available at https://www.health.tas.gov.au/sites/default/files/2022-02/Government%20Response%20to%20the%20CAMHS%20Review%20Report.pdf [Verified 18 April 2023]
Gossip K, Pagliaro C, Comben C, Fjeldsoe K, Whiteford H, Diminic S (2023) Using the national mental health service planning framework to inform integrated regional planning: a case study in Tasmania, Australia. International Journal of Mental Health Systems 17, 23.
| Crossref | Google Scholar |
Henderson JL, Chiodo D, Varatharasan N, et al. (2023) Youth wellness hubs Ontario: development and initial implementation of integrated youth services in Ontario, Canada. Early Intervention in Psychiatry 17(1), 107-114.
| Crossref | Google Scholar | PubMed |
Holloway EM, Rickwood D, Rehm IC, Meyer D, Griffiths S, Telford N (2018) Non-participation in education, employment, and training among young people accessing youth mental health services: demographic and clinical correlates. Advances in Mental Health 16(1), 19-32.
| Crossref | Google Scholar |
Iorfino F, Carpenter JS, Cross SPM, et al. (2022) Social and occupational outcomes for young people who attend early intervention mental health services: a longitudinal study. Medical Journal of Australia 216(2), 87-93.
| Crossref | Google Scholar | PubMed |
MHC (2021) Youth mental health services: state-wide consultation report. (Mental Health Council: Tasmania) Available at https://mhct.org/wp-content/uploads/2022/02/MHCT-Youth-MH-Services-Report-2021.pdf [Verified 18 April 2023]
PHT (2020) Rethink 2020: a state plan for mental health in Tasmania 2020-2025. Primary Health Tasmania, Tasmania. Available at https://www.health.tas.gov.au/sites/default/files/2021-12/Rethink_2020_state_plan_2020-25_DoHTasmania.pdf [Verified 18 April 2023]
Romero-López-Alberca C, Gutiérrez-Colosía MR, Salinas-Pérez JA, et al. (2019) Standardised description of health and social care: a systematic review of use of the ESMS/DESDE (European Service Mapping Schedule/Description and Evaluation of Services and DirectoriEs). European Psychiatry 61, 97-110.
| Crossref | Google Scholar | PubMed |
Salinas-Perez JA, Gutierrez-Colosia MR, Furst MA, et al. (2020) Patterns of mental health care in remote areas: Kimberley (Australia), Nunavik (Canada), and Lapland (Finland): Modèles de soins de santé mentale dans les régions éloignées: Kimberley (Australie), Nunavik (Canada) et Laponie (Finlande). The Canadian Journal of Psychiatry 65(10), 721-730.
| Crossref | Google Scholar | PubMed |
Salvador-Carulla L, Alvarez-Galvez J, Romero C, et al. (2013) Evaluation of an integrated system for classification, assessment and comparison of services for long-term care in Europe: the eDESDE-LTC study. BMC Health Services Research 13, 218.
| Crossref | Google Scholar |
Salvador-Carulla L, Furst MA, Tabatabaei-Jafari H, et al. (2022) Patterns of service provision in child and adolescent mental health care in Australia. Journal of Child Health Care 1, 1-15.
| Crossref | Google Scholar |
Samji H, Wu J, Ladak A, et al. (2022) Review: mental health impacts of the COVID-19 pandemic on children and youth – a systematic review. Child and Adolescent Mental Health 27(2), 173-189.
| Crossref | Google Scholar | PubMed |
State Growth Tasmania (2022) Tasmania service age groups. State Growth Tasmania, Tasmania. Available at https://profile.id.com.au/tasmania/service-age-groups [Verified 18 April 2023]
Tong A, Sainsbury P, Craig J (2007) Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care 19, 349-357.
| Crossref | Google Scholar | PubMed |
van Spijker BA, Salinas-Perez JA, Mendoza J, et al. (2019) Service availability and capacity in rural mental health in Australia: analysing gaps using an integrated mental health atlas. Australian & New Zealand Journal of Psychiatry 53(10), 1000-1012.
| Crossref | Google Scholar | PubMed |